Another year, another Congressional fix to Medicare physician reimbursement. Sadly, we are not out of the woods yet—and the annual song and dance with the Centers for Medicare & Medicaid Services (CMS) and Congress to avoid reductions to physician payments will likely continue for years to come.
In a previous Regs and Eggs blog from October, I gave you a preview of the large-scale reductions that were coming your way in calendar year (CY) 2022— specifically describing these three separate cuts:
- Medicare Physician Fee Schedule (PFS) Conversion Factor: 3.75 percent
- Medicare Sequester: 2 percent
- “Pay-Go” Sequester: 4 percent
- TOTAL: 9.75 percent
Thanks to significant advocacy by ACEP and other medical societies, Congress has now officially stepped in to avert the majority (but not all) of this 9.75 percent cut. To help put what Congress did into context, let me take you on a journey through time: the past, present, and future of Medicare physician payments.
First, I’ll take you on trip down memory lane to remind you of how we got here and what ACEP has done to help preserve emergency medicine reimbursement. Then, we’ll travel together to the present to see how your Medicare reimbursement will be affected in 2022 based on the recent Congressional action. Lastly, we’ll take a look into the future to see what issues we will likely face in 2023 and beyond.
Where we were:
If you recall, we were in the exact same place a year ago. We were facing a significant, 10.2 percent, reduction to the Medicare PFS conversion in 2021, and we needed Congress to act before the end of the year. Congress did in fact act by instituting a one-year fix, which only offset around two-thirds of that 10.2 percent reduction (the conversion factor wound up being reduced by 3.3 percent in 2021).
However, it is important to understand that even with the 3.3 percent reduction to the PFS conversion factor in 2021, many of you still have experienced an overall increase in your Medicare reimbursement this past year. And how did that happen? I’m proud to say that the payment increases you may have seen this year are directly due to ACEP’s advocacy efforts.
ACEP knew ahead of time that reductions in 2021 were likely and took action early on to try to protect emergency physicians from the brunt of these cuts. Specifically, we pushed for significant increases in the values of the emergency department (ED) evaluation and management (E/M) codes levels 3 through 5 (CPT codes 99283, 99284, and 99285)—the most commonly billed codes for emergency medicine. We met with CMS staff directly to advocate for these increases and presented sound arguments for why the agency should adopt revised code values for these services. In the CY 2021 PFS proposed reg (page 50133) released in August 2020, CMS explicitly called out ACEP, stating that based on our comments, the agency decided to increase these code values. In all, instead of a reduction, we estimated that you likely saw increases of 9.8 percent for ED E/M level 3 services, 1.6 percent for ED E/M level 4 services, and 2.0 percent for ED E/M level 5 services, respectively, in 2021 compared to 2020.
Where we are now:
Unfortunately, the one-year fix Congress instituted in 2021 expired, as one-year fixes tend to do after a year! Congress responded last week by kicking the can down the road again and passing yet another one-year fix (as Congress loves to do).
But, believe you me, this one-year fix was hard to get—and only came after ACEP and other medical associations continuously pushed Congress over the past year to take action. For those of you who were able to join us in DC, we made this issue a main topic during our Leadership and Advocacy Conference in July and issued action alerts requesting that you contact your Congressional representative. Based on our advocacy and the actions that many of you took, over half of the members of the House of Representatives (247 in total) joined a bipartisan "Dear Colleague" letter that was sent to Speaker of the House Nancy Pelosi (D-CA) and Minority Leader Kevin McCarthy (R-CA) in October, urging them to provide stability for health care providers by addressing the looming payment cuts. That letter helped push Congress over the finish line.
So, what’s included in the one-year fix for 2022? The Protecting Medicare and American Farmers from Sequester Cuts Act (yes, that’s really the bill’s name) passed by Congress last week addresses the three upcoming cuts to Medicare reimbursement in the following ways:
- PFS Conversion Factor Cuts: The Act provides a one-year increase in the conversion factor of 3.0 percent. Note that this does not fully cancel out the scheduled 3.75 percent reduction, and ultimately leaves us with a 0.75 percent cut in the PFS conversion factor for CY 2022.
