
Acute Liver Failure Case
Kimberly Pistell, DO
LCDR MC USN
Introduction
Acute liver failure is not a common condition seen in the ER, but it is important to recognize and treat early as it has a high morbidity and mortality rate. There are approximately 2,000 cases each year in the United States.1 The standard treatment for hepatic encephalopathy secondary to liver failure includes lactulose and rifaximin- both which reduce the amount of ammonia in the gut, and hemodialysis to help remove ammonia from the blood. What if your patient is too unstable for dialysis? How else can you treat their hyperammonemia? I would like to present a case of acute liver failure that was ultimately treated with a relatively inexpensive medication that is better known for its role as a food preservative.
Case
A 56-year-old female was brought into the emergency room for altered mental status and yellowing of the skin. She was found at home by a coworker after not showing up to work for two days. She was taking amlodipine for hypertension and a multivitamin. Pertinent exam findings included jaundice, mild diffuse abdominal tenderness without ascites, asterixis, and confusion. Her workup in the ER was notable for a transaminitis int the 800s, a total bilirubin of 4.5 mg/dL, a mild AKI, mild hyponatremia (132 mEq/L), an ammonia “unable to result”, with a negative tox and ethanol screening. She was diagnosed with acute liver failure and admitted to the ICU, where she rapidly deteriorated, requiring intubation and vasopressors. At this point, she had already been started on lactulose, rifaximin, and broad-spectrum antibiotics. An EEG showed generalized slowing. Hyperammonemia was the suspected cause of this presentation, with an unknown ammonia level. The pathologist was consulted to obtain approval for the lab to dilute the ammonia level down to an interpretable level, which resulted in a verbal report of “likely greater than 1000-2000” after the sample was diluted by 100x. Ammonia is neurotoxic, leading to cell death, cerebral edema, and ultimately herniation, which is what makes acute liver failure such a dangerous condition. While ammonia levels do not always correlate with the severity of signs and symptoms, concentrations > 150-200 umol/L correlate with increased intracranial pressure and herniation. Levels > 200-500 umol/L are associated with poor neurologic outcome and death.2
Acute Liver Failure
The features that define liver failure are 1. Severe acute liver injury with no prior history of liver disease. Timing varies by resources, with some defining acute as anything less than 26 weeks. 2. Impaired synthetic function (INR > 1.5). 3. Altered mental status. The causes are numerous, with acetaminophen overdose being the leading cause in developed countries, and viral hepatitis the leading cause in Asia and Africa. Other less common causes include toxins, ischemia, drug reaction, autoimmune hepatitis, heat stroke, and Wilson disease.3
Hyperammonemia
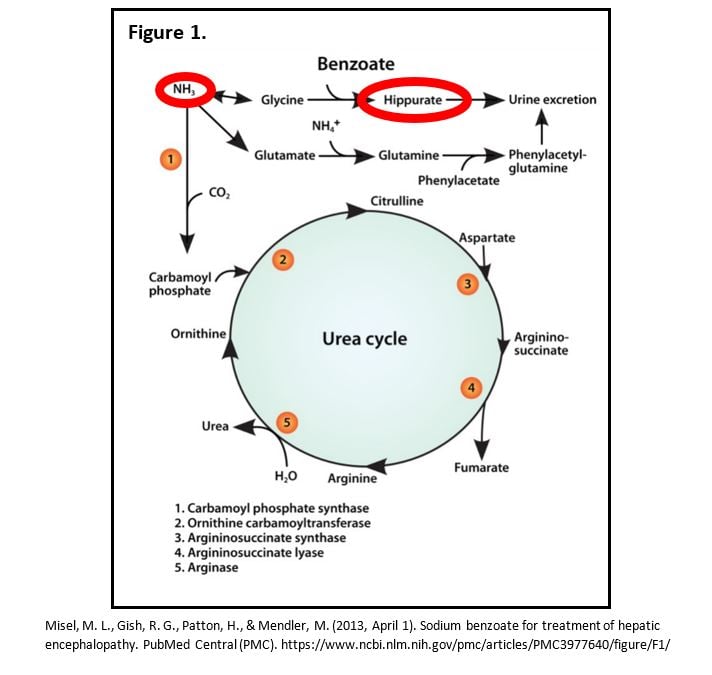
Hyperammonemia is multifactorial. Ammonia is generated in the intestine as a result of bacterial breakdown of dietary protein and urea in the colon by urease-containing bacteria, as well as the metabolism of glutamine in the wall of the small intestine. Liver damage prevents the ammonia from being converted to urea. Ammonia metabolism is further impaired in patients with muscle wasting and kidney dysfunction. Standard treatments for liver failure include medications that aim to reduce the amount of ammonia absorbed-lactulose and rifaximin, which may not be as useful to treat hepatic encephalopathy in the acute setting.4 Lactulose impairs absorption of ammonia and has a cathartic effect of the gastrointestinal tract. Rifaximin reduces intestinal bacterial production of ammonia.5 Both lactulose and rifaximin reduce the amount of ammonia absorbed in the intestine, but the toxicity is related to the high levels of ammonia circulating in the blood and tissue. Ammonia is a small molecule that is not largely protein bound, making it amenable to dialysis. Renal replacement therapy (RRT) would remove the ammonia from the blood, although rapid shifts can cause worsening cerebral edema. A continuous mode would avoid the large metabolic and hemodynamic fluctuations associated with intermittent RRT, which could worsen an already increased intracranial pressure.4 Our patient was not a candidate for RRT due to risk of herniation from rapid osmotic shifts and medical futility in a patient that was given a very poor prognosis. Liver transplant was considered, but our patient was too unstable.
