ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
Contributed by: Dr. Shoshana Taube, MD
As soon as monkeypox is suspected, health department personnel should consult their state health department or the CDC Emergency Operations Center (770-488-7100). For initial laboratory testing of monkeypox virus specimens at Laboratory Response Network (LRN) laboratories or authorized commercial laboratories, the recommended specimen type is lesion material. Specifics on the acceptable specimen type accepted within these laboratories may vary. Please contact the appropriate public health department or commercial laboratory to determine acceptable specimens. Please find additional information in CDC Guidance on Preparation and Collection of Specimens.
Skin specimens of the lesions should be collected as soon as monkeypox is suspected. Proper specimen collection is the most important step in the laboratory diagnosis of infectious diseases. Improperly collected specimens may lead to false negatives or inconclusive results. Below are a collection of guidelines to aid in the evaluation of patients with suspected monkeypox.
Collecting and Handling of the Specimens Safely
For healthcare professionals collecting specimens from patients with suspected monkeypox infections, use of PPE is highly recommended, which includes N95 or higher-level respirator, eye protection, gloves, and a gown.
After specimen collection is completed, all protective materials worn by the specimen collector (gloves, mask, gown, etc.) and all used sample collection materials (alcohol wipes, holders, etc.) must be placed in red biohazard bags and autoclaved or incinerated prior to disposal.
Sharps such as needles, blades, etc. used to open vesicles should be disposed of in appropriate puncture-resistant containers for autoclave of infectious waste.
Proper hand hygiene should be utilized before and after specimen collection and following removal of PPE.
Specimen Collection
A minimum of 3 lesions, 6 total swabs/specimens, should be collected, preferably from different locations on the body and/or from lesions with differing appearances.
Swab the lesion with a vigorous back and forth motion while rotating the swab for at least 5 seconds with two separate sterile dry polyester or Dacron swabs.
CDC guidance: Break off the end of the applicator of each swab into a 1.5- or 2-mL screw-capped tube with O-ring or place each entire swab in a separate sterile container. Do not add or store in viral or universal transport media.
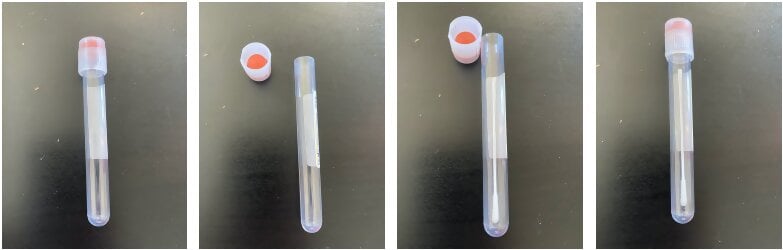
Another option is to place each swab in a No Additive Vacutainer, such as a no additive urine analysis vacutainer. Pop off the cap of the container, place swab inside, break stick if necessary, and place cap back on the vacutainer.
Updated guidance: In addition to dry swabs, CDC can now accept dry lesion swabs in viral transport media and lesion crusts (currently these two specimens must be received by CDC within 7 days of collection).
Storage, and Preservation of Specimen Prior to Shipping
Specimens must be triple packed for storage and shipment:
Freeze (-20°C or lower) specimens within an hour after collection.
However, if there is no freezer available, refrigerate samples (2-8°C) within an hour of collection and store for up to 7 days.
Samples must be received within 60 days if frozen or 7 days if refrigerated.
For transportation out of the facility for laboratory testing, the inside of the tertiary receptacle should be packed with icepacks to ensure the samples stay cool.
Additional information on specimen storage, packaging, and shipping instructions can be found on the CDC information on Poxvirus Molecular Detection and Poxvirus Serology.
Additional information from the CDC can be found on the Laboratory Procedures for Monkeypox and 2022 Monkeypox: Information for Health Departments.