Bupropion overdose: Suicide attempt or recreational disaster?
Case
A 33-year-old male with past medical history of substance abuse presented to the emergency department for bupropion overdose. He was last seen normal prior to going to bed. Just prior to arrival his girlfriend woke to find him sitting up against a wall in the bedroom with multiple empty bottles of bupropion XL. The bottles were reported as being half full, with a maximum potential dose of up to 6.75 g of bupropion XL. He appeared altered, had pill residue in both nares and on his lips, and was noted to have brief, generalized, seizure-like activity lasting less than 10 seconds that extinguished on its own.
On arrival the patient was alert but disoriented to place and time. He was afebrile, mildly hypertensive and tachycardic, non-tachypneic, and saturating normally on room air. On physical exam his pupils were 3 mm equal round and reactive, no nystagmus was noted, his tone was normal, but he had non-extinguishing clonus of his lower extremities. His initial EKG showed sinus tachycardia with a rate of 111, normal QRS duration, and a QTc of 474 ms. Initial lactate was 5.1 and a leukocytosis was present to 11.6, likely secondary to seizure activity. Labs were otherwise unremarkable, no electrolyte abnormalities were present, urine toxicology screen was negative, and serum ethanol, acetaminophen and salicylate levels were undetectable.
About 2 hours after arrival to the emergency department the patient had another generalized tonic-clonic seizure and was given lorazepam 1mg IV with cessation of seizure activity. Given concern for continued seizure activity and worsened mental status, the patient was then intubated for airway protection and sedated with propofol. He was admitted to the medical ICU.
While in the ICU, the patient did not experience further seizure activity. His QTc peaked at 504 but, he remained in sinus rhythm. Neurology was consulted for new onset seizure activity. Head CT was performed and read as normal. EEG indicated lowered seizure threshold with propensity for focal seizures in the right temporal region and was suggestive of severe encephalopathy. After 2 days in the ICU, the patient was extubated to nasal cannula and transferred to floor level of care. Collateral information gathered from the patient’s psychiatrist indicated that he was most likely attempting to get high and that this was unlikely to have been a suicide attempt. He was discharged on the 3rd day of his hospital stay with instructions to follow up with his primary care physician and psychiatrist in one week.
Bupropion Overdose
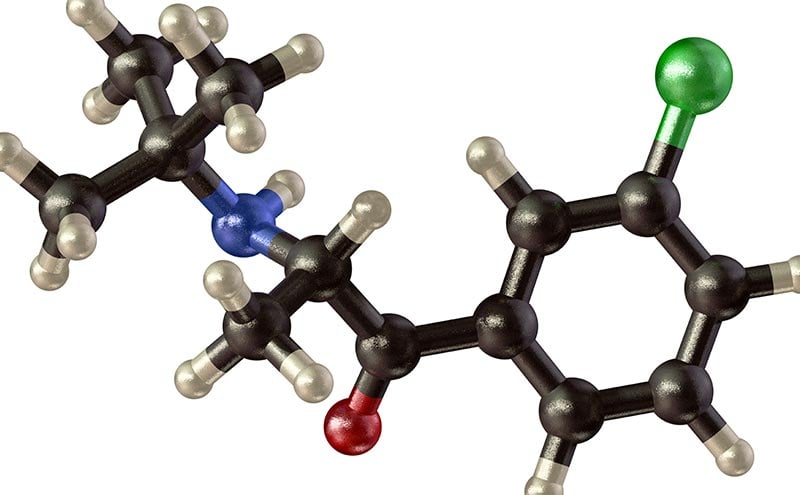
Initially investigated by Burroughs Wellcome in the 1970’s as a potential anti-depressant, bupropion is an N-tert-butyl analogue of cathinone, the naturally occurring stimulant found in khat [1]. Bupropion is structurally related to numerous drugs of abuse including amphetamine, methamphetamine (“crystal meth”), methylenedioxypyrovalerone (MDPV or “bath salts”), and methylenedioxymethamphetamine (MDMA or “ecstasy”). Bupropion exerts its antidepressant actions via inhibition of dopamine and norepinephrine reuptake, and has antagonistic activity at the nicotinic acetylcholine receptor. In contrast to many other antidepressants, bupropion has minimal serotonergic activity.
