Authors: Edward H. Suh, MD†; Liliya Abrukin, MD, MPH†; David Bodnar, MD‡; Gerardo Chiricolo, MD§; Johnathon LeBaron, DO||; Laura Melville, MD, MS§; Peter A. D. Steel, MA, MBBS‡; Brenna M. Farmer, MD, MBA, MS‡; Nicholas Gavin, MD, MBA, MS†; Marie-Laure Romney, MD, MBA†; Manish Sharma, DO, MBA||; Amos J. Shemesh, MD‡
† Department of Emergency Medicine, NewYork-Presbyterian Hospital/Columbia University Irving Medical Center
‡ Department of Emergency Medicine, NewYork-Presbyterian Hospital/Weill Cornell Medical Center and Lower Manhattan Hospital
§ Department of Emergency Medicine, NewYork-Presbyterian Hospital/Brooklyn Methodist Hospital
|| Department of Emergency Medicine, NewYork-Presbyterian Hospital Queens
Acknowledgment: Thank you to Dr. Angela Mills, Dr. Rahul Sharma, and the NewYork-Presbyterian Hospital leaders for their support in developing these guidelines.
Editors’ note: The NewYork-Presbyterian pathway differs in some minor ways from other recommendations in the ACEP COVID-19 Field Guide. This variation points out the importance of using current resources, using clinical judgment, and individualizing care. The items in this pathway are also potentially useful when evaluating patients with other respiratory infections, particularly during pandemics and other times of system saturation.
NewYork-Presbyterian COVID-19 evaluation pathway
- This evaluation pathway was developed through an iterative process, with input from leadership and academic representatives across the campuses of the NewYork-Presbyterian Hospital System during the initial COVID-19 surge.
- The group was able to incorporate real-time feedback from their different institutions, which was critically important because several institutions experienced surges earlier than others. This protocol reflects the clear need at that time to create a safe outpatient follow-up pathway for patients who would ordinarily be treated as inpatients. Adjustment may be necessary based on the resources available at each facility.
- The pathways outlined in this guideline reflect the best evidence available at the time, with some modification based on newer evidence, including the continually updated ACEP ED COVID-19 Management Tool.
- The use of risk prognostication tools, such as the Pandemic Respiratory Infection Emergency System Triage (PRIEST) score, can aid in clinical decision-making and can provide a probability of adverse outcomes at 30 days; scores greater than 4 predict adverse outcomes with high sensitivity. However, no large prospective validation studies of any COVID-19 risk stratification scores have been done.
- Access to outpatient pulse oximeters and oxygen concentrators and close telehealth follow-up services are crucial to safely discharging moderate-risk cohorts.
- In addition, moderate-risk patients must have the following if they are to be discharged:
- An observation period in the emergency department to ensure initial stability;
- Assistance at home to limit exertion and facilitate calling 911 if any worsening of clinical status occurs;
- A working phone number or internet with video capability (the latter is strongly preferred for visual telehealth follow-up services); and
- The ability to use a pulse oximeter (with an oxygen concentrator, for those who need it).
- These guidelines do not replace clinical judgment, but rather serve to inform clinicians across a broad spectrum of training to risk stratify patients with COVID-19 when resources are overwhelmed.
COVID-19 screening laboratory evaluation
COVID-19 screening laboratories differ by site, but tests may include:
- CBC with differential
- Lymphopenia may be present.*
- Thrombocytopenia may be present.*
- Complete metabolic panel
- Renal insufficiency may be present.*
- Transaminitis may be present.*
- SARS-CoV-2 polymerase chain reaction test
- Procalcitonin
- Blood cultures
- Sputum cultures
- Urine cultures
- Urinalysis
- Venous blood gas
- Lactate dehydrogenase*
- Creatine kinase*
- Troponin or high-sensitivity troponin*
- Ferritin*
- C-reactive protein*
- PT/INR
- PTT
- D-dimer*
* Abnormal findings can be used for risk stratification as part of the overall clinical picture.
COVID-19 screening imaging
In general, imaging is not required for screening, particularly in low-risk patients.
- Chest x-ray
- Portable may be preferred for infection control purposes.
- Chest CT
- Not a preferred method for diagnosis because of infection control measures required between patients and current testing availability.
