The Resuscitationist’s Approach to Severe Hyponatremia
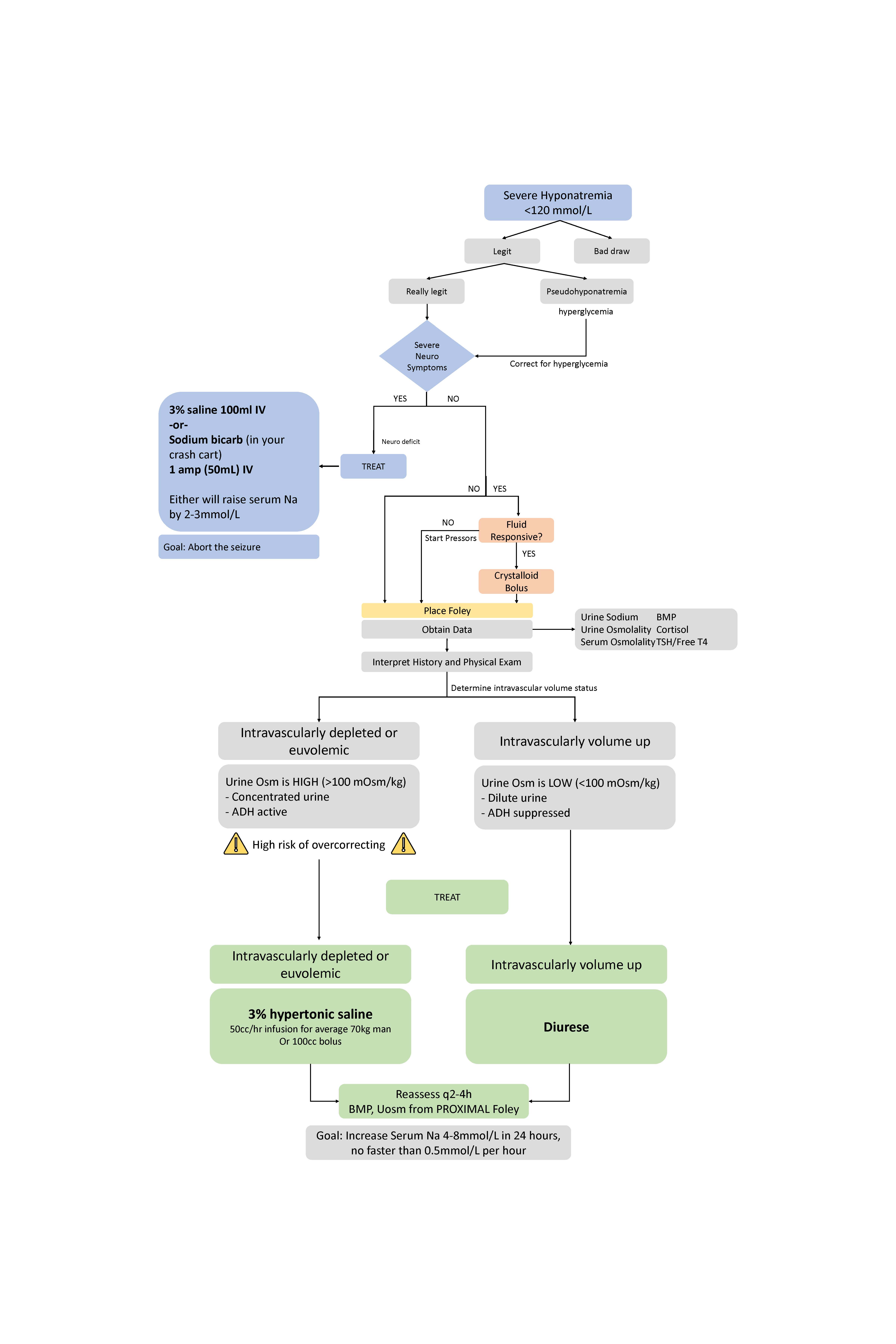
Hyponatremia, defined as serum sodium <135mmol/L, is a factor in 1 in 5 emergency department admissions and is associated with increased mortality and hospital length of stay.1 Diagnosis and treatment of hyponatremia during the resuscitation phase is challenging given its complex pathophysiology and confusing treatment modalities. Reliance on laboratory results to guide resuscitation is impractical. The resuscitationist’s approach to severe hyponatremia offers a 5-step approach focusing on the initial management of severe neurologic sequelae, resuscitation of shock, and subsequent evaluation and treatment of hyponatremic patients based on underlying pathophysiology and antidiuretic hormone (ADH) action. It also identifies and treats overcorrection to avoid osmotic demyelination syndrome.