Therapeutic doses of bupropion (150-300 mg daily) are generally well tolerated with the most common side effects being dry mouth and insomnia. At higher doses, bupropion causes a wide range of toxic effects similar to the effects produced by its related drugs of abuse. In mild to moderate toxic doses it produces agitation, hallucination, tachycardia, tremor, and single episodes of seizure. In severe toxic doses it can cause coma, hypotension, multiple seizures, QRS widening, QTc prolongation, status epilepticus, and ventricular dysrhythmias [2].
Seizure due to intentional or unintentional overdose is among the most commonly reported toxic effect of bupropion [3–6]. In the vast majority of cases, bupropion induced seizure is preceded by a prodrome with agitation, tremor, or hallucination occurring prior to seizure [7]. The incidence of seizure is dose dependent, with seizure occurring with higher frequency at higher doses [8,9]. Bupropion is a significant cause of drug induced seizure. A retrospective review of drug-induced seizure reported to a state-wide poison control center system found that bupropion overdose accounted for the largest share of reported seizure activity at 23% [10]. Of the total number of reported cases of bupropion induced seizure in this study, 63.3% were single episodes of seizure, 31.8% were multiple discrete episodes of seizure, and 4.5% progressed to status epilepticus [10].
Recreational use and abuse
The inhibitory activity of bupropion on dopamine reuptake would seem to suggest addictive potential similar to that of cocaine or amphetamines. However, early studies of bupropion provided evidence to the contrary. In comparison to dextroamphetamine, doses of bupropion ranging from 50-400 mg did not produce the same behavioral or peripheral sympathomimetic effects seen with 5-10 mg of dextroamphetamine [11,12]. The lack of sympathomimetic effects in these studies was likely dose related, as bupropion is generally well tolerated with standard therapeutic dosing.
Reports of recreational bupropion use surfaced in 2002, nearly two decades after its original FDA approval for the treatment of depression [13,14]. The first reported case involved a 13-year-old girl with a history of drug experimentation, that ingested a total dose of 600 mg orally after being told it would give her a “better high than amphetamine.” No adverse effects were reported and she was discharged after 16 hrs of observation [14]. The second case involved a 16-year-old boy with a history of marijuana and alcohol use, that crushed and insufflated six 150 mg bupropion tablets resulting in generalized tonic-clonic seizure. He reported previous insufflation of two or three crushed tablets that provided a brief “buzz” [13]. Since that time, numerous case reports of recreational use have been published of users that have ingested, nasally insufflated, or injected bupropion. Bupropion abuse is particularly prevalent in correctional facilities and in those with a history of both drug abuse and incarceration. One reported case of seizure related to nasal insufflation involved a 38-year-old man who indicated learning this method while incarcerated [15]. Among those who regularly abuse bupropion it has been referred to as “jailhouse coke,” “wellies,” “dubs” (for W), or “Barnies” given the purple color of some bupropion formulations [16,17].
Bupropion has been noted to induce a high similar to that of cocaine but of lesser intensity. Orally ingested bupropion undergoes extensive first pass hepatic metabolism to three metabolites: hydroxybupropion, erythrohydrobupropion, and threohydrobupropion [2]. The most active of these metabolites, hydroxybupropion, has only half the activity of bupropion [2]. Recreational use of bupropion via nasal insufflation or IV injection bypasses first pass metabolism producing a more intense effect than with oral ingestion. Bupropion use via intravenous injection is particularly problematic as it can cause vascular damage and tissue necrosis. Venous insufficiency and arterial occlusion resulting in severe pain, tissue ischemia and necrosis have both been described as being caused by bupropion [17].