Alternative Treatments
There are several case reports for alternative treatments to acute hepatic encephalopathy discussing the use of sodium benzoate, a common food preservative. It is also used as long-term treatment in urea-cycle disorders. The case reports found that sodium benzoate is at least as effective as lactulose, at a significantly reduced price-lactulose costs approximately 30 times that of sodium benzoate.6 Sodium benzoate provides an alternate pathway for the degradation of nitrogen waste, forming hippurate, which is cleared in the urine, and can also be cleared with hemodialysis.5 It reduces the amount of ammonia levels in the serum and tissue where it exerts its toxic effects. Since sodium benzoate is not commonly used as a medication, we had to obtain it from a nearby hospital. Some resources recommend a loading dose of 5.5 g/m2 IV over 90 min, followed by a maintenance dose of 55 g/m2 IV over 24 hours. Continue maintenance infusions until elevated plasma ammonia levels have been normalized or patient can tolerate oral nutrition and medications.7
Case Resolution
Our patient had significant improvement over the next 24 hours after receiving a combination of lactulose, rifaximin, and sodium benzoate. Five days later, she was extubated with resolution of her liver failure. She was transferred out of the ICU and underwent further testing to find the underlying etiology of her acute liver failure.
Key Points
- Acute-ACUTE-liver failure is an emergency. Start thinking ahead and consider liver transplant early in the course.
- Always follow up on unclear lab values, especially ones that may alter your course.
- Treat early and aggressively. Time is tissue.
- Think outside of the box. Look for case reports or alternative treatments.
- Advocate for your patient. In our case, I may have pushed for CRRT after our patient was denied hemodialysis.
Resources
- Acute liver Failure | Cleveland Clinic. (n.d.). Cleveland Clinic. https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/acute-liver-failure#incidence-tab
- Gupta, S., Fenves, A. Z., & Hootkins, R. (2016). The role of RRT in hyperammonemic patients. Clinical Journal of the American Society of Nephrology, 11(10), 1872–1878. https://doi.org/10.2215/cjn.01320216
- Acute liver failure in adults: Etiology, clinical manifestations, and diagnosis - UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/acute-liver-failure-in-adults-etiology-clinical-manifestations-and-diagnosis?search=liver%20failure&source=search_result&selectedTitle=2%7E150&usage_type=default&display_rank=2#H4
- Liver, E. A. (2017). EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. Joural of Hepatology, 1047-1081.
- Misel, M. L., Gish, R. G., Patton, H., & Mendler, M. (2013, April 1). Sodium benzoate for treatment of hepatic encephalopathy. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3977640/
- Sushma, S., Dasarathy, S., Tandon, R., Jain, S., Gupta, S., & Bhist, M. S. (1992). Sodium benzoate in the treatment of acute hepatic encephalopathy: A double-blind randomized trial. Hepatology, 16(1), 138–144. https://doi.org/10.1002/hep.1840160123
- Sodium benzoate / Sodium phenylacetate Dosage Guide + Max dose, Adjustments. (n.d.). Drugs.com. https://www.drugs.com/dosage/sodium-benzoate-sodium-phenylacetate.html