The Resuscitationist’s Approach
#1: Treat Severe Neurologic Sequelae
Patients with hyponatremia can exhibit neurologic findings including dizziness, altered mental status, seizure, and coma, depending on chronicity.2 Complications include stupor, coma, and seizure. These symptoms are common when serum sodium is <120mmol/L.1,2 Severe hyponatremia is treated promptly with 100-150ml IV hypertonic 3% NaCl over 10-20 minutes up to 3 times, or until the cessation of seizure or improvement in mentation.3 100mL of 3% saline usually raises serum sodium to 2-3mmol/L.2 Initially increasing serum sodium by 4-6mmol/L reduces the risk of brain herniation and aborts most seizures.4 3% NaCl is not always readily available and delays occur while awaiting pharmacy compounding. However, sodium bicarbonate is available in crash carts and can substitute for 3% NaCl when administered over 10 minutes. 100mL of 3% NaCl and 1 ampule of 8.4% sodium bicarbonate contains roughly 50mEq of sodium.5
#2: Resuscitate Shock
Divide patients into fluid-responsive and non-fluid-responsive shock. Patients with fluid-responsive shock should receive fluids without fear of a significant change in serum sodium. Lactated ringers are preferred over normal saline initially due to the sodium content (130mmol/L of sodium vs 154 mmol/L, respectively). The Adrogué-Madias formula predicts, for a 70kg man, one liter of lactated ringers will increase serum sodium by 0.32 mmol/L whereas saline by 0.79 mmol/L.5 Therefore, hyponatremic patients can receive several liters of either solution with minimal increase in serum sodium. Consider vasoactive medications instead in patients with non-fluid-responsive shock. When not in shock, resist giving hyponatremic patients isotonic crystalloid before collecting data. Unnecessary fluids will alter the patient’s initial urine studies and place them at risk for overcorrection.1
#3: Obtain Accurate Data
Additional data must be obtained for patients resuscitated from a neurologic and shock standpoint. Foley catheterization is critical to visually qualifying urine osmolality throughout the patient’s resuscitation while waiting for urine sodium, urine osmolality, serum osmolality, and serum sodium labs. Cortisol and thyroid studies may also be obtained. Thorough history helps differentiate etiologies of hyponatremia including malignancy and medication-induced syndrome of inappropriate antidiuretic hormone (SIADH), excessive free water or alcohol intake, and malnutrition.1,2 Organ dysfunction including cirrhosis, chronic renal failure, and heart failure particularly with recent diuresis should be noted.1,2
#4: Determine Intravascular Volume Status
Hypovolemic, euvolemic, and hypervolemic etiologies are traditionally based on physical exam, serum and urine sodium, and serum and urine osmolality. However, labs require hours to complete. Instead, appropriate treatment can be quickly deduced via assessment of intravascular volume status based on history, physical exam, and visual qualification of urine osmolality at the proximal foley. Intravascularly depleted patients (distributive shock, hypovolemia) or euvolemic patients with endocrinopathy, malnutrition, and excessive water or alcohol intake can be grouped by their underlying physiology. These patients appear dry or euvolemic on the exam, they have high urine osmolality due to real or perceived volume depletion and inappropriately active ADH resulting in water retention and worsening their hyponatremia.2 This also includes patients with congestive heart failure or cirrhotics who were diuresed, those with nephrotic syndrome, or patients with significant third-spacing.2 Importantly, these patients are at risk of overcorrecting. Baroreceptors perceive fluid resuscitation as an improvement in intravascular volume status, leading to ADH suppression and subsequent free water loss, thus rapidly increasing serum sodium.1