Conclusion
Bupropion overdose is a well-known cause of seizure with potential deadly cardiovascular effects in extreme overdose [18,19]. While suicidal ideation is certainly an important consideration with overdose, this case illustrates the abuse potential of prescription drugs not generally thought of as dugs of abuse. Bupropion in particular possess dopaminergic and noradrenergic activity making it an attractive choice for those seeking a cocaine like high. Bupropion is both cheaper and easier to obtain than illicit substances like amphetamines and cocaine, and should be on our radar as a potential drug of abuse.
- 1. Baumann MH, Walters HM, Niello M, Sitte HH. Handbook of Experimental Pharmacology. 2018;1–30.
- Brown KM, Crouch BI. Bupropion Overdose: Significant Toxicity in Pediatrics. Clin Pediatric Emerg Medicine. 2017;18:212–7.
- Rivas-Coppola MS, Patterson AL, Morgan R, Wheless JW. Bupropion Overdose Presenting as Status Epilepticus in an Infant. Pediatr Neurol. 2015;53:257–61.
- Jepsen F, Matthews J, Andrews F. Sustained release bupropion overdose: an important cause of prolonged symptoms after an overdose. Emerg Med J. 2003;20:560–1.
- Mainie I, McGurk C, McClintock G, Robinson J. Seizures after bupropion overdose. Lancet. 2001;357:1624.
- Storrow AB. Bupropion overdose and seizure. Am J Emerg Medicine. 1994;12:183–4.
- Shepherd G, Velez LI, Keyes DC. Intentional bupropion overdoses. J Emerg Medicine. 2004;27:147–51.
- Johnston J, Lineberry C, Ascher J, Davidson J, Khayrallah M, Feighner J, et al. A 102-center prospective study of seizure in association with bupropion. J Clin Psychiatry. 1991;52:450–6.
- Dunner D, Zisook S, Billow A, Batey S, Johnston J, Ascher J. A prospective safety surveillance study for bupropion sustained-release in the treatment of depression. J Clin Psychiatry. 1998;59:366–73.
- Thundiyil JG, Kearney TE, Olson KR. Evolving epidemiology of drug-induced seizures reported to a poison control center system. J Medical Toxicol. 2007;3:15–9.
- Miller L, Griffith J. A comparison of bupropion, dextroamphetamine, and placebo in mixed-substance abusers. Psychopharmacology. 1983;80:199–205.
- Peck A, Bye C, Clubley M, Henson T, Riddington C. A comparison of bupropion hydrochloride with dexamphetamine and amitriptyline in healthy subjects. Brit J Clin Pharmaco. 1979;7:469–78.
- Welsh CJ, Doyon S. Seizure Induced by Insufflation of Bupropion. New Engl J Medicine. 2002;347:951–951.
- McCormick J. Recreational bupropion abuse in a teenager. Brit J Clin Pharmaco. 2002;53:214–214.
- Paggio D. Psychotropic medication abuse in correctional facilities. Psychopharmacology Newsletter. 8.
- Hilliard WT, Barloon L, Farley P, Penn JV, Koranek A. Bupropion Diversion and Misuse in the Correctional Facility. J Correct Health Car. 2013;19:211–7.
- Strike M, Hatcher S. Bupropion Injection Resulting in Tissue Necrosis and Psychosis. J Addict Med. 2015;9:246–50.
- Morazin F, Lumbroso A, Harry P, Blaise M, Turcant A, Montravers P, et al. Cardiogenic shock and status epilepticus after massive bupropion overdose. Clin Toxicol. 2009;45:794–7.
- Franco V. Wide complex tachycardia after bupropion overdose. Am J Emerg Medicine. 2015;33:1540.e3-1540.e5.
Marc Rigatti, MD, PhD
University of Connecticut, Emergency Medicine Residency



