Consensus Recommendations on the Treatment of Opioid Use Disorder in the ED
Learn MoreACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
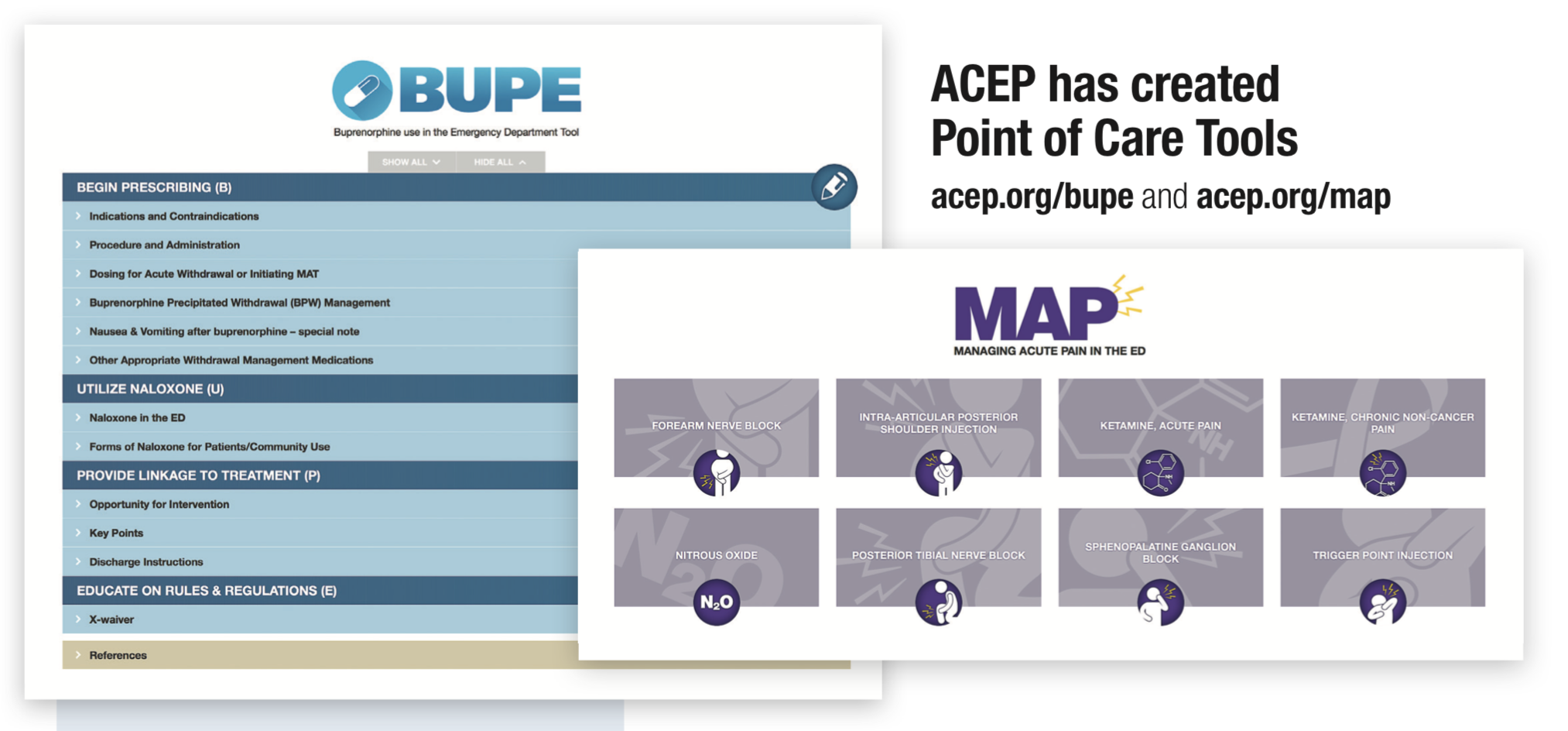
Every day emergency physicians see the devastating consequences of the opioid epidemic. ACEP is one of the leaders in the battle against this epidemic. Here are some of the initiative and resources ACEP has developed and continues to work on to empower emergency physicians.
Receive clinical guidance, discover tools and resources, and get your questions answered through ACEP’s EM Opioid Advisory Network - a panel of emergency physicians offering expert advice.
For a quick introduction to Opioids, Opioid Use Disorder and ED initiated Buprenorphine please see ACEP's Opioid Summary Guide.
ACEP Helps Get 3-Day Bupe Rule Changed to Improve Patient Care
Dec. 12, 2020 - As part of the stopgap funding bill approved by Congress in December 2020, emergency physicians will now be able to dispense up to a three-day supply of buprenorphine at one time to a patient suffering from acute withdrawal symptoms. The funding bill included the "Easy Medication Access and Treatment for Opioid Addiction Act" (Easy MAT Act), H.R. 2281, which ACEP has been working on with Congressman Dr. Raul Ruiz (D-CA) since last year. Read more.
Congress Passes Opioid Package
Oct. 24, 2018 - President Trump signed a sweeping legislative package of bills to address the nation's growing opioid epidemic. Included in the package are the "Alternatives to Opioids (ALTO) in the Emergency Department Act" and the "Preventing Overdoses While in Emergency Rooms (POWER) Act," both of which ACEP developed with the sponsoring members of Congress. Read the press release.
Read more about Emergency Medicine Opioid Principles on ACEP's advocacy website.
ACEP Letter of Support - "Excellence in Mental Health & Addiction Treatment Expansion Act”
HR 3931
S. 1905
October 19, 2017
ACEP-Supported Innovations Bill Sent to President
December 2016
ACEP Letter of Support for the "21st Century Cures Act"
House
Senate
November 2016
Congress Approves Comprehensive Addiction and Recovery Act
July 2016