- Medicare Sequester: The two percent Medicare sequester payment reductions that have been postponed throughout the COVID-19 pandemic are delayed for an additional 3 months (until March 31, 2022); followed by a 3-month one percent reduction in Medicare payments (April 1, 2022 - June 30, 2022); and ending with the moratorium phasing out completely after June 30, 2022.
- PAYGO Cuts: The Act includes a one-year delay of the statutory 4.0 percent "PAYGO" sequestration cuts. PAYGO is a budget rule that requires any mandatory spending increases or tax cuts to be offset by decreases in spending or tax increases. As you may recall, these PAYGO cuts were triggered by the American Rescue Plan that passed earlier this year, with Medicare PAYGO cuts capped at 4.0 percent.
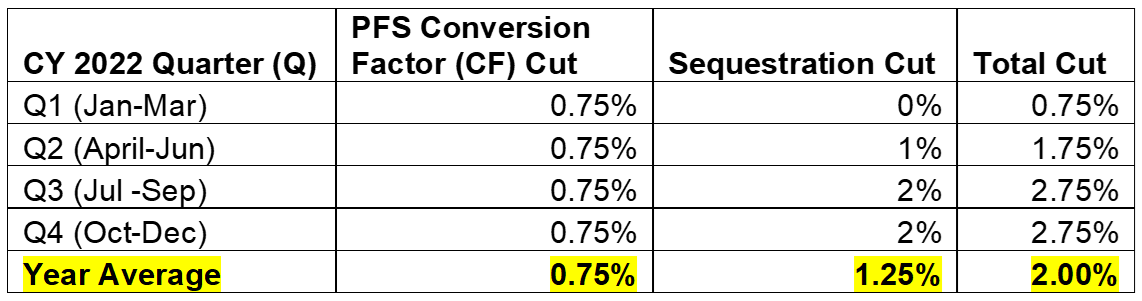
What does this mean for provider reimbursement in general? The two percent Medicare sequester cuts are phased in over the year, and therefore the reduction clinicians will face to their Medicare payments varies depending on what quarter of the year we are in—as if health care policymaking wasn’t complicated enough already. As you can see from the chart below, the total cut to Medicare reimbursement, including both the PFS conversion factor cut and sequestration, averages out to around 2 percent over the course of the entire year.
And what does this mean for your reimbursement as an emergency physician? Well, unfortunately, the 2 percent sequester is not going to go away. In fact, Congress paid for the fix in part by increasing the sequester percentage in 2030 (i.e., kicking that particular can even further down the road). HOWEVER, notwithstanding the sequester (which is really beyond our control), your PFS payments may still be higher than they were in 2020 because of ACEP's previous advocacy work! As you can see from the chart below, you may be better off in 2022 compared to 2020 as a direct result of the increases to the ED E/M levels 3-5 relative value units (RVUs) that ACEP pushed for in 2021. In other words, although the PFS conversion factor has declined in both 2021 and 2022, the RVU increases ACEP secured for the main codes that you bill for have practically made up for these decreases.
