ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
Contributor: David McKenzie, Reimbursement Director, American College of Emergency Physicians
Last updated August 2023
Medicare
For in-person evaluation and management (E/M) services conducted in the emergency department, emergency physicians can use the five emergency department E/M codes (Current Procedural Terminology [CPT] codes 99281-99825). Medicare and Medicaid cover emergency telehealth services, but Medicaid reimbursement for telehealth varies by state. For Medicare, the following is the official guidance, even with the COVID-19 public health emergency (PHE) having ended on May 11, 2023:
Table 14.1 shows which telehealth flexibilities expired at the end of the COVID-19 PHE and which ones follow a different timeline. Overall, even after the end of the PHE, emergency department E/M, critical care, and some observation services can be provided through telehealth for Medicare beneficiaries through the end of 2023 (these flexibilities may be extended). Once those codes are removed from the list, emergency physicians won’t be able to bill for those services any longer; however, they can still bill office and outpatient E/M codes for telehealth, which are permanently on the list of approved telehealth services.
Although emergency physicians can continue billing emergency department E/M, critical care, and some observation services as telehealth services through at least December 31, 2023, their ability to provide these emergency telehealth services will be limited going forward. The 2024 Medicare Physician Fee Schedule that is expected to be released in early November 2023 may provide more details about telehealth coverage in 2024 and beyond.
Table 14.1. Status of telehealth services for emergency medicine as of August 2023. Credit: ACEP.
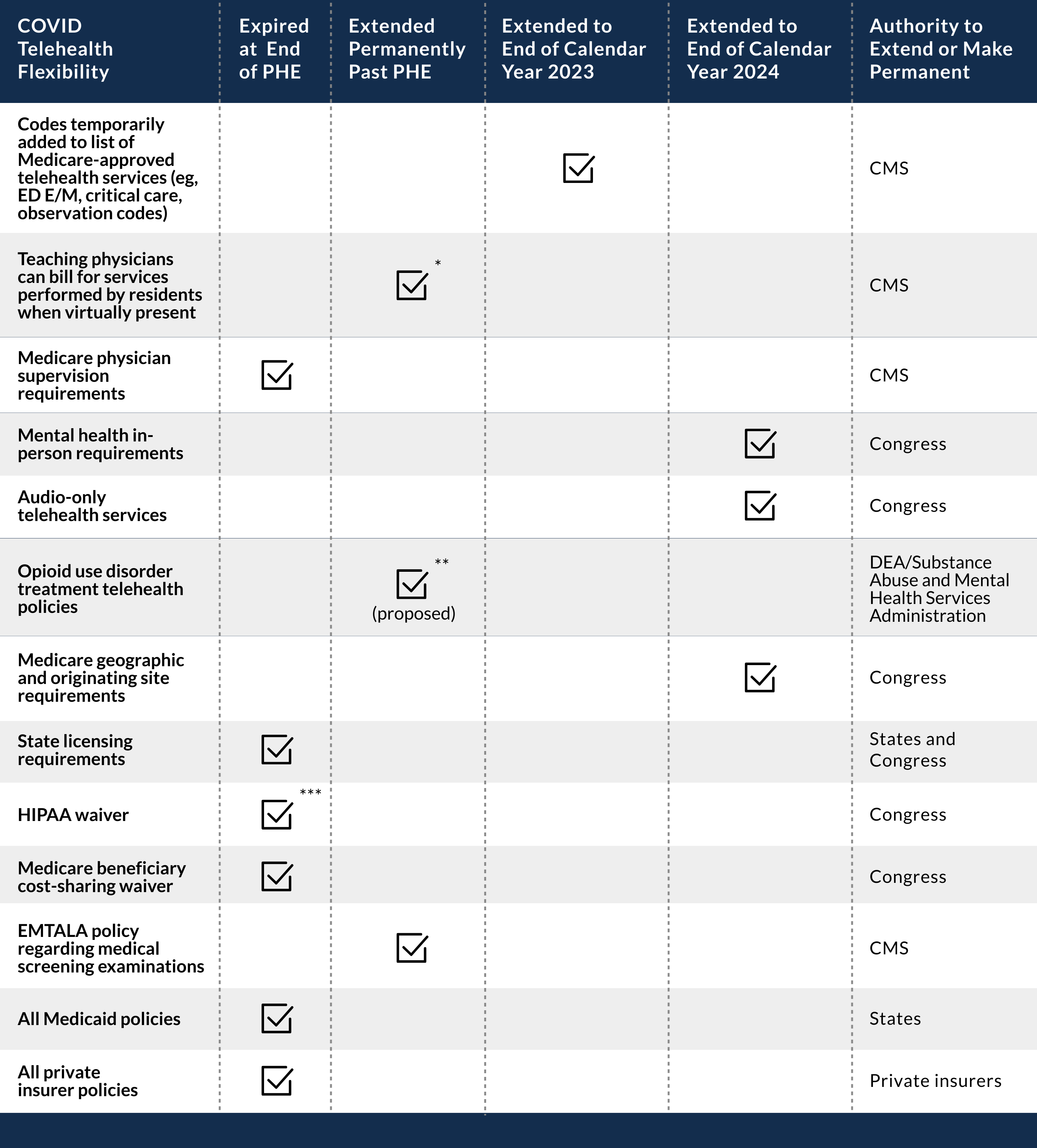
* Extended permanently only in rural areas
** Proposed for opioid treatment programs and for buprenorphine prescriptions. On May 9, 2023, however, the Drug Enforcement Administration (DEA) announced that as it considers permanent expansions, it will extend the current flexibilities for 6 months through November 11, 2023.
