Thoracentesis
Michael Mirza, MD
Christopher Bryczkowski, MD, FACEP
I. Introduction
- One of the many etiologies of dyspnea in the emergency department is a pleural effusion—an abnormal collection of fluid in the pleural space.
- Removal of this fluid by needle aspiration is called a thoracentesis.
- Ultrasound allows the distinction between effusion and lung consolidations, and the diagnostic accuracy of ultrasound for pleural effusions is superior (93%), compared to auscultation (61%) and AP chest radiograph (47%), using chest CT as the reference standard.1,2
- In addition, ultrasound can precisely identify the location of the fluid so that the chest wall can be marked in preparation for thoracentesis.3
- Thoracentesis can be both diagnostic and therapeutic for the patient.
- Using ultrasound to guide this procedure can decrease the very high complication rate associated with it.3-5
Indications
- Therapeutic intervention in a symptomatic patient
- Diagnostic evaluation of pleural fluid
II. Anatomy
- The pleural space is bordered by the visceral and parietal pleura.
- Fluid in the pleural space appears anechoic and is readily detected above the brightly echogenic diaphragm when the patient is in a supine position
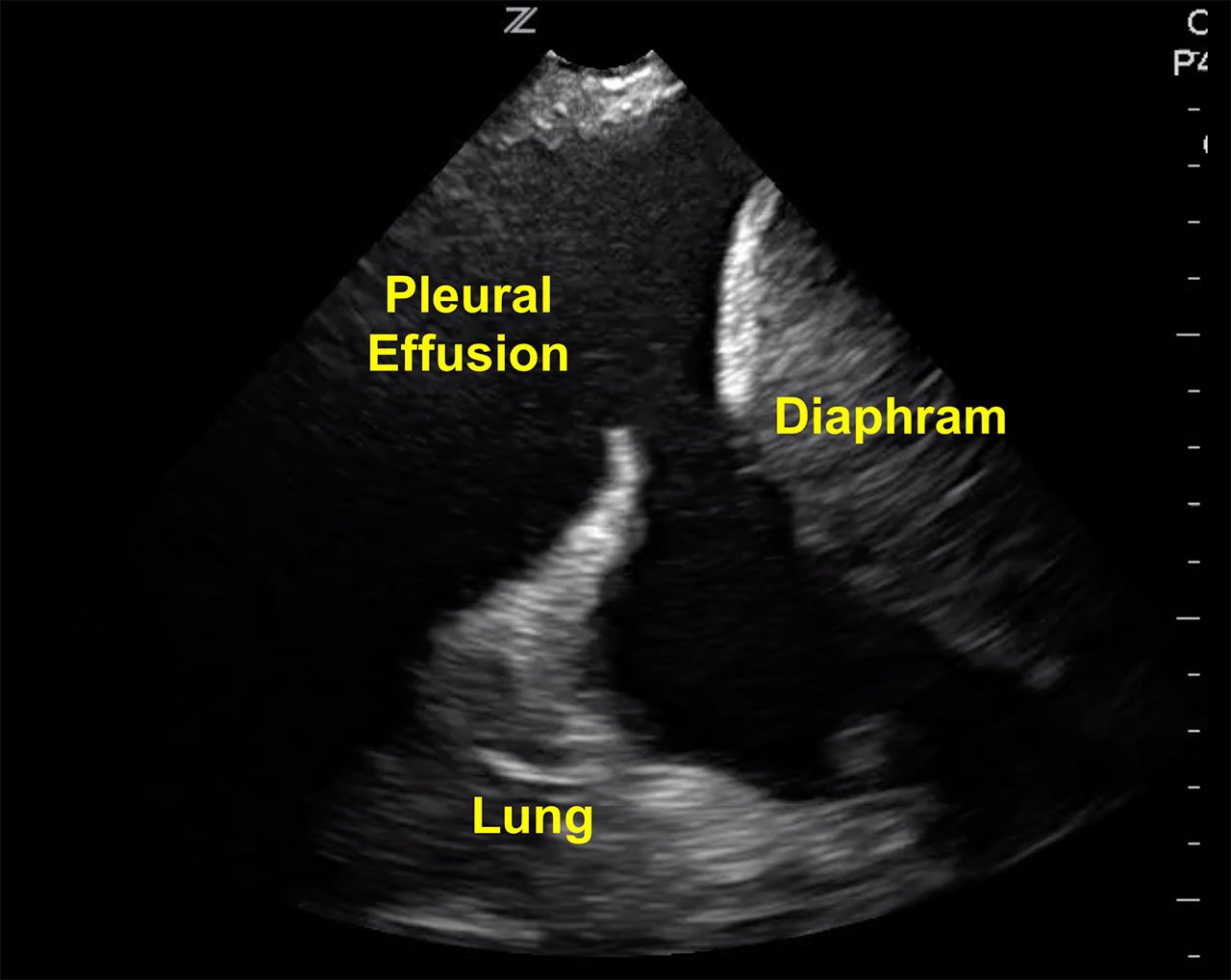
- Figure 1. Visualizing a large pleural effusion, diaphragm and liver
- Video 1. Large pleural effusion
III. Scanning Technique
- The ideal position for the patient is to sit upright leaning forward.
