Overview
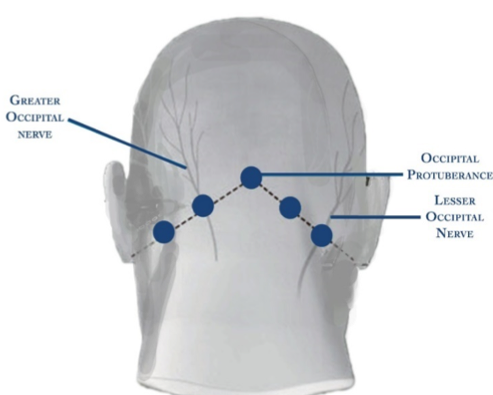
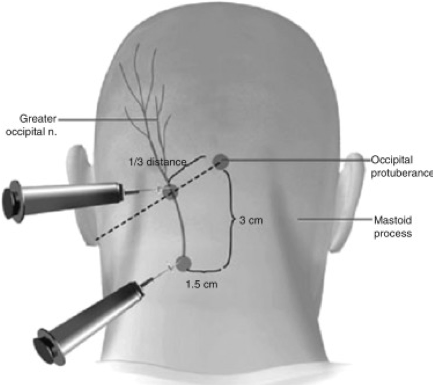
The greater and lesser occipital nerves originate from the neck and provide sensory input to either side of the scalp. They lack motor function. Occipital nerve blocks involve the injection of local anesthetic, with or without steroids, to inhibit the activity of these nerves in the following evidence-supported conditions. Figure 1