True hypervolemic patients’ urine osmolality is usually low, manifesting as dilute urine.1 These patients include those with congestive heart failure and cirrhosis with volume overload and chronic oliguric renal failure. These patients may present with hypoxic respiratory failure, pulmonary edema, B-lines on point-of-care ultrasound, and congestive hepatopathy. Their ADH is appropriately suppressed due to hypervolemia or is non-functional due to kidney disease.1
#5: Treat
For euvolemic or volume-depleted patients, give 3% saline. For intravascularly volume-up patients, focus on escalating diuresis.1 Serum sodium is raised slowly, typically no faster than 0.5mmol/L/hr or 4-8mmol/L in 24 hours to avoid osmotic demyelination syndrome.3 Giving 100-150mL 3% NaCl boluses versus continuous infusion is debated.6,7 Consider emergency department staffing for frequency and reliability of correction rate monitoring. Ideally, check every 2-4 hours. 3% NaCl bolus may be safer when monitoring and timing are difficult to control. Infusion rates derived from the Adrogué-Madias formula are found online.
Overcorrection: The Resuscitationist’s Rescue
Remain vigilant against overcorrection in hyponatremic patients who received a fluid bolus and who begin auto-diuresing. The first indication will be dilute urine at the proximal foley and large amounts of urine output, essentially free water, which causes the serum sodium to rise quickly.1 Overcorrection can also occur with intentional diuresis of hypervolemic patients. In this case, administration of desmopressin (DDAVP), an ADH analogue, can be administered in 2mcg IV doses every 8 hours as needed to prevent free water loss and slow sodium correction.8,9 After 1-2 hours, the effectiveness of DDAVP can be reassessed by examining the urine at the proximal foley which should demonstrate darker, more concentrated urine. Serum sodium and urine osmolarity should be assessed every 2 hours. If the serum sodium is still rising, give D5W to further slow correction.1,2 Maintain sodium correction to 0.5mmol/L/hr or lower sodium by this same rate to the initial correction goal of 4-8mmol/L in 24 hours.3 For the average 70kg person, a rate of 170cc/hr of D5W generally corrects serum sodium by 0.5mmol/L/hr.5
References
- Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol 2014;170(3):G1-47.
- Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med 2013;126(10 Suppl 1):S1-42.
- Sterns RH, Hix JK, Silver SM. Management of hyponatremia in the ICU. Chest 2013;144(2):672–9.
- Peri A. Management of hyponatremia: causes, clinical aspects, differential diagnosis and treatment. Expert Rev Endocrinol Metab 2019;14(1):13–21.
- Adrogué HJ, Madias NE. Hypernatremia. N Engl J Med 2000;342(20):1493–9.
- Baek SH, Jo YH, Ahn S, et al. Risk of Overcorrection in Rapid Intermittent Bolus vs Slow Continuous Infusion Therapies of Hypertonic Saline for Patients With Symptomatic Hyponatremia: The SALSA Randomized Clinical Trial. JAMA Intern Med 2021;181(1):81–92.
- Tran LK, Marino KK, DeGrado JR, Szumita PM, Dube KM. Evaluation of Desmopressin in Critically Ill Patients with Hyponatremia Requiring 3% Hypertonic Saline. Am J Med Sci 2021;361(6):711–7.
- MacMillan TE, Cavalcanti RB. Outcomes in Severe Hyponatremia Treated With and Without Desmopressin. Am J Med 2018;131(3):317.e1-317.e10.
- Sood L, Sterns RH, Hix JK, Silver SM, Chen L. Hypertonic saline and desmopressin: a simple strategy for safe correction of severe hyponatremia. Am J Kidney Dis 2013;61(4):571–8.
Sarah Perez, MD