Identify
How should EDs identify pediatric patients’ vaccination status?
Regional Immunization Information Systems
The working group recognizes that regional immunization information systems vary in their utility and their capability for bidirectional flow of vaccination data. Moreover, this capability of hospitals to access the regional immunization information system may change with time or with changes in their electronic health record system (EHR). We recommend that EDs utilize the regional immunization information system to ensure patients’ up-to-date status in situations where hospitals can link to regional immunization information systems and can easily and reliably determine the ED patient’s vaccination status.
Depending upon the ED, staff can obtain access to immunization information systems information in these ways:
- If the ED utilizes an EHR, check with the system administrators to see if there is an existing connection with the immunization information system. If there is an established connection, the individuals wanting access will likely need to request access from the local system administrators, not from the immunization information system. It might be worth checking the EHR vaccination section to see if there is already immunization information system.
- If the ED does not utilize an EHR, connect with the state immunization information system. State Immunization Information Systems List (CDC).
- If the ED does utilize an EHR, but no connection to the immunization information systems, this may be a two-part solution. First, contact the state immunization information system to see if you can get connected via the user interface while you work with the EHR administrators to see if they can work to establish an electronic interface for data exchange. As long as the individual is set up with access to view/add (might be different language on this depending upon the jurisdiction) they should be able to view and add patients and vaccines. More than 80% of immunization information system data comes from established data exchange (EHR to immunization information system), which is helpful for any person who needs to input the information. In this way, medical staff input immunization records into the EHR, which then automatically sends/receives vaccine data.
Health System Electronic Health Record
For children in an ED that is affiliated with their medical home, the ED’s EHR may connect to an accurate vaccination record. The ED personnel may access this.
Triage Assessment for Vaccination Status
There is little evidence-base regarding best-practices for triage nurse assessment of pediatric vaccination status, especially in the context of utilizing immunization information systems or medical home EHRs. Moreover, there may be difficulties in assessing the nuances of each child’s vaccination status (e.g., a child who seems behind on vaccine according to immunization information systems may be up-to-date in the PCP’s EHR).
Nevertheless, especially in cases where an ED does not utilize the regional immunization information system, the triage assessment of a child’s vaccination status may be quite relevant in terms of their clinical care and important in terms of identifying under-vaccinated patients.
For this reason, we recommend that, in the absence of access to a regional immunization information system, triage assessment for vaccination status accomplish two main goals.
- The triage assessment for vaccination status quickly determines the children whose caregivers believe that the children are up-to-date. Although this parental belief may be mistaken, for these patients, we recommend no further ED intervention for administering or encouraging routine childhood vaccinations.
- For children whose caregiver reports that they are not fully vaccinated, the ED staff might assess the barriers to vaccination in a non-judgmental fashion and assist the caregiver as appropriate.* We recommend the following.
- For patients who have identifiable barriers to vaccinations, the ED should provide social work or other linkage services, as appropriate. Note that some EDs may have the capacity to provide routine childhood vaccinations in the ED. In these circumstances, EDs may provide routine childhood vaccinations, as appropriate.
- For caregivers who are vaccine hesitant, the ED should deliver a non-judgmental, culturally competent recommendation. (See section below.)
- For caregivers who are vaccine intent with no barriers to primary care, the ED should specifically refer to primary care or vaccination providers. Note that some EDs may have the capacity to provide routine childhood vaccinations in the ED. In these circumstances, EDs may provide routine childhood vaccinations, as appropriate.
*Triage Flowcharts for assessing pediatric patients’ vaccination status are given in the appendix.