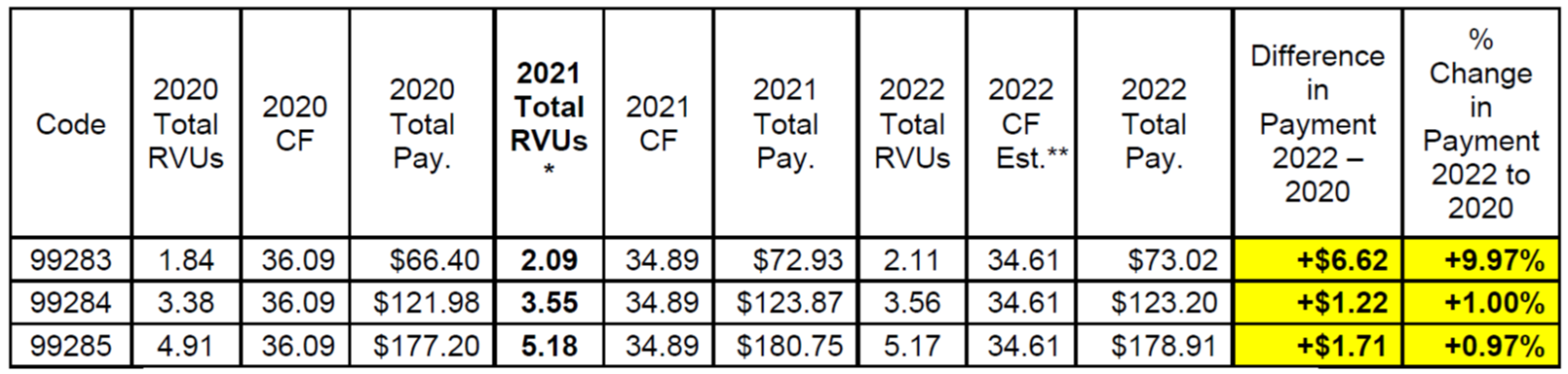
* ACEP proposed higher work RVUs to CMS in 2021, and CMS accepted ACEP’s recommendations.
** CMS has not yet officially updated the conversion factor in 2022 to reflect the Protecting Medicare and American Farmers from Sequester Cuts Act. This is my estimate, which represents a 3 percent increase to the previously finalized 2022 conversion factor of 33.5983 (33.5983 x 1.03 = 34.61).
Remember: Total payment under the PFS = Total RVUs x Conversion Factor
Where we are going
Since Congress instituted another one-year fix for 2022, this latest fix will expire at the end of next year— meaning that CMS will most definitely propose another cut to the PFS conversion factor in 2023. Instead of proposing a 3.75 percent cut as CMS did in 2022, CMS will instead propose a 3.0 percent cut for 2023, since Congress just allowed 0.75 percent of the 3.75 percent reduction to occur in 2022.
And that’s how it’s going to be— Congress may offset another portion of the 3.0 percent cut in a fix at the end of next year, allowing some reduction to the conversion factor to take place in 2023. Then, year-after-year, Congress (after a significant amount of advocacy from ACEP and other medical societies) will probably enact legislation that slowly chips away at the remaining PFS conversion factor reduction until it reaches zero.
The 2 percent Medicare sequester will also continue year-after-year and may even wind up being extended past its current end date of 2030, as Congress will likely continue to use the sequester as a budget gimmick (paid for off of your backs) to pay for legislation that costs money.
What we need, and will continue to strongly advocate for, is stable Medicare reimbursement and more appropriate annual updates that account for the increased cost of providing care to Medicare beneficiaries. To that end, we sent a letter to the Medicare Payment Advisory Committee (MedPAC) this week requesting that the Commission recommend that the PFS conversion factor be updated by the Medicare Economic Index (MEI)—an inflationary factor that is supposed to measure the increased cost of providing physician services each year. Right now, the PFS is scheduled to receive an annual update of zero percent until 2026. Further, we requested that MedPAC recommend other policies to CMS and Congress that would further incentivize high-quality care, protect the safety net, and reduce disparities in terms of access to care in rural and underserved communities.
Finally, ACEP will ALWAYS push for regulatory changes and payment reforms that we can directly control—such as the 2021 RVU increases—which will benefit all of you as emergency physicians regardless of where you work or your practice environments.
ACEP knows that we have more work to do to prevent future cuts, and we will continue to fight the good fight every day on your behalf.
Until next week, this is Jeffrey saying, enjoy reading regs with your eggs.