Lumbar Puncture
Lumbar Puncture
Robert M. Bramante, MD, FACEP
I. Introduction and Indications
- Ultrasound guided lumbar puncture is effective in adult and pediatric patients
- Ultrasound can reduce failures and improve ease in obese patients1
- Ultrasound guided landmark identification on obese patients has more than twice the success rate compared to palpation alone.1,2 Ultrasound is effective in identifying landmark anatomy across a range of BMIs3
- Indications include any person requiring a lumbar puncture for clinical care, especially when there is difficulty palpating landmarks. There is, however, mixed evidence on whether routine ultrasound use offers benefit over a traditional landmark approach.4,5
II. Anatomy
- The most pertinent structures for ultrasound identification include the L3, L4, and L5 spinous processes and interspinous space.1,3 (Fig. 1)

- Figure 1. Sagittal view spinous processes and interspinous space (adult)
- Spinous processes appear as hyperechoic crescents with acoustic shadowing
- The ligamentum flavum, dura mater, epidural, and subarachnoid spaces can also be identified using ultrasound.1,6 These additional structures are easier to visualize in young children as bones are not yet calcified.4,6 (Video 1)
Video 1. Sagittal view of interspinous processes and spinal cord (pediatric) - Landmark height is guided by a line drawn across the superior iliac crests. Ultrasound is used to identify the midline by noting the location of the spinous processes.
