The Use of Low Titer Group O Whole Blood for TEMS
Introduction
The job of the tactical law enforcement officer (LEO) is inherently dangerous. Tactical teams throughout the US in the last two decades have begun to more heavily rely on specially trained paramedics and physicians to provide immediate life-saving treatments at the point-of-injury (POI) prior to extraction to safety and staging traditional EMS units.
Many of the advances in tactical emergency medical services (TEMS) can be attributed to Tactical Combat Casualty Care (TCCC). Born from TCCC, its civilian counterpart, Tactical Emergency Casualty Care (TECC) has greatly influenced how TEMS conducts and provides casualty care in the civilian setting. Across combat and tactical medicine, hemorrhage control and the prevention/treatment of hemorrhagic shock have made a significant impact.1-4
In 2014, the TCCC guidelines for fluid resuscitation in hemorrhagic shock changed to recommending whole blood (WB) as the fluid of choice.5 The[KMOP1] methods for the process of utilizing low titer group O whole blood (LTOWB) at the point of injury (POI) have previously been described.3,4 It is these lessons learned from combat that have substantially changed the approach and treatment of hemorrhagic shock patients within Emergency Medicine Services (EMS). Currently, there are several prehospital programs (helicopter and ground EMS) that are utilizing cold – LTOWB.5,6 However, the question remains, how can LTOWB be best implemented for TEMS at the POI?
Background
The use of LTOWB dates back to World War II. During this time, a study was conducted using group O plasma on healthy volunteers at the Colorado State Penitentiary, to determine what titers would elicit a reaction.10 With this data, Maj. Leslie H. Tisdall determined that group O blood was safe at titers below 1:200.10 Around the same time, the American Red Cross Blood Donor Service determined from pools of donated plasma that group O blood was safe at titers below 1:250.10 Though correlation between antibody levels and risk of hemolysis is imprecise, these antibodies can be measured in the lab setting in order to identify low risk FWB donors.8 In 1944 a group A patient received 75 mL of group O blood with an IgM anti—A titer of 8000. This along with similar reactions caused the US Army to state low titer was < 1:250.12 This practice was carried over to the Korean War, where over 400,000 units of LTOWB were transfused, without a significant reaction.12 Currently, there is no universally accepted definition of “low titer.” Within the United States, “low titer” is IgM anti—A and anti—B and can range from 1:150 – 1:250.
Low Titer Group O Whole Blood at the Point of Injury
LTOWB can be administered as cold – LTOWB or fresh – LTOWB. While the use of fresh – LTOWB has yet to be officially implemented, there are tactical teams with programs in development. It remains unclear that if this practice becomes implemented, if it will be accepted as a safe and a valid means to provide prehospital resuscitation. However, due to the tactical situation, availability, and location, fresh – LTOWB may be the only option.
There are several models to predict a massive transfusion, however, in the austere and tactical environment, the decision to perform a transfusion must often be made quickly. Therefore, the trigger to initiate a transfusion is often based on mechanism of injury to help minimize critical thinking in an unstable environment and without the need for lab work or excessive metric data. The injuries that initiate a transfusion protocol:13 (Figure 1)
- One or more major amputations
- Penetrating or blunt torso trauma
- Suspected pelvic fracture
- Evidence of severe bleeding
Use of LTOWB can only proceed when other critical concomitant steps are in place. It is critical that the medic or physician obtains intravenous (IV) access, but intraosseous should be considered if unable to gain IV within 1-2 IV attempts. One-gram of tranexamic acid (TXA) should be administered. Both CRASH II and MATTERs I/II demonstrated a benefit for patients administered TXA.11-13
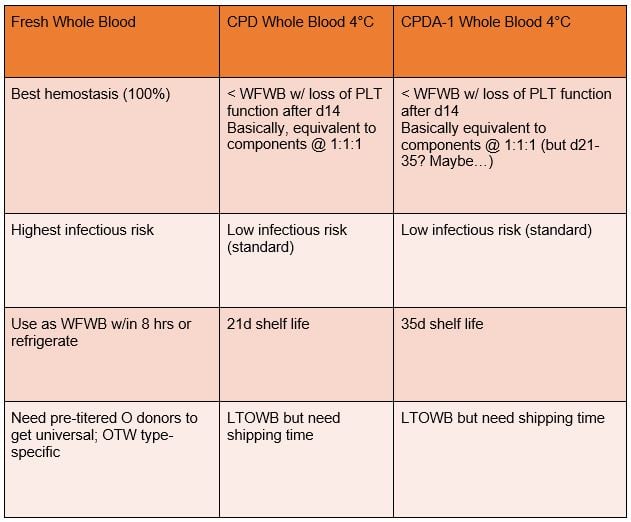
If cold – LTOWB is available, it must be stored between 1-10° C. Storage devices are available that can be placed inside an aid-bag and small adhesive devices can be attached to the unit of blood to indicate if the blood has gone above the temperature threshold. When preparing a transfusion of LTOWB, the unit must be administered using a 170-210 micron filter. There is no need to prime the administration set with a crystalloid, it is perfectly appropriate to use blood only. Currently, there are many fluid warmers on the market. Depending on the logistics, you may be able to carry or have access to the larger more effective fluid warmers. Cold – LTOWB is shelf-life is dependent on the solution in the collection bag. If collected in citrate phosphate dextrose CPD-adenine (CPDA-1) it has a 35 days shelf-life, if collected with citrate phosphate dextrose (CPD), it is limited to 21 days (Table 1).see associated figure below (Figure5).
