ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
1. What is the RAC program?
As part of the efforts to fight fraud, waste and abuse in the Medicare program, the Tax Relief and Health Care Act of 2006, required a national Recovery Audit Contractor (RAC) program to be in place by January 1, 2010. The goal of the recovery audit program is to identify improper payments made on claims for services provided to Medicare beneficiaries. Improper payments may be overpayments or underpayments.
Overpayments can occur when health care providers submit claims that do not meet CMS coding or medical necessity policies. Underpayments can occur when health care providers submit claims for a simple procedure, but the medical record reveals that a more complicated procedure was actually performed. Providers that could be reviewed include hospitals, physician practices, nursing homes, home health agencies, durable medical equipment suppliers and any other provider or supplier that submits claims to Medicare.
2. Are there any significant changes in the program for 2024?
None are currently planned.
In March 2020, CMS suspended RAC reviews due to the 2019-Novel Coronavirus (COVID-19) Public Health Emergency (PHE). However, in August 2020 RAC audits resumed.
CMS recently modified the RAC program in response to many concerns raised. These modifications in the program have been made to reduce provider burden, according to CMS. Improvements include the following:
The RACs in Regions 1-4 perform postpayment review to identify and correct Medicare claims that contain improper payments (overpayments or underpayments) that were made under Part A and Part B for all provider types other than Durable Medical Equipment, Prosthetics, Orthotics and Supplies and Home Health/Hospice. The Region 5 RAC is dedicated to the postpayment review of DMEPOS and home Health/Hospice claims nationally. In May 2016, CMS revised the method used to calculate additional documentation requests (ADR) limits for institutional providers (Facilities).
3. Will the Recovery Audit Contractors (RACs) replace all current review entities?
No. Other entities such as Medicare Administrative Contractors, Medicaid, Program Safeguard Contractors, Office of Inspector General or Quality Improvement Organizations (QIOs) could still review a provider's claims. The RACs will not review a claim that has previously been reviewed by another entity. One new entity is the Supplemental Medicare Review Contractor (SMRC). The Centers for Medicare & Medicaid Services (CMS) has contracted with Strategic Health Solutions, LLC, a Supplemental Medical Review/Specialty Contractor (SMRC) to “perform and/or provide support for a variety of tasks aimed at lowering the improper payment rates and increasing efficiencies of the medical review functions of the Medicare and Medicaid programs”.
SMRC will be conducting nationwide medical review as directed by CMS. The medical review is performed on Part A, Part B, and DME providers and suppliers. Provider Compliance Group/Division of Medical Review and Education (DMRE) will select the services and provider specialties that will be reviewed. SMRC will evaluate medical records and related documents to determine whether Medicare claims were billed in compliance with coverage, coding, payment, and billing practices. CMS internal data analysis, the Comprehensive Error Rate Testing (CERT) program, professional organizations and Federal oversight agencies will contribute to determining what is to be audited. Once errors are identified, CMS will be notified of the improper payments and/or noncompliance with documentation requests. At that point, the MAC may determine to initiate claim adjustments and/or overpayment recoupment actions through the established Medicare overpayment recovery process.
4. As of 2024, who are the RAC contractors?
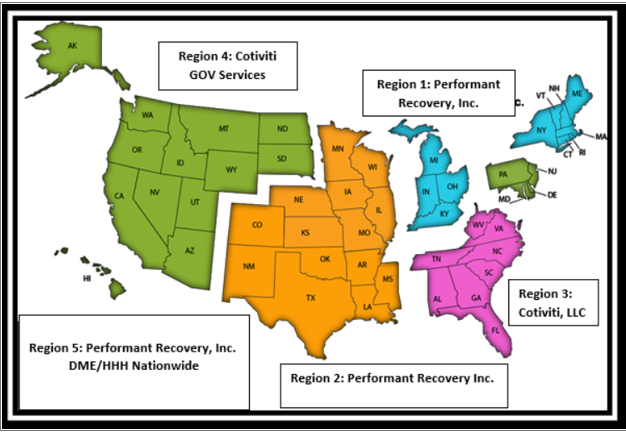
The country has been divided into five regions. Each region has been awarded to a contractor. The RACs were selected under an open bidding process. The RACs will be paid on a contingency fee basis on the overpayments and underpayments they identify.
RACs in Regions 1-4 will perform post payment review to identify and correct Medicare claims specific to Part A and Part B.
Region 5 RAC will be dedicated to review of Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) and Home Health / Hospice.