Appendix: Triage Flowcharts for Assessing Pediatric Patients’ Vaccination Status
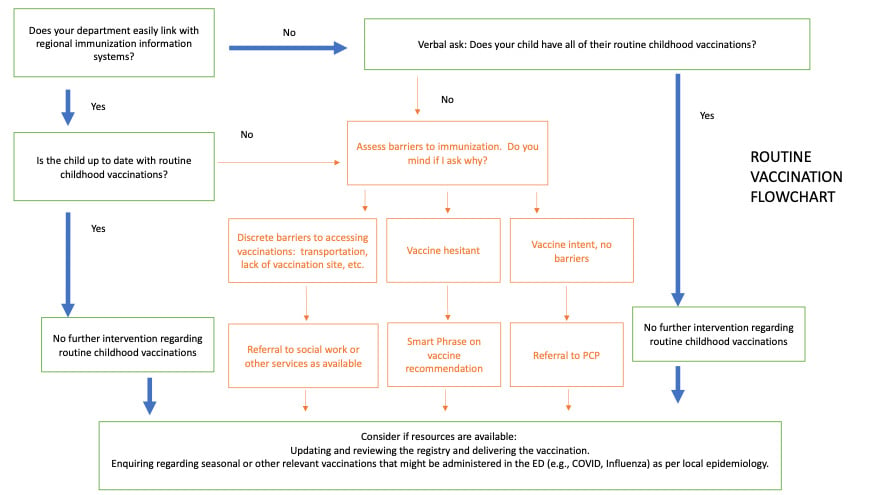
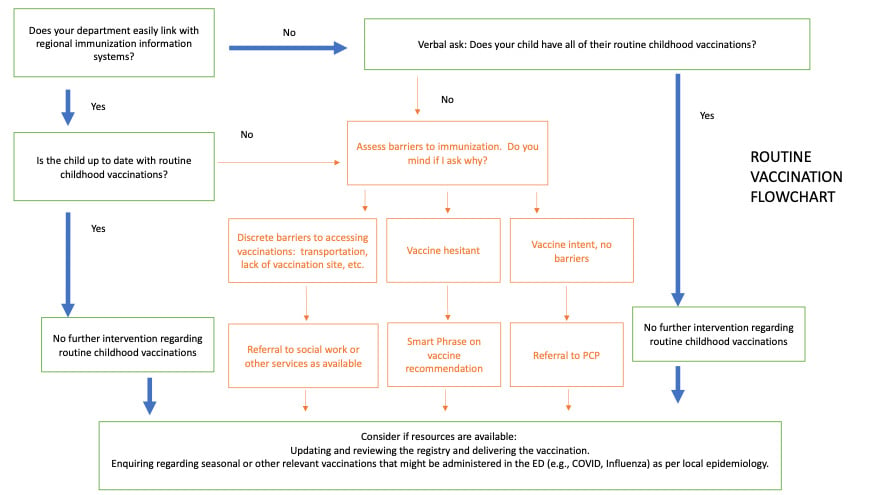
Routine Vaccination Flowchart
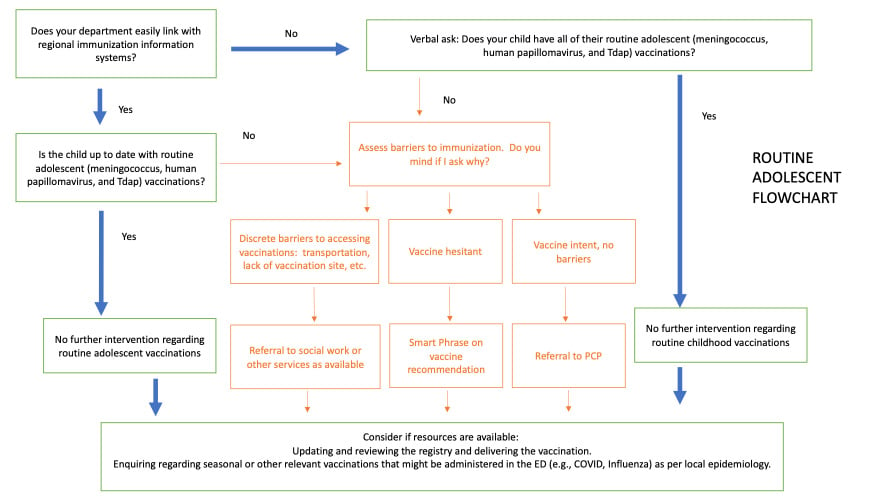
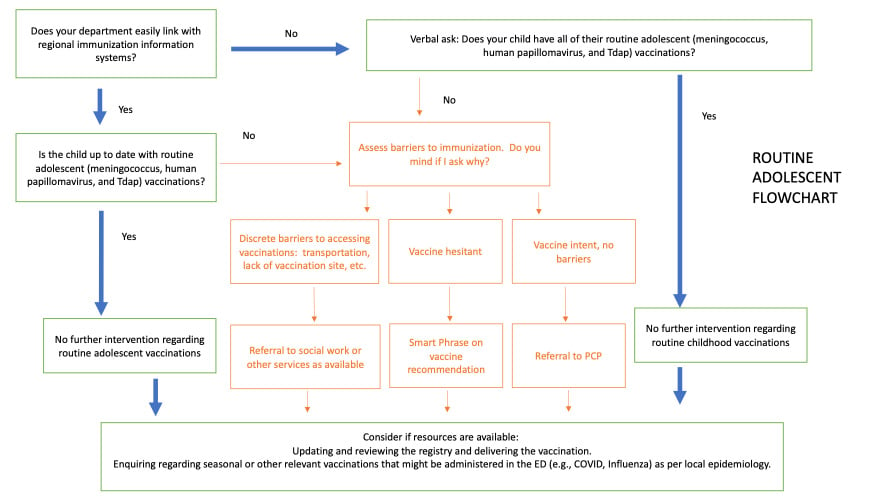