Fresh – LTOWB is much more challenging and requires identification of low titer donors prior to operational use. Similar to the military, a LEO roster and identification card is recommended (Figure 2) along with titer testing, transfusion transmitted disease (TTD) testing is completed. In the military the identified donors, need regular TTD testing prior to deployment and are valid for 90-100 days. The universal donors will carry at least one 450 ml single blood-pack unit with CPD or CPDA-1 with them in their bleeder kit. Blood collection will begin immediately following proper identification of the donor’s full name. The TEMS medic or their designated person has the option of starting a 14- or 16-gauge saline lock and then placing the collection bag needle through the needle port (Figure 3). This offers the advantage of access for replacement fluids and less positioning of the needle, though collection can be slower. Traditional blood collection uses hemostats or similar to “clamp” the collection bag line, however, the Norwegian Naval Special Operations Commando protocol has shown that step is not necessary.14 This allows blood to immediately flow into the bag when the needle is placed inside the vein and eliminates a non-essential task.
Determining the quantity of blood in the collection bag can be difficult and previous methods with nylon banding have been flawed. A novel collection method was recently developed, by tying 5 ½-6 ½ inch paracord or similar around the circumference, it is difficult to overfill the collection bag using this method.18 The beaded cable tie is the easiest and most accurate means to use during the donation (Figure 4). Given the immediate draw and transfusion for trauma casualties, no refrigeration is necessary to maintain sterility of the blood, in addition should the scene dynamic change, the medic can hold the blood for up to six hours before needing to cool it to 1-10° C.14
Consideration for hypocalcemia must also be made in LEOs undergoing LTOWB transfusion. Blood transfusions during trauma resuscitation decrease blood calcium levels. In addition, hypocalcemia is a potential life-threating complication from citrate present in the donor bag. The effects of hypocalcemia include, long QTc, decreased cardiac output, coagulopathy, seizures, and eventually contribute to mortality. A 2015 study demonstrated 97% (n=152) of patients requiring a massive transfusion (MT) had hypocalcemia and 111 (71%) with severe hypocalcemia.16 Furthermore, 2017 study of patients receiving a MT revealed hypocalcemia occurred in 35 (85%) of the patients.17 These studies were following the general rule of giving calcium after every 4 units of blood. This guideline suggests calcium should be given early. It is recommended giving 2 grams CaCl2 or 6 grams calcium gluconate slow IV push after the first unit.
Conclusion
SWAT teams and their medics continue to make advancements in many aspects of prehospital tactical medical care and with many looking for the next steps in improved officer and civilian care at POI LTOWB transfusions must be a strong consideration. While fresh – LTOWB is superior in terms of hemostatic potential and oxygen carrying capacity, it is more feasible to carry cold – LTOWB. The use of LTOWB is a proven safe and effective option in the treatment of hemorrhagic shock. Effective implementation will require SOPs, labeling updates, and identification of a titer testing service. By ensuring proper testing and training, the FWB “battle drill” can be quickly and safely performed. By addressing the concerns, tactical teams can adapt the principles above to successfully implement and use LTOWB for use at the POI and in disasters.
References
- Eastridge BJ, Mabry RL, Seguin P, et al. Death on the battlefield (2001-2011): Implications for the future of combat casualty care. J Trauma. 2012;73(6, Supplement 5):S431-S437.
- Butler FK, Holcomb JB, Schreiber MA, et al. Fluid Resuscitation for Hemorrhagic Shock in Tactical Combat Casualty Care: TCCC Guidelines Change 14-01– 2 June 2014. J Spec Oper Med. 2014;14(3):30-55.
- Fisher AD, Miles EA, Cap AP, Strandenes G, Kane SF. Tactical Damage Control Resuscitation. Mil Med. 2015;80(8).
- Strandenes G, Berseus O, Cap AP, et al. Low titer group O whole blood in emergency situations. Shock. 2014;41 Suppl 1:70-75.
- McGinity AC, Zhu CS, Greebon L, et al. Pre-hospital Low Titer Cold Stored Whole Blood: Philosophy for Ubiquitous Utilization of O Positive Product for Emergency Use in Hemorrhage due to Injury. J Trauma Acute Care Surg. 2018;6S( Suppl 1):S115-S119.
- Dodge M, Thompson D, Bank EA, Nealy W, Fisher AD. Whole Blood in EMS May Save Lives. Journal of Emergency Medical Services. 2018(February):50-55.
- Kendrick DB. Blood Program in World War II. Washington, D.C.: Office of the Surgeon General; 1964.
- Karafin MS, Blagg L, Tobian AA, King KE, Ness PM, Savage WJ. ABO antibody titers are not predictive of hemolytic reactions due to plasma-incompatible platelet transfusions. Transfusion. 2012;52(10):2087-2093.
