ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
Author: Sandra Schneider, MD, FACEP, Associate Executive Director for Clinical Affairs, American College of Emergency Physicians
It has long been known that during a pandemic or major disaster that a shortage of ventilators and other life-sustaining devices could occur. The triaging of ventilators should occur only when the hospital, region, or nation is operating in crisis mode. Ideally, planning for such an event should take place in advance and involve hospital personnel, the ethics committee, and even members of the public. Preplanning mitigates the enormity of the decision that must be made by the physician caring for the patient.
As ventilators become scarce, attempts should be made to increase the number of devices available. The Federal Government is working with industries to produce more units; however, it is clear that this solution will take time. In the meantime, hospitals should create a communication system or dashboard to locate available units within the region. Ventilators used on animals are identical to those for humans, so veterinarian options should be explored.
It is possible to ventilate more than one patient (i.e., up to four patients) with a single ventilator. While the Society of Critical Care Medicine opposed this option in the “Consensus Statement on Multiple Patients Per Ventilator,” other agencies offer this as an option, including the:
In other countries faced with a ventilator shortage, guidelines for intubation were based on projected survival from COVID-19. These guidelines take into account the patient's age and comorbidities as well as the survival data from China.
Perhaps the best plan on ventilator allocation open to the public is New York State’s “Ventilator Allocation Guidelines.”
Other documents discuss ventilator allocation over a larger geographic region, including the:
It is difficult, if not impossible, to have all the necessary facts at hand when making the decision regarding intubation and ventilator use. Most scoring systems are based on the sequential organ failure assessment (SOFA) score, which is unavailable in the emergency department. The New York guidelines suggest that the following patients are excluded from ventilator support and, depending on the scarcity of ventilators, are not candidates for intubation (see the “Ventilator Allocation Guidelines” for further details).
Exclusion criteria:
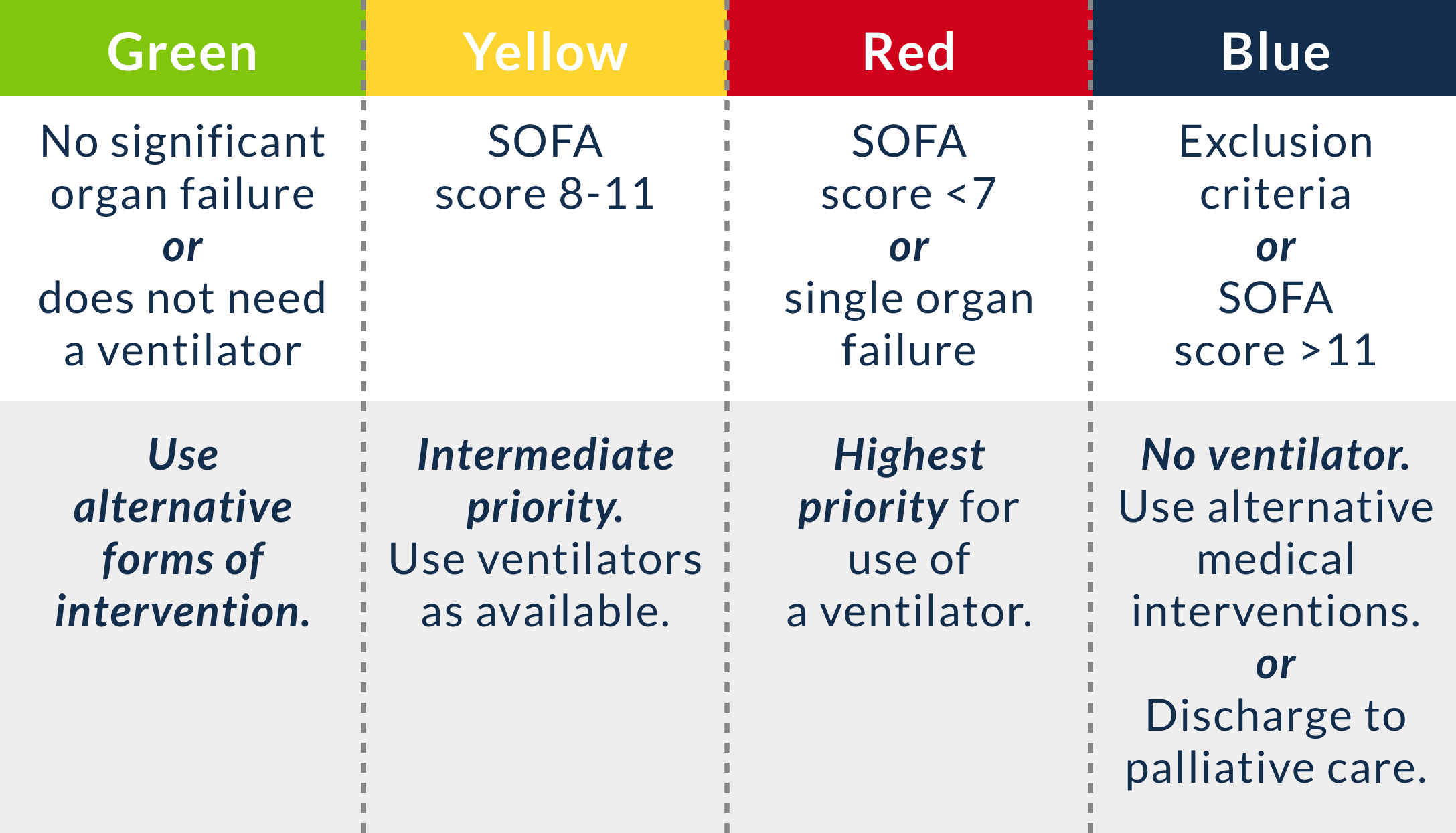
Given enough time for information gathering, the New York guidelines also rely on the SOFA score, which assigns a color code of priority for ventilators (Figure 10.2):
For more information, refer to MDCALS’s SOFA score calculator.
Figure 10.2 Color-coded SOFA scoring system.
Patients are reassessed at 48 hours and periodically over time; the plan has additional information for decisions at these points in time.
Other plans exist or are modified from the New York guidelines. It is essential that a plan be in place to assist the physicians who must make these difficult decisions in the emergency department and ICU.