Place a local skin wheal of anesthetic just adjacent to the probe in transverse orientation.
- For a median nerve block, place the skin wheal on either side of the probe, depending on hand dominance.
- For a radial nerve block, place the skin wheal on the lateral (radial) side of the probe to avoid puncture of the radial artery.
- For an ulnar nerve block, place the skin wheal on the medial (ulnar) side of the probe to avoid puncture of the ulnar artery.
Place a sterile cover over the ultrasound probe and apply sterile gel.
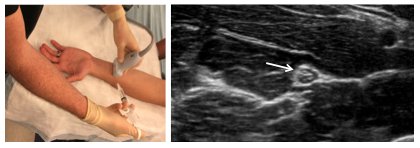
With a spinal needle attached to the anesthetic syringe, enter the skin 1 cm adjacent to the probe with the needle bevel up. Entry of the needle should generally be at a 45-degree angle.
To best visualize the needle tip, keep the probe in a transverse orientation and use an in-plane technique.
Advance the needle slowly, and aim toward the dorsal aspect of the hyperechoic (bright) nerve. Stay at least 1 cm from the nerve to avoid puncture.
Slowly inject 2 to 3 mL of anesthetic to confirm location. Anesthetic will have a hypoechoic (dark) appearance. If patient feels a sharp electric type pain with injection remove needle slightly and re-inject. Patient should feel pressure but not electric shooting pain.
Using V-shaped redirections of the needle, inject 2 to 5 mL of anesthetic per each nerve over the palmar and dorsal aspects of the nerve. The needle should not penetrate the nerve at any point.
- Full circumferential spread of anesthetic around the nerve is ideal but not required.
Visualize injection of the anesthetic at all times.
- If the injection cannot be visualized, stop the procedure.
The patient should start to experience pain relief within 15 minutes and full blockade after 30 minutes. The duration of the block should be 3 to 8 hours, depending on the anesthetic used.