Evaluation pathway (by risk group)
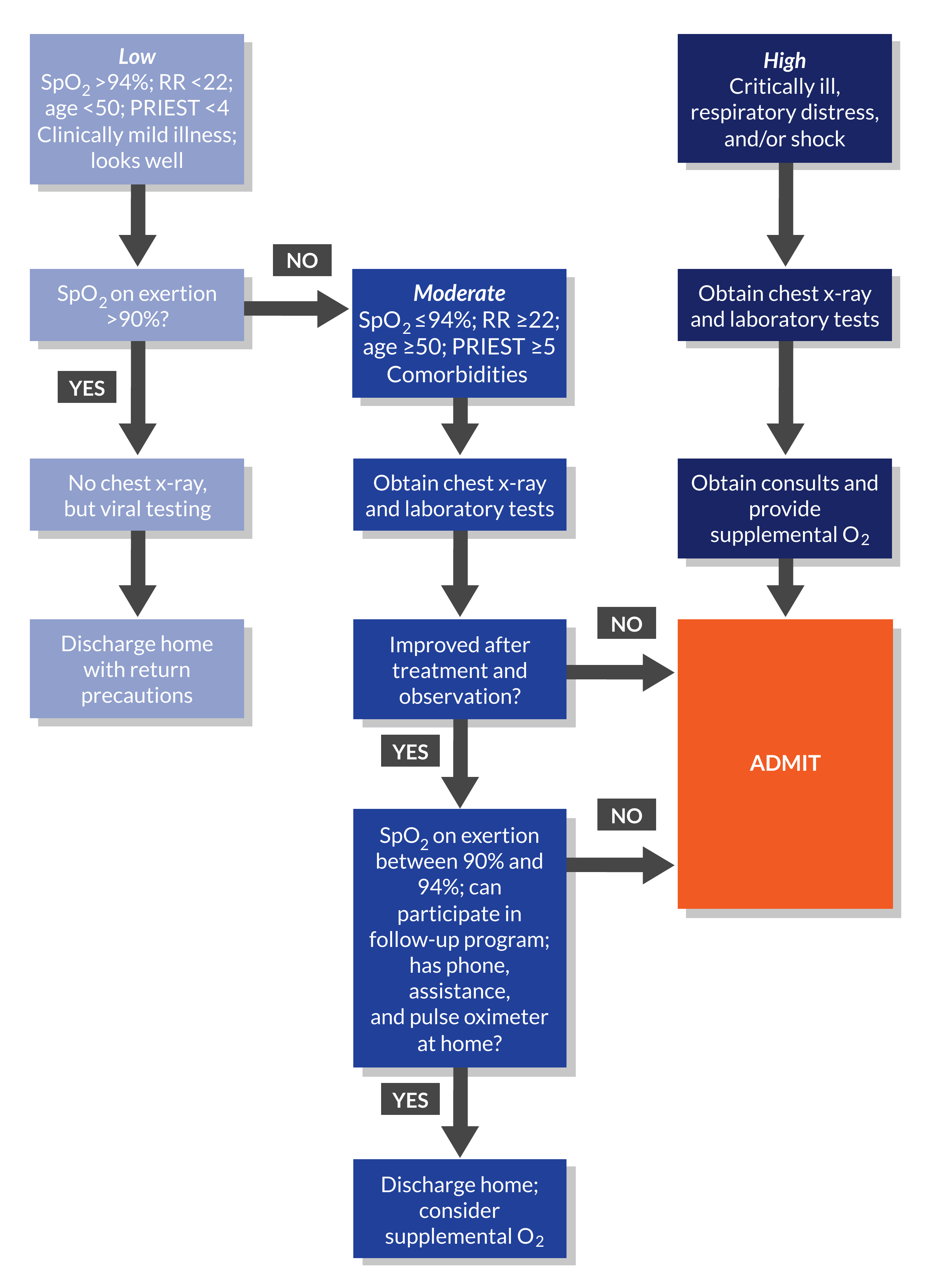
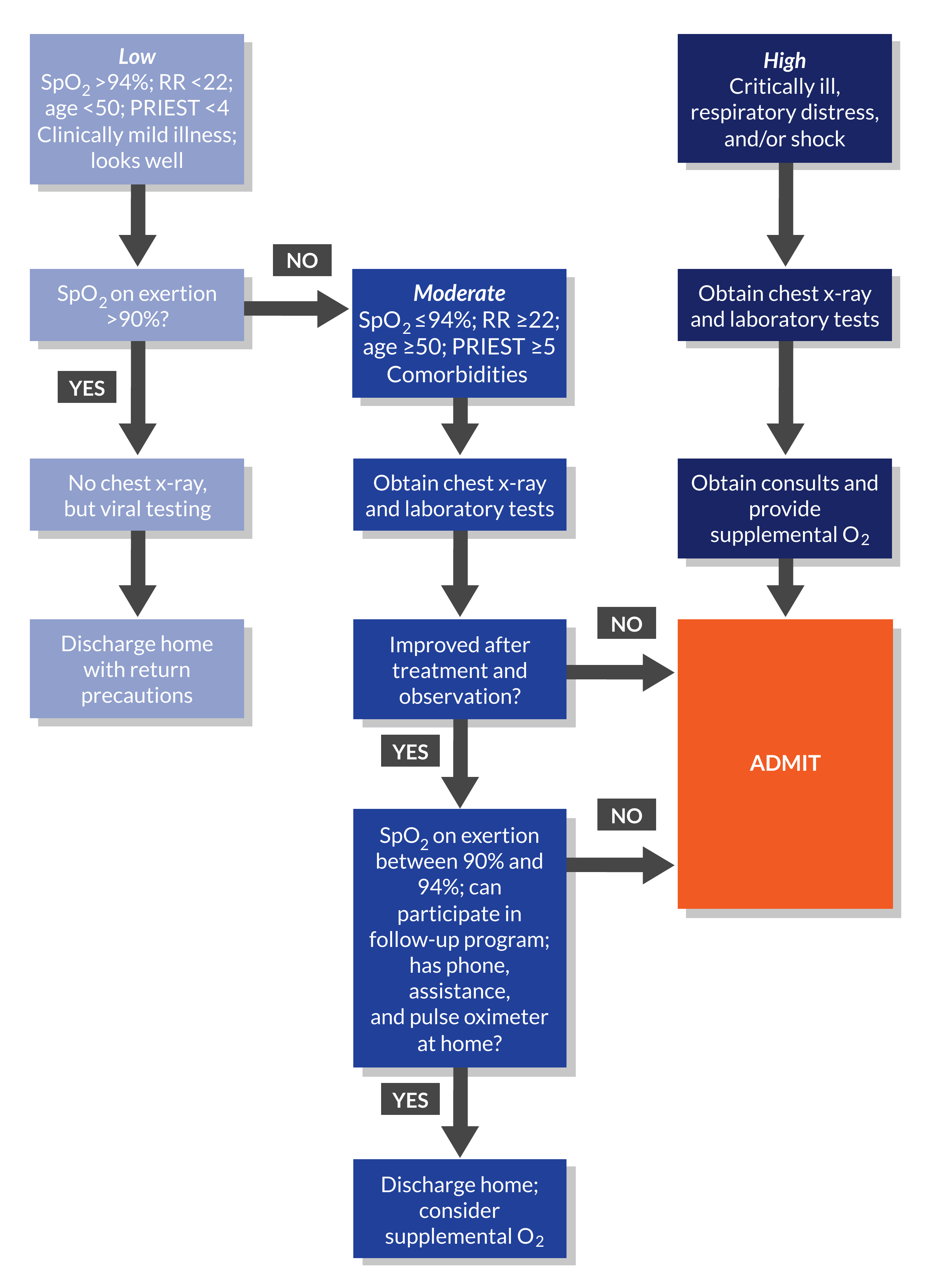
The ACEP ED COVID-19 Management Tool is recommended as the most comprehensive evidence-based tool available to determine risk prognostication and severity and for management recommendations (Figure 11.1).
Low risk of adverse outcomes
Includes patients with clinically mild illness with normal vital signs, including an SpO2 level >94% and a respiratory rate <22 breaths/min; age <50 years; and a PRIEST score less than 4.
- Obtain an exertional oxygen saturation reading. If the reading is >90% after 1 minute of walking in place at the bedside:
- No routine chest x-ray is needed, unless for another indication.
- Viral testing should be obtained to allow for appropriate prescribing of readily available outpatient medications, particularly for patients at high risk of disease progression. Outpatient medications include nirmatrelvir with ritonavir, remdesivir infusions, and molnupiravir.
- If the patient has exertional oxygen desaturations <90%, moderate-risk evaluation should occur.
Moderate risk of adverse outcomes
Includes patients with (1) oxygen saturations between 90% and 94% and respiratory rate ≥22 breaths/min; (2) age ≥50 years and comorbidities; or (3) a PRIEST score of 5 or greater. Comorbidities or conditions that can place patients at moderate risk of adverse outcomes include:
- Hypertension
- COPD
- Diabetes
- Obesity
- Cardiovascular disease
- Lung disease
- Cancer
- Immunosuppression
- Renal disease
In moderate-risk patients, obtain laboratory tests and imaging as clinically indicated, including laboratory studies (mentioned above) based on infectious disease and hospital epidemiology input to aid in risk stratification. Chest x-ray commonly shows bilateral opacities in moderate-risk patients. Many of these patients will need to be admitted.
After a period of observation, if there is no indication for admission, the following should be available to patients before discharge:
- At least a working telephone at their home, although internet with video capability for telehealth is preferred;
- Assistance at home to limit the patient’s exertion levels;
- A follow-up program for monitoring either with a primary care physician seen in person (if available) or through telehealth visits for monitoring (if available); and
- A pulse oximeter and supplemental oxygen (the latter if indicated). Supplemental oxygen is indicated at discharge if exertional oxygen saturation is between 90% and 92%.
