As emergency physicians, you can breathe a little easier now. Instead of a cut to Medicare reimbursement in 2021, now, with the passage of the major omnibus bill at the end of 2020, many of you will actually see an increase in your Medicare reimbursement this year. And since many private payors use Medicare payment levels to set their rates, you hopefully will receive some much needed financial security during this very difficult time.
So what exactly happened? As you may recall from my Regs & Eggs post on the 2021 Medicare physician fee schedule (PFS) final regulation, the Centers for Medicare & Medicaid Services (CMS) finalized a 10.2 percent cut to the PFS conversion factor. Since the PFS conversion factor converts all PFS codes to a dollar amount, this major cut would have impacted every health care practitioner that bills Medicare. ACEP therefore joined with the American Medical Association (AMA) and other medical associations in fiercely opposing this cut and urging Congress to pass legislation that would eliminate the reduction.
While Congress did not completely eliminate the cut to the conversion factor in the omnibus bill, the legislation did include two provisions that, taken together, had the overall effect of offsetting around two-thirds of the 10.2 percent reduction. First, the bill granted CMS enough funding to add 3.75 percent back to the PFS. Second, it delayed the implementation of the add-on code for complexity (G2211) for three years until 2024. This single code had initially accounted for around 3 percent of the conversion factor cut.
CMS recently updated the PFS conversion factor to incorporate these legislative changes. Instead of the 10.2 percent cut that was initially calculated, the conversion factor will now be reduced by only 3.3 percent in 2021 compared to 2020.
Now, how does that impact you specifically? It is important to remember that your total Medicare reimbursement depends on both the conversion factor and the codes that you typically bill. As seen below, the total payment any health care practitioner receives for a service is based on the amount of relative value units (RVUs) for the service (which include work, practice expense, and malpractice RVUs), the size of the conversion factor, and a geographic adjustment.
Total payment under the PFS = Total RVUs x Conversion Factor x Geographic Adjustment
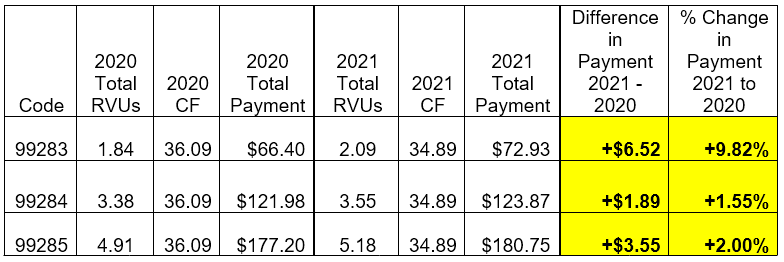
Knowing ahead of time that the conversion factor would likely be cut in 2021, ACEP took action early to ensure that you as emergency physicians would receive an appropriate level of reimbursement for the services you deliver. When CMS announced last year that it was seeking to revalue the office and outpatient evaluation and management (E/M) codes for 2021, ACEP advocated strongly for corresponding increases for the ED E/M codes levels 3 through 5 (CPT codes 99283, 99284, and 99285)—the most commonly billed codes for emergency medicine. These efforts built on our advocacy to the AMA’s RVS Update Committee (RUC). ACEP also provided data and a solid policy argument directly to CMS and the White House to help strengthen our case. That advocacy paid off, and CMS adopted our increased code values for the ED E/M codes in 2021.
Initially, the large, 10.2 percent across-the-board cut to the conversion factor totally wiped out the increases to the ED E/M code values—resulting in an estimated 6 percent reduction to your payments. Now, with a smaller cut to the conversion factor, these increases will show through. In fact, we have calculated that you will see an increase of 9.8 percent for ED E/M level 3 services, 1.6 percent for ED E/M level 4 services, and 2.0 percent for ED E/M level 5 services in 2021.
While this is great news, we are not totally out of the woods yet. A 2 percent reduction to Medicare reimbursement instituted in 2013, called sequestration, continues to rear its ugly head. Although Congress temporarily halted sequestration during the COVD-19 public health emergency, it is now scheduled to come back in full force on April 1, 2021. Further, looking past 2021, the additional PFS spending caused by the large increases to the office and outpatient E/M codes will continue to result in across-the-board cuts to the conversion factor. While Congress intervened in 2021 to offset a large proportion of the conversion factor cut, it may need to act again before January 1, 2022 to prevent another reduction from occurring. Finally, CMS could decide in 2024 to institute G2211—the add on code for complexity. As previously mentioned, the implementation of that code would result in a significant cut to the conversion factor.
ACEP knows that we have more work to do to prevent future cuts, but for now, I am happy to say: crisis averted, and we will continue to fight another day.