Medicare Fee for Service RAC Contact Information
Providers should first attempt to contact the Recovery Audit Contractors (RAC) through the customer service line. If that does not answer the provider's questions and/or concerns, then the provider can email CMS.
|
Recovery Audit Contractors 2020 |
||||
|
Region |
States |
Websites |
|
Phone Number |
|
Region 1 Performant Recovery, Inc. |
CT, IN, KY, MA, ME, MI, NH, NY, OH, RI, and VT |
1-866-201-0580 |
||
|
Region 2 Performant Recovery, Inc. |
AR, CO, IA, IL, KS, LA, MO, MN, MS, NE, NM, OK, TX, and WI |
1-866-201-0580 |
||
|
Region 3 Cotiviti LLC |
AL, FL, GA, NC, SC, TN, VA, WV, Puerto Rico and U.S. Virgin Islands |
1-866-360-2507 |
||
|
Region 4 HMS Federal Solutions |
AK, AZ, CA, DC, DE, HI, ID, MD, MT, ND, NJ, NV, OR, PA, SD, UT, WA, WY, Guam, American Samoa and Northern Marianas |
|
Part A: 1-877-350-7992 Part B: 1-877-350-7993 |
|
|
Region 5 DME/HHE/ |
Nationwide for DMEPOS/HHA/ |
1-866-201-0580 |
||
5. What are the RAC auditors looking for?
The RAC contractors are tasked with identifying improper payments made on claims of health care services provided to Medicare beneficiaries. Each RAC uses their own proprietary software and the RAC's interpretation of Medicare rules and regulations. These payments may be underpayments or overpayments. This will be done by focusing auditing efforts on companies and individuals whose billings for Medicare services trend higher than the majority of providers and suppliers in their community. In these cases, the RAC proprietary software has determined there is a possibility that the claim may contain an error.
Under most circumstances, the RAC will request medical records from the provider to determine whether overpayment(s) and/or underpayment(s) have occurred. When medical records are submitted, the process is called a Complex Review. In these cases, the RAC proprietary software has determined there is a high probability (but not certainty) that the claim contains an overpayment.
In some situations, the RAC may use automated reviews to demand monetary recoupment (where NO medical record is involved in the review) in situations where the RAC proprietary process determines with certainty that the claim contains an overpayment. An automated review must:
The RAC will also work directly with beneficiaries to ensure they received the durable medical equipment or home health services for which Medicare was billed and that the items and services were medically necessary. The RAC's will review paid claims for all Medicare Part A and B providers to ensure their claims met Medicare statutory, regulatory and policy requirements and regulations.
Payments will be deemed improper when:
Medicare pays a claim that should have been paid by a different health insurance company (e.g. beneficiary is employed and gets health benefits through his or her job, that health insurance company-not Medicare-that may be the primary payer of the beneficiary's health care services).
6. What types of penalties or fines might the RAC contractor be empowered to levy?
The RAC Contractor has the ability to perform extrapolation based on improper payments identified during a review.
When RACs choose to do extrapolation, they will have to follow all of the same instructions that the CMS carriers, FIs and MACs have to follow about selecting a statistically valid random sample using a statistician and any other requirements for using extrapolation.
Interest will accrue from the date of the final determination and be charged on an overpayment amount for each 30-day period that payment is delayed. Any payments received from a provider will be first applied to any accrued interest and then to any remaining principal balance.
7. What should I do if I receive correspondence from a RAC auditor requesting records?
If a request is received for records from a RAC contractor, the records requested must be sent in a timely manner. The response must be received within 45 calendar days or request an extension within those 45 days. The RAC may make a finding than an overpayment or underpayment exits if there is no timely response to a request for medical records. When you receive a records request from a RAC, you should have the claim in question reviewed internally and start preparing to file an appeal in the event that the RAC determines that the claim was overpaid.
8. What is the RAC process timeline?
Note: if an appeal is filed later than 30 days, the contractor will also stop recoupment at whatever point that an appeal is received and validated, but Medicare may not refund any recoupment already taken.
There are five levels of appeal:
Medicare expects providers to “Stay in the know on proposed and approved topics that RAC's are able to review.” These topics will be updated monthly on the RAC reviews topic page and include:
TOP ISSUES PER REGION 2020
|
Region 1 |
Global versus Technical Component/Professional Component Reimbursements: Unbundling; Physician/Non-Physician Practitioner Coding Validation; Facility vs Non Facility Reimbursement: Incorrect Coding; Observation Evaluation and Management Services Billed Same Day as Inpatient: Unbundling; Critical Care Billed on the Same Day as Emergency Room Services |
|
Region 2 |
Procedures that Include Ultrasound: Incorrect Coding; Modifier 57 for Procedure with a 0-Day or 10-Day Global Indicator: Incorrect Coding; Modifiers TC and 26: Incorrect Coding Critical Care Professional Services: Unbundling; Observation Evaluation and Management Services Billed Same Day as Inpatient: Unbundling; Critical Care Billed on the Same Day as Emergency Room Services: Unbundling; |
|
Region 3 |
Procedures that Include Ultrasound: Incorrect Coding; Modifier 57 for Procedure with a 0-Day or 10-Day Global Indicator: Incorrect Coding; Modifiers TC and 26: Incorrect Coding Critical Care Professional Services: Unbundling; Observation Evaluation and Management Services Billed Same Day as Inpatient: Unbundling; Critical Care Billed on the Same Day as Emergency Room Services: Unbundling; |
|
Region 4 |
Procedures that Include Ultrasound: Incorrect Coding; Modifier 57 for Procedure with a 0-Day or 10-Day Global Indicator: Incorrect Coding; Modifiers TC and 26: Incorrect Coding Critical Care Professional Services: Unbundling; Observation Evaluation and Management Services Billed Same Day as Inpatient: Unbundling; Critical Care Billed on the Same Day as Emergency Room Services: Unbundling; |