III. Scanning Technique, Normal Findings and Common Variants
Scanning Technique
- Linear transducer is adequate for many patients, but a lower frequency curvilinear transducer may be necessary for deeper structures or based on body habitus.
- The patient may be positioned sitting up or in the lateral recumbent position.
- After visualizing the line formed across the superior iliac spines, scan in the transverse plane to the spinal column to identify the crescent shaped hyperechoic spinous process with underlying shadow. You may identify the paraspinal musculature on either side of this bony structure in the transverse view. (Fig. 2)
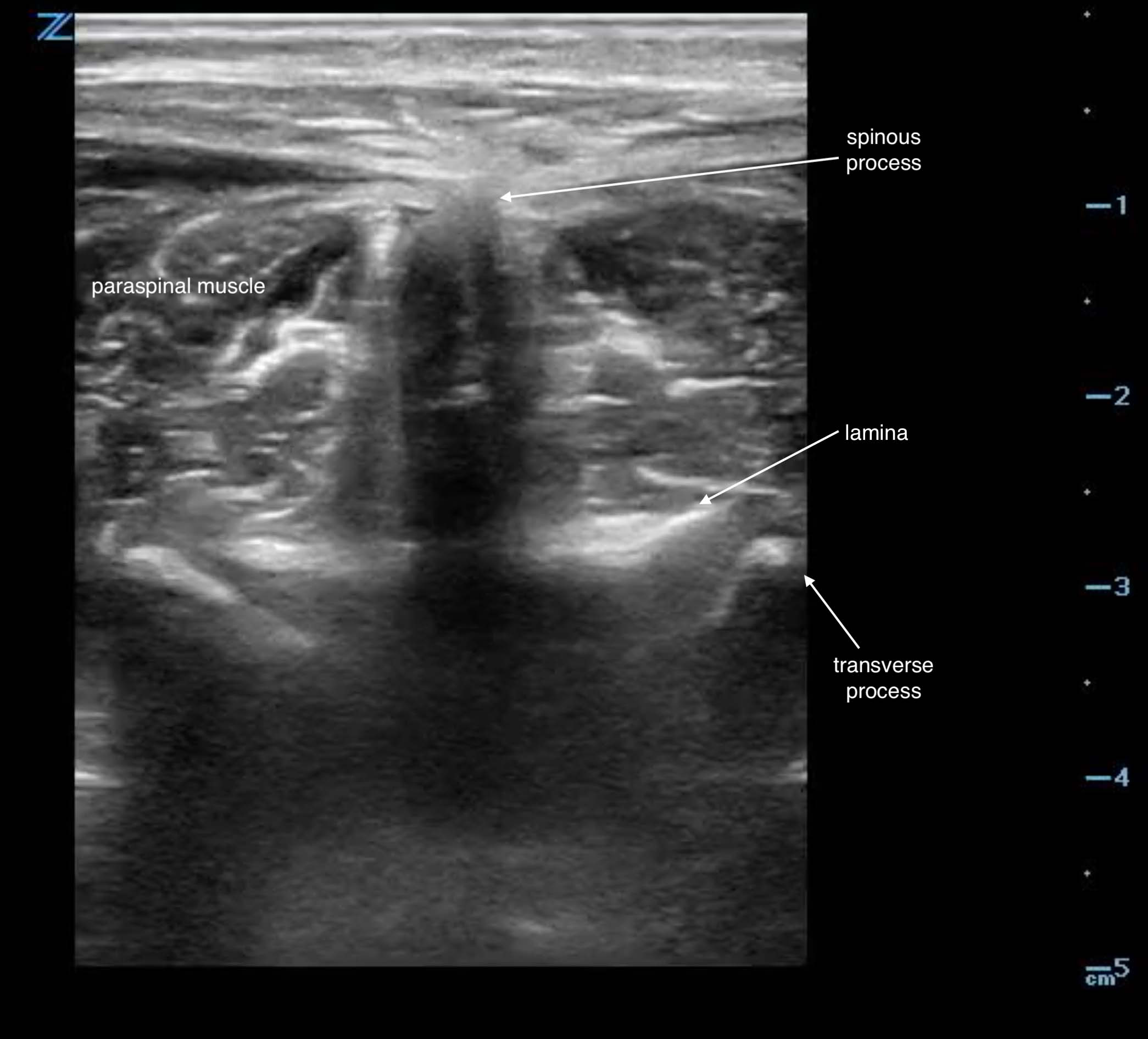
- Figure 2. Transverse view spinous process in adult
- Rotate the transducer to the sagittal plane to identify the sequential spinous process and the interspinous space. Scan caudally to identify the sacrum (a hyperechoic linear structure) (Fig. 3). This will allow you to count up from L5/S1 interspace to the L4/L5 and L3/L4 interspinous spaces.
- Mark the area in both planes. If using the static technique, you must reimage and remark this space if the patient moves or is repositioned.1,4
- The subdural space can appear as a dark space inside the vertebral column.5
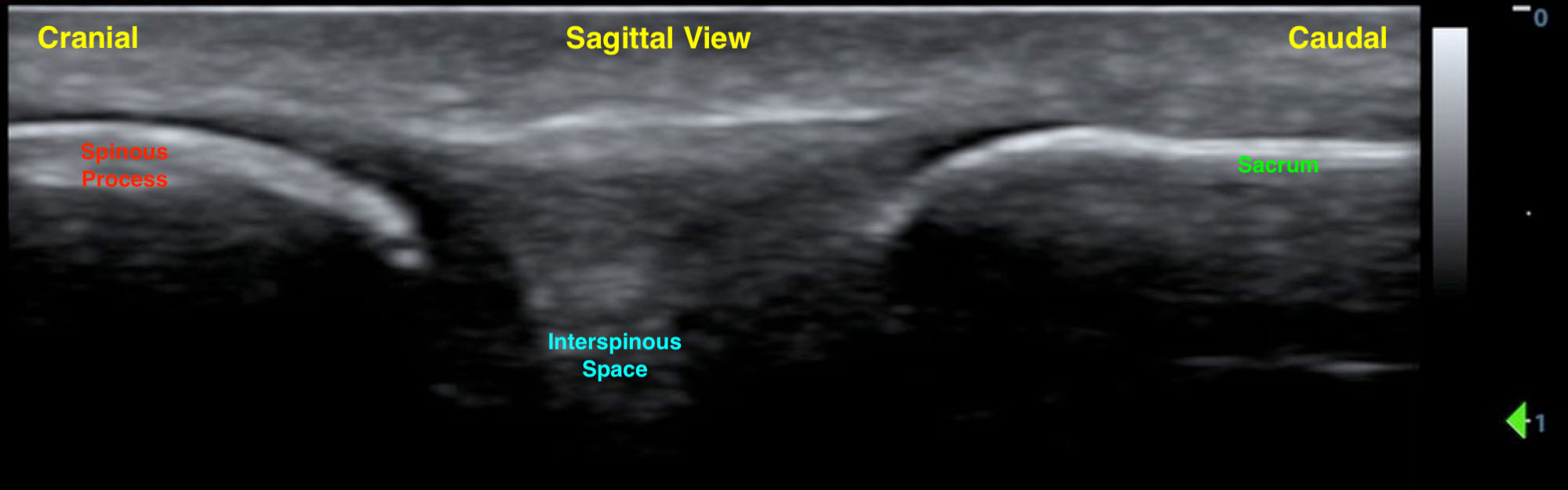
- Figure 3. Sagittal spinous process and sacrum
Positioning
- Children: Maximum interspinous space is achieved in the sitting position with flexed hips.