If these items or conditions cannot be met at home, then moderate-risk patients should be admitted to the hospital.
High risk of adverse outcomes
Includes patients who are critically ill; in respiratory distress; with significant tachypnea, work of breathing, or hypoxia; in shock; or with evidence of clinical deterioration while in the emergency department.
- Obtain laboratory tests and imaging.
- Consult critical care.
- Consult infectious disease, if needed, for appropriate medication management with remdesivir or other immunotherapies such as baricitinib or tocilizumab.
- Utilize supplemental oxygen via a nonrebreather mask, nasal cannula, or both.
- If a negative pressure room is available, start high-flow nasal cannula or BiPAP therapy, as indicated.
- Intubate the patient if they are not stabilized by noninvasive respiratory support.
- Alert the airway team, if appropriate.
- Admit the patient to a step-down unit or CCU.
Figure 11.1 Evaluation pathway for patients with suspected COVID-19. Credit: ACEP.



COVID-19 Severity Classification
ACEP COVID-19 Severity Classification Tool contributors: Brian Fengler, MD, Cofounder and Chief Medical Officer, EvidenceCare; Sandy Schneider, MD, FACEP, Associate Executive Director, ACEP; Amy Baxter, MD, Chief Executive Officer, Pain Care Labs, Clinical Associate Professor at Augusta University; Brenna Farmer, MD, MBA, MS, Site Director, NewYork-Presbyterian Hospital Lower Manhattan Hospital Emergency Department, Director of Patient Safety, NewYork-Presbyterian/Weill Cornell Medical Center, Associate Professor of Clinical Emergency Medicine; Phil Parker, MD, GMO SCP-Health, SCP-Health; Jonathan A. Handler, MD, Adjunct Associate Professor, Northwestern University Feinberg School of Medicine, Department of Emergency Medicine; Peter A. D. Steel, MA, MBBS, Director of Clinical Services, NewYork-Presbyterian/Weill Cornell Medicine Department of Emergency Medicine; Amos J. Shemesh, MD, Assistant Director of Clinical Services, NewYork-Presbyterian/Weill Cornell Medical Center; Pawan Goyal, MD, MHA, FAMIA, Associate Executive Director, Quality, ACEP; Sharon Hibay, DNP, RN, Chief Clinical Officer, Arch Systems, LLC; Christopher Corbit, MD, FACEP, Facility Medical Director, Summerville Medical Center; Tamara Moores Todd, MD; Todd B. Taylor, MD, FACEP, Clinical Informaticist, Independent Consultant; Andrew S. Kanter, MD, MPH, FACMI, FAMIA, Chief Medical Officer, Intelligent Medical Objects; Edward H. Suh, MD, Assistant Professor of Emergency Medicine, Columbia University Medical Center
ACEP and EvidenceCare created a seven-step triage tool for emergency physicians to better classify COVID-19 patients and be informed of next steps. The tool classifies patients on a range from mild or low risk to critical based on seven categories of measurement: vital signs, a quick COVID-19 Severity Index (qCSI) calculator, symptoms and risk factors, discharge home criteria, diagnostic testing and suggested laboratory studies, imaging and laboratory results, and disposition.
The COVID-19 Severity Classification Tool can be accessed through ACEP’s web page. An integrated version is also available for Epic, Cerner, and T-Systems. Hospitals can contact info@evidence.care for more information.
Additional readings
- COVID-19 ED management tool now available, updated. American College of Emergency Physicians. Published September 12, 2023.
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020 May;46(5):854-887. doi: 10.1007/s00134-020-06022-5
- Shi Y, Yu X, Zhao H, et al. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020 Mar 18;24(1):108. doi: 10.1186/s13054-020-2833-7
- Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020 May;94:91-95. doi: 10.1016/j.ijid.2020.03.017
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3
- Beeching NJ, Flectcher TE, Fowler R. Coronavirus disease 2019 (COVID-19). BMJ Best Practice. Last updated January 12, 2024.
- Carpenter CR, Mudd PA, West CP, et al. Diagnosing COVID‐19 in the emergency department: a scoping review of clinical examinations, laboratory tests, imaging accuracy, and biases. Acad Emerg Med. 2020 Aug; 27(8):654-670. doi: 10.1111/acem.14048
- Goodacre S, Thomas B, Sutton L, et al. Derivation and validation of a clinical severity score for acutely ill adults with suspected COVID-19: the PRIEST observational cohort study. PLoS ONE. 2021 Jan 22;16(1):e0245840. doi: 10.1371/journal.pone.0245840
- Suh EH, Lang KJ, Zerihun LM. Modified PRIEST score for identification of very low-risk COVID patients. Am J Emerg Med. 2021 Sep;47:213-216. doi: 10.1016/j.ajem.2021.04.063