Overview
Posterior tibial nerve (PTN) blocks provide analgesia to the calcaneus and the majority of the plantar surface of the foot, areas that are difficult to anesthetize with local infiltration.1-4
PTN blocks alone don’t provide adequate anesthesia for ankle fractures but can be used with other regional blocks.
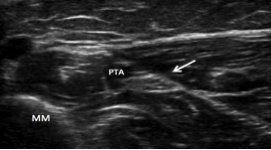
PTN blocks can be performed using landmark-based or ultrasound-guided techniques. The use of ultrasound has been shown to improve the success of sensory block.5