*** Department of Health and Human Services announced that it was extending its enforcement discretion, and it continued to not impose penalties on practitioners who used non–HIPAA-compliant telehealth technology (eg, Skype and Facetime) for 90 days after the PHE ended (ie, August 9, 2023).
Medicaid
Now that the PHE has ended, there is significant concern that millions of people will lose their Medicaid and Children’s Health Insurance Program (CHIP) coverage. To ensure that lower-income Americans received the care they needed during the pandemic, Congress, through the Families First Coronavirus Response Act (FFCRA), provided additional federal support to states that expanded and were able to maintain their Medicaid and CHIP rolls. Nearly all states took advantage of this increased 6.2% Federal Medical Assistance Percentage (FMAP) in some form, leading to a significant increase in overall Medicaid enrollment.
Once the higher FMAP goes away, states will become responsible for more of the care costs for this population. States, undoubtedly, will need to reevaluate who will remain eligible for Medicaid as they “unwind” from the PHE and go back to traditional Medicaid and CHIP operations and funding levels. To help states with this unwinding process and to ensure that there is a reasonable process in place for reassessing Medicaid eligibility, CMS issued guidance to states that specifically lays out a 12-month time frame for making these eligibility re-determinations. CMS is hopeful that some of the people cut from Medicaid will be able to enroll in the Affordable Care Act insurance plans.
Congress allowed states to phase down the higher FMAP through the end of the year. That means that some patients who are currently on Medicaid could lose that coverage sometime in 2023.
Testing
H.R. 6201, the FFCRA signed by President Trump on March 18, 2020, made testing for COVID-19 universally free (no cost sharing) for most Americans, even those who are uninsured.
Coverage rules for COVID-19 vaccines and therapeutics
At-home tests, testing-related services, and COVID-19 treatments are no longer covered under the exceptions in place during the PHE and are generally treated as regular forms of care, which means Medicare, Medicaid, and many privately insured patients will have coinsurance and deductible requirements (Medicaid rules vary by state) for COVID-19–related care. Privately insured patients will generally have higher fees for out-of-network care. Uninsured patients will have to pay for testing, care, and vaccinations. The good news is that patients with any type of insurance should continue to have their vaccinations covered at no cost, since vaccinations are considered a preventative service that must be covered without cost sharing, at least for the time being.
With respect to Medicare reimbursement, CMS had been paying clinicians for administering the COVID-19 vaccines at $40 per dose since 2021. This payment rate will continue through the end of 2023 and, starting in 2024, will drop to $30 per dose. CMS will also continue the additional payment of $35.50 for COVID-19 vaccine administration in the home under certain circumstances through the end of 2023. Finally, CMS will pay for COVID-19 monoclonal antibodies through 2023 as well. CMS has been reimbursing $450 for administering a COVID-19 monoclonal antibody therapy in a health care setting and $750 for administering these therapies in homes. Starting January 1, 2024, CMS will pay physicians who administer COVID-19 monoclonal antibody products at the same rate as it does for administering other complex biologic products.
Vaccines
The American Medical Association (AMA) CPT Editorial Panel expedited the creation of new codes for COVID-19 vaccines during the pandemic. These codes can be found in the 2023 CPT code set in the front of the Medicine Section. The codes range from 0001A to 0112A but may be out of numerical sequence. Codes selected for each vaccine vary by the specific immunization and dose (first, second, booster) given. An example of COVID-19 immunization administration appears below:
#● 0071A immunization administration by intramuscular injection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (COVID-19) vaccine, mRNA, lipid nanoparticle, spike protein preservative-free 10 µg/0.2 mL dosage, diluent reconstituted, tris-sucrose formulation, first dose
For more information on vaccine coding and nomenclature, see AMA’s “COVID-19 CPT vaccine and immunization codes.”