ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
Memphis, Tennessee
Frank Zilm & Associates, Inc.
Kansas City, Missouri
Frank Zilm, DArch, FAIA, FACHA, President
Jon R. Summers, Principal, brg3s
Opened September 2014
Key Words
Operational efficiency
Space issues
Problem/Situation
The old emergency department was significantly undersized for the then-current and projected volumes with poor ambulance and walk-in access and limited ambulance capacity. The old emergency department had 37 patient stations, yet projections for next few years indicated need for 54 to 60 stations. The problem was identified in 2008.
Solution
Planning for expanding or replacing the emergency department began in 2008. Initially the focus was on locating the emergency department on a confined urban health care campus. Six to eight site options were considered. Final location was determined, which placed a new emergency department at the then-current main entrance to the hospital, relocating the main entrance while maintaining the existing lobby. Site circulation during construction, both pedestrian and vehicular, was a significant challenge. The final design incorporated two major new concepts never before used in the state of Tennessee:
Both “paper” and computer simulations were used to test the new operational concepts with the proposed plan.
Another challenge included designing the building to accommodate a seven-story future addition without interruption to the new emergency department. A modular heliport was used that can be relocated to the top of the future addition.
After 6 months, the new emergency department is viewed as a success, albeit with the operational challenges associated with moving from 17,000 sf to 32,000 sf. One week prior to opening, another regional hospital closed with much of its emergency department volume shifting to the Methodist emergency department. This additional volume, which was unexpected, put significant burden on the new emergency department, which opened with minimum additional staff. Staffing has been slowly increased to meet the demand, yet the facility has performed well.
Lessons Learned
Editorial Commentary
The use of ambulance access on a floor below the emergency department has proved to work and made the project doable on a tight site. The emergency department layout mixes resuscitation rooms with other patient treatment rooms to balance staffing. Linear peripheral circulation is used as the organizing principle. The emergency department uses a split- flow approach that divides patients into vertical and horizontal streams. The very large ambulance arrivals area below the emergency department provides numerous opportunities for disaster preparedness.
Figure 1.
Illustration depicting staff inner core, Methodist University Hospital, Emergency Department.
Figure 2.
Ground floor plan with emergency vehicle plaza.
Figure 3.
Aerial view.

Figure 4.
First floor plan indicating treatment, support, and public spaces.
Figure 5.
First floor plan indicating staff inner core, public corridor, and treatment spaces.
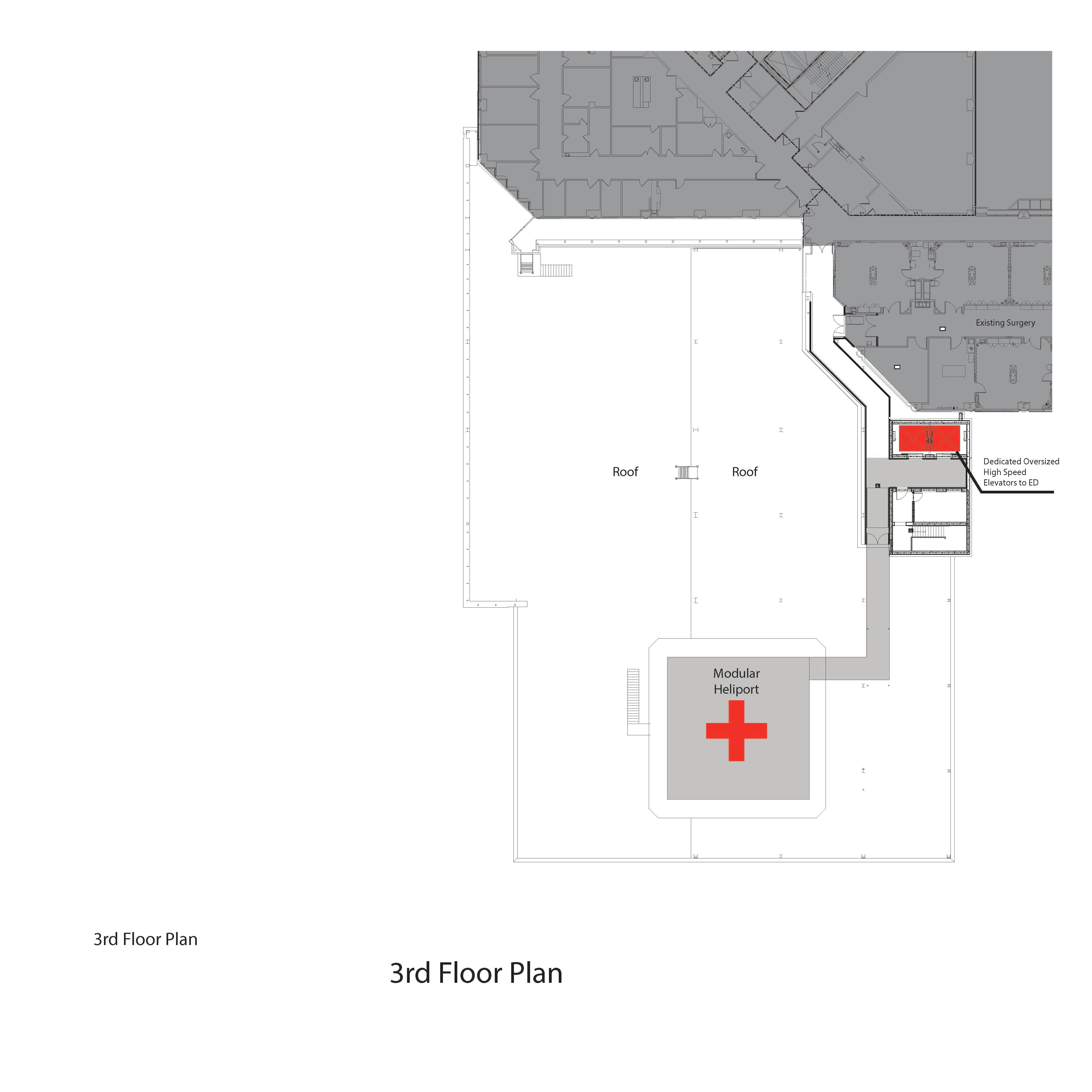
Figure 6.
Third floor plan.