|
Region 5 |
Not Applicable to Part A and B. |
9. What is the success rate for RAC appeals?
10. What are identified areas for risk?
CMS is requiring that the Recovery Audit Contractor post the list of issues that they are going to be reviewing on their website. All proposed new issues come from the RAC. They will be submitted to CMS and have to be approved by CMS. Once they are approved, the new issues will be posted to the RAC Website for each contractor.
11. Will the RACs be reviewing E/M services?
RACs are able to review any and all services billed by a physician or any other provider who bills the fee for service under Medicare. RACs must follow the rules in place for all Medicare contractors for physician E/M services, and those rules currently state that a reviewer will review an emergency department claim under the 2023 guidelines.
12. Should our hospital/physician group implement an audit program in preparation for the RAC?
You may want to consider being proactive in reviewing your company's coding, billing and documentation practices to assure Medicare compliance. Consider taking a sampling of your claims and review the documentation to assure that it supports the billed E/M coding, services billed, medical necessity, and services or test ordered.
13. How far back can the RAC contractors go when selecting claims for review?
RACs are able to look back three years from the dates the claim was paid. In 2015, CMS limited the RAC look-back period to 6 months from the date of service for patient status reviews, in cases where the hospital submits the claim within 3 months of the date of service. That same look-back condition will continue in 2024.
14. Can RACs review records before claims are paid?
The Recovery Audit Prepayment Review programs allow RACs to review claims before they are paid to ensure that the provider complied with all Medicare payment rules. The Targeted Probe and Educate (TPE) program, looks for providers and suppliers who have high claim error rate or unusual billing practices and for items and services that have a high national error rate and are a financial risk to Medicare.
Common claim errors identified are (a)missing provider signature; (b)encounter notes that do not support all elements of eligibility, and (c) Documentation that does not meet medical necessity, and; Missing or incomplete initial certifications or recertification. If chosen, providers receive a letter from their MAC. The MAC will review 20-40 provider claims and supporting medical records. If compliant, the provider will not be reviewed again for at least one year for the selected audit topic. If some claims are denied, the provider will be invited to a one-on-one education session and give a 45-day period to make changes and improve.
15. Can we expect other payers to conduct RAC audits in 2024?
Medicaid has implemented RAC audits. The Affordable Care Act (ACA) requires Medicaid agencies to contract with Recovery Audit Contractors (RACs) to identify and recover overpayments and to identify underpayments. States must also develop processes for entities to appeal RAC determinations, and coordinate RAC efforts with other Federal and state law enforcement agencies. Most states have developed comprehensive Medicaid RAC solutions to meet ACA requirements.
In addition to Medicaid RACs, Medicaid MIC’s (Medicaid Integrity Contractors) report directly to CMS and have the responsibility for Audit, Review and Education. There are five jurisdictions of MICs, New York (CMS Regions I & II); Atlanta (CMS Regions III & IV); Chicago (CMS Regions V & VII); Dallas (CMS Regions VI & VIII); and San Francisco (CMS Regions IX & X).
16. Is there any oversight of the RAC contractors to assure they follow the same guidelines imposed on the providers?
Yes. According to CMS, it has made changes to the review approval process to even further improve the RACs’ identifications, as well as the overturn rate of appeals. CMS now requires the MACs to validate the RACs’ proposed review methodology and policy interpretations for their particular jurisdictions to minimize incorrect findings. While the review approval process should minimize these occurrences, CMS assures that it will work quickly to resolve the issues, so the provider can avoid the burden of the appeals process when issues do occur.
Additional Reading
Updated January 2024
Disclaimer
The American College of Emergency Physicians (ACEP) has developed the Reimbursement & Coding FAQs and Pearls for informational purposes only. The FAQs and Pearls have been developed by sources knowledgeable in their fields, reviewed by a committee, and are intended to describe current coding practice. However, ACEP cannot guarantee that the information contained in the FAQs and Pearls is in every respect accurate, complete, or up to date.
The FAQs and Pearls are provided "as is" without warranty of any kind, either express or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. Payment policies can vary from payer to payer. ACEP, its committee members, authors or editors assume no responsibility for, and expressly disclaim liability for, damages of any kind arising out of or relating to any use, non-use, interpretation of, or reliance on information contained or not contained in the FAQs and Pearls. In no event shall ACEP be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material. Specific coding or payment related issues should be directed to the payer.
For information about this FAQ/Pearl, or to provide feedback, please contact ACEP's Reimbursement Team.