Routine Adolescent Flowchart
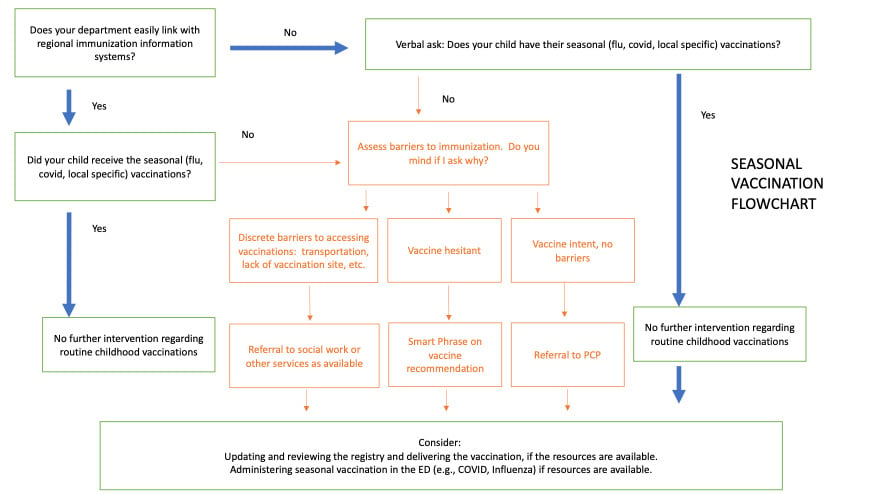
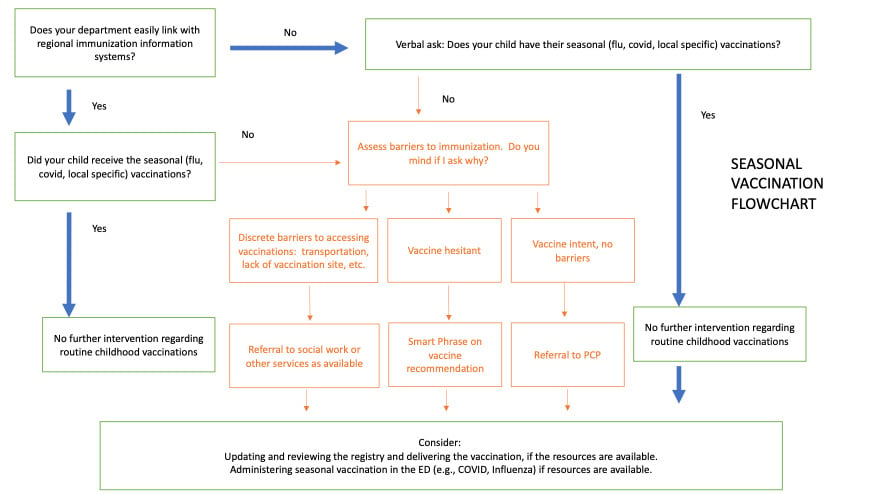
Seasonal Vaccination Flowchart
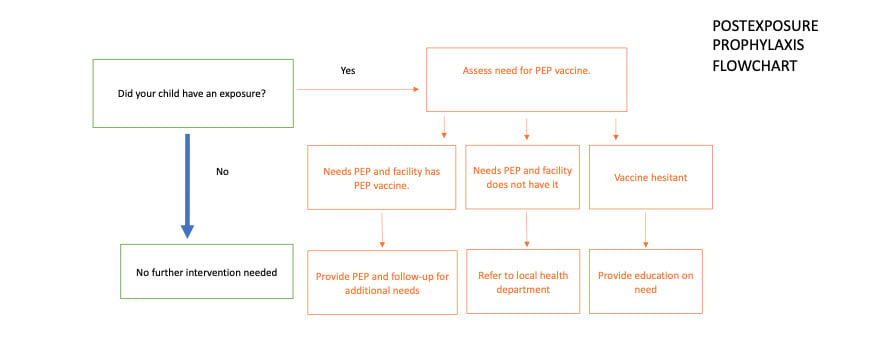
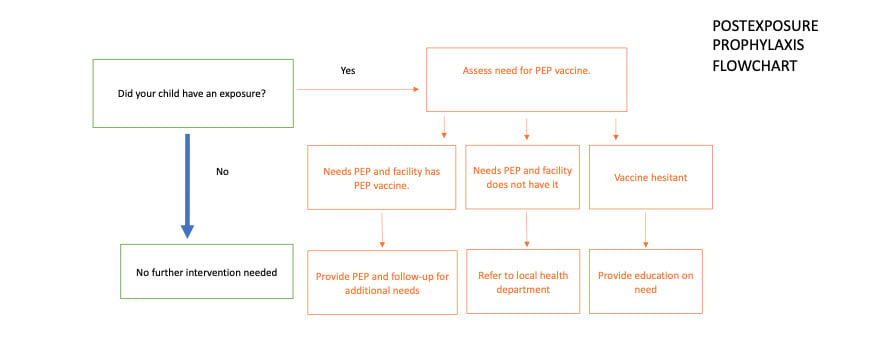
Postexposure Prophylaxis Flowchart