- If using the lateral recumbent position, hold at the shoulders as flexing the neck does not increase the interspinous distance and increases risk of hypoxia.7
- Adults: Sitting up with supported feet increases the interspinous space.8
Normal Findings
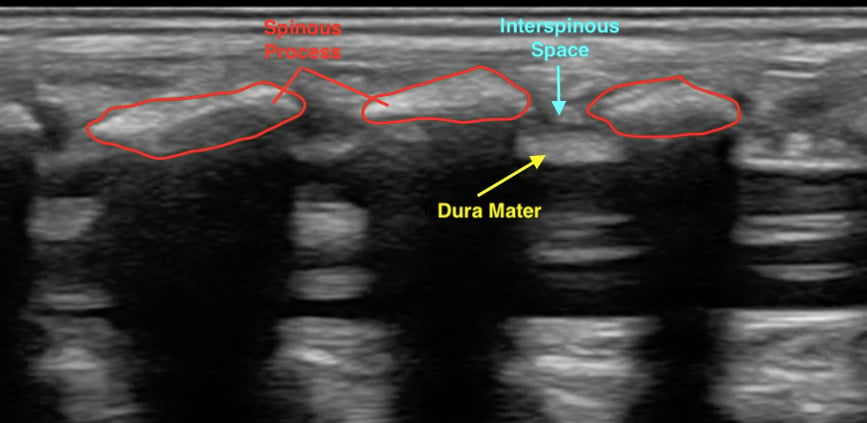
- Figure 4. Normal spinal anatomy (pediatric)
IV. Pearls and Pitfalls
Pearls
- Consider starting with the curvilinear transducer in patients with larger body habitus.
- Mark the skin with ink that will not be removed by betadine/ chlorhexidine skin preparations.
Pitfalls
- Scan slowly when searching for the midline in the sagittal plan as the hyperechoic spinous processes can be passed over.
- Scanning in the transverse plan and noting the midline initially can obviate this.
- Underestimating depth on patients with larger body habitus.
- Not rescanning and remarking the landmarks if the patient moves.
V. References
- Nomura JT, Leech SJ, Shenbagamurthi S, et al. A randomized controlled trial of ultrasound- assisted lumbar puncture. J Ultrasound Med. 2007;26(10):1341-8.
- Strony R. Ultrasound-assisted lumbar puncture in obese patients. Crit Care Clin. 2010;26(4):661-4.
- Stiffler KA, Jwayyed S, Wilber ST, et al. The use of ultrasound to identify pertinent landmarks for lumbar puncture. Am J Emerg Med. 2007;25(3):331-4.
- Peterson MA, Pisupati D, Heyming TW, et al. Ultrasound for routine lumbar puncture. Acad Emerg Med. 2014;21(2):130-6.
- Mofidi M, Mohammadi M, Saidi H, et al. Ultrasound guided lumbar puncture in emergency department: time saving and less complications. J Res Med Sci. 2013;18(4):303-7.
- Ferre RM, Sweeney TW. Emergency physicians can easily obtain ultrasound images of anatomical landmarks relevant to lumbar puncture. Am J Emerg Med. 2007;25:291-6.
- Abo A, Chen L, Johnston P, et al. Positioning for lumbar puncture in children evaluated by bedside ultrasound. Pediatrics. 2010;125(5);e1149-53.
- Sandoval M, Shestak W, Stürmann K, et al. Optimal patient position for lumbar puncture, measured by ultrasonography. Emerg Radiol. 2004;10(4):179-81.