- A high frequency linear transducer (7.5 to 12 MHz) is the optimal choice for this procedure and placed on the patient’s back in the sagittal or transverse position.

- Figure 2. Patient in sitting position with ultrasound probe placed over the thoracentesis area
- The lung is seen as an echogenic structure moving with respiration.
- Look for the deepest pocket of fluid superficial to the lung.
- Freeze the image and take note of the maximum permissible depth of needle insertion; this will prevent puncturing the lung. (Fig. 3)
- Bear in mind that the lung is a moving structure and that the depth of fluid may vary with respiration.
- Bear in mind that the lung is a moving structure and that the depth of fluid may vary with respiration.
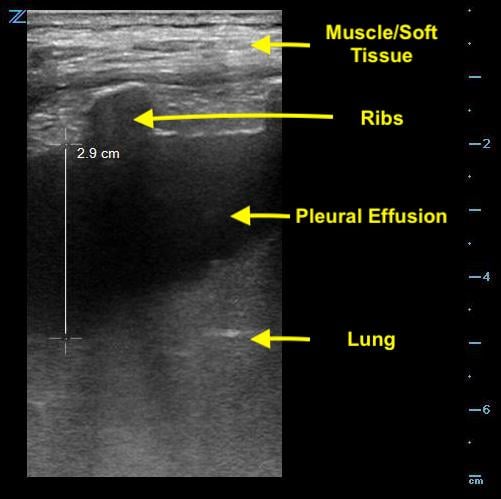
- Figure 3. Measurement of depth to lung parenchyma
- In order to visualize an effusion, the ultrasound beam will first image the chest wall, pleural line and the ribs.
- The edge of bone is echogenic and gives off a characteristic shadowing. (Fig. 4)
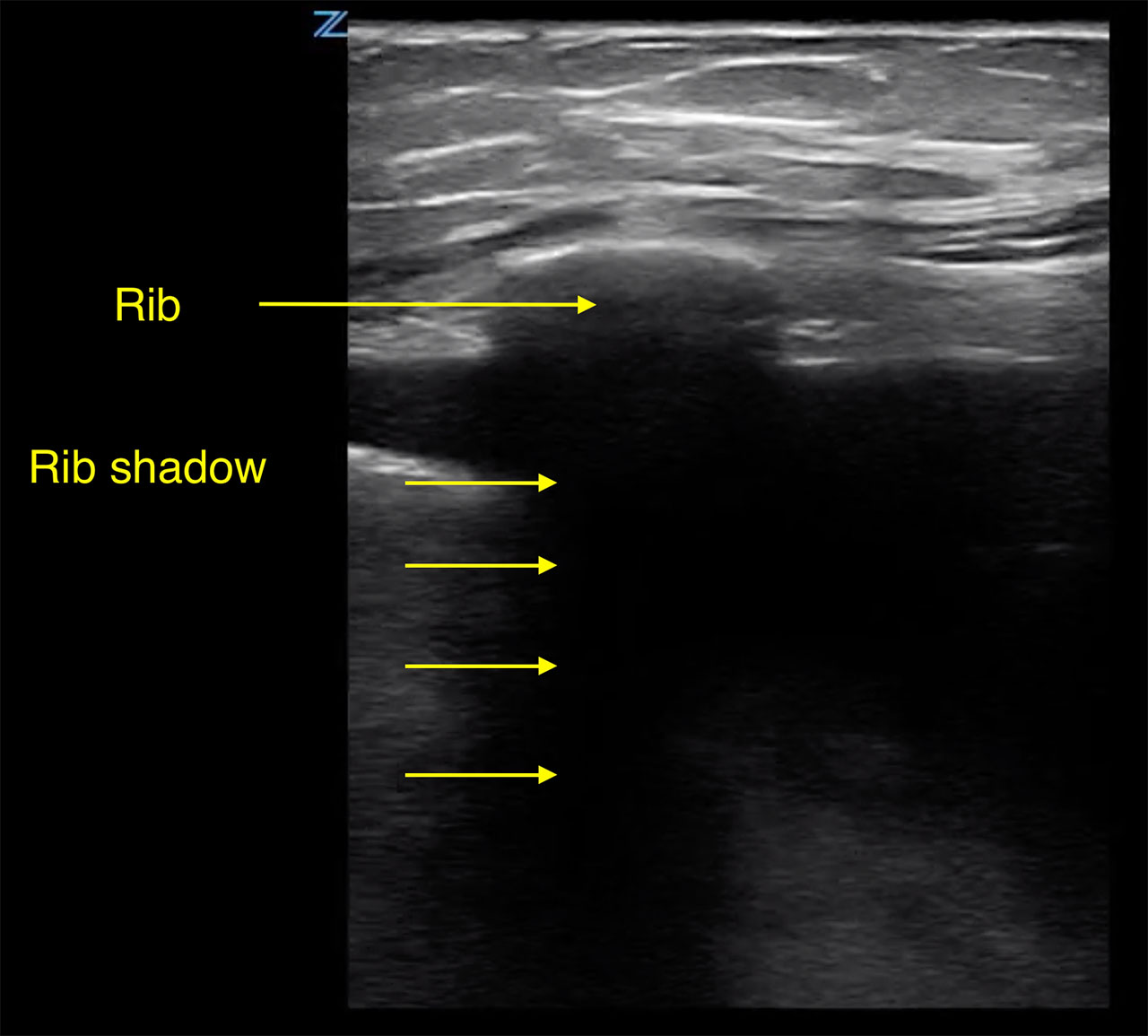
- Figure 4. Pleural effusion with rib shadow. The transducer is placed perpendicular to the axis of the rib
- The area should be marked with a pen and then prepped and draped in standard surgical fashion before the procedure is performed.
- Watch movement of diaphragm for a few respiratory cycles to determine how cephalad the diaphragm moves and mark a location for needle insertion above the that point to insure avoiding the diaphragm during the procedure.
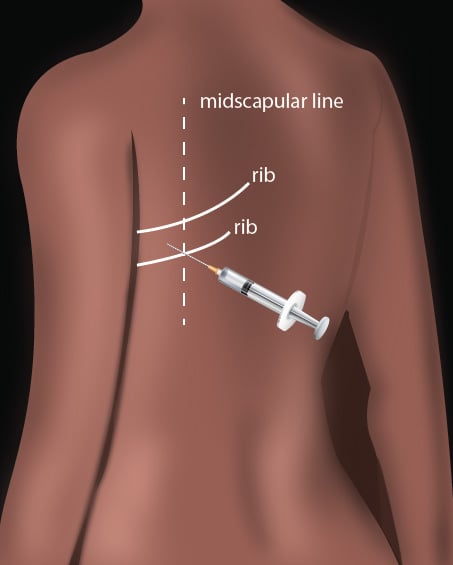
- Illustration 1. Overview of technique