- Berseus O, Boman K, Nessen SC, Westerberg LA. Risks of hemolysis due to anti-A and anti-B caused by the transfusion of blood or blood components containing ABO-incompatible plasma. Transfusion. 2013;53 Suppl 1:114S-123S.
- Fisher AD, Miles EA, Cap AP, Strandenes G, Kane SF. Tactical Damage Control Resuscitation. Mil Med. 2015;180(8):869-875.
- Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Arch Surg. 2012;147(2):113-119.
- Morrison JJ, Ross JD, Dubose JJ, Jansen JO, Midwinter MJ, Rasmussen TE. Association of cryoprecipitate and tranexamic acid with improved survival following wartime injury: findings from the MATTERs II Study. JAMA Surg. 2013;148(3):218-225.
- Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with signifi cant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376.
- Strandenes G, De Pasquale M, Cap AP, et al. Emergency whole-blood use in the field: a simplified protocol for collection and transfusion. Shock. 2014;41 Suppl 1:76-83.
- Meledeo MA, Fisher AD, Peltier GC, et al. Volumetric control of whole blood collection in austere environments. J Trauma Acute Care Surg. 2017;82(6S Suppl 1):S26-S32.
- Giancarelli A, Birrer KL, Alban RF, Hobbs BP, Liu-DeRyke X. Hypocalcemia in trauma patients receiving massive transfusion. J Surg Res. 2016;202(1):182-187.
- MacKay EJ, Stubna MD, Holena DN, et al. Abnormal Calcium Levels During Trauma Resuscitation Are Associated With Increased Mortality, Increased Blood Product Use, and Greater Hospital Resource Consumption: A Pilot Investigation. Anesth Analg. 2017;125(3):895-901.
Figure 1: Prehospital Trauma Resuscitation for TEMS
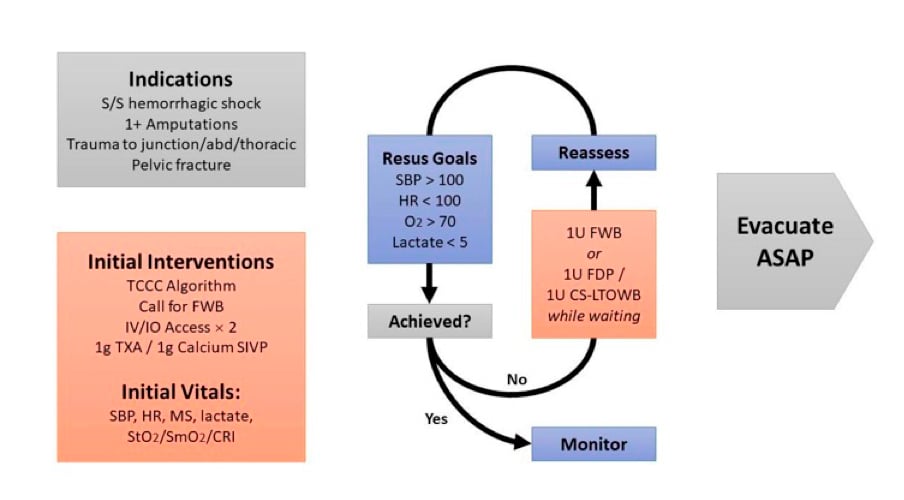
Figure 2: US Army LTOWB Donor Card
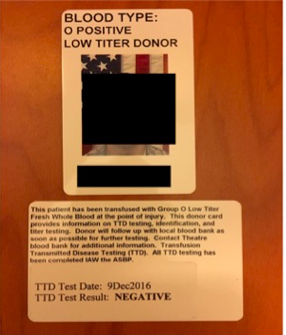
Figure 3: Alternative mean to collect a LTOWB donation

Figure 4: Beaded cable tie used to determine a full blood bag
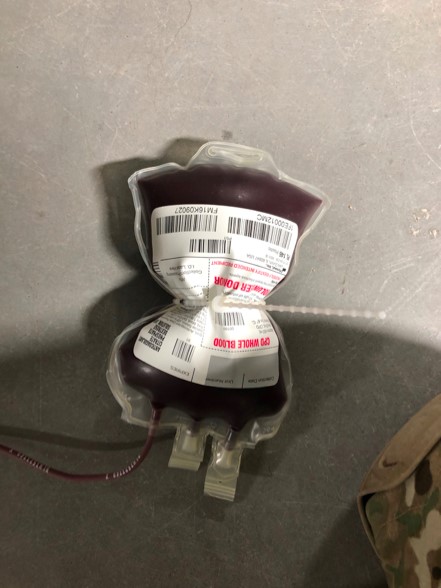
Table 1: Comparison between blood products. Adapted from Dr. Andrew P. Cap, used with permission
Andrew D. Fisher, MPAS, PA-C, LP
Medical Command, Texas Army National Guard, Austin, TX
Texas A&M College of Medicine, Temple, TX
Prehospital Research in Military and Expeditionary Environments (PRIME2)