IV. Pathology
- Complications can include pneumothorax, puncture of lung tissue, cystic masses, empyema or mediastinal structures.
- Incidence of pneumothorax is greatly reduced with the use of ultrasound (0.97% with ultrasound vs 8.89% without ultrasound).6
- Color flow doppler can help differentiate free-flowing effusion versus a hypoechoic mass.2
V. Pearls and Pitfalls
- Failure to identify the deepest pocket of fluid
- Failure to identify the diaphragm, avoiding intra-abdominal injury
- Failure to use this diagnostic tool for all thoracentesis procedures
- Not appreciating that the lung is a moving structure. The depth of fluid may vary with inspiration and expiration.
VI. References
- Prina E, Torres A, Carvalho CRR. Lung ultrasound in the evaluation of pleural effusion. J Brasileiro de Pneumologia. 2014;40(1):1-5.
- Soni NJ, Franco R, Velez MI, et al. Ultrasound in the Diagnosis & Management of Pleural Effusions. J Hosp Med. 2015;10(12):811-6.
- Koh DM, Burke S, Davies N, Padley SP. Transthoracic US of the chest: clinical uses and applications. Radiographics. 2002;22:e1.
- Barnes TW, Morgenthaler TI, Olsen EJ, et al. Sonographically guided thoracentesis and rate of pneumothorax. J Clin Ultrasound. 2005;33(9):442-6.
- Jones PW, Moyers JP, Rogers JT, et al. Ultrasound-guided thoracentesis: is it a safer method? Chest. 2003;123:418-23.
- Cavanna L, Mordenti P, Bertè R, et al. Ultrasound guidance reduces pneumothorax rate and improves safety of thoracentesis in malignant pleural effusion: report on 445 consecutive patients with advanced cancer. World J Surg Oncol. 2014;12:139.