Foreign Body Localization
Christopher Bryczkowski, MD, FACEP
I. Introduction and Indications
- Any patient presenting with a wound should always raise concern for a possible retained foreign body.
- Despite meticulous irrigation and standard x-ray imaging modalities, some foreign bodies can still be missed.
- Significant cause of wound complications & medical-legal claims1
- X-rays may not detect radiolucent objects such as: wood, plastic and organic matter.2
- CT use for foreign body detection can be time consuming, expensive and has been shown to have a low sensitivity, ranging from 0 to 60%.3,4
- Ultrasound has proven to be a valuable tool for localizing foreign bodies in soft tissue, especially those that are radiolucent.5-7
- In the hands of experienced sonologists, ultrasound for foreign body detection has been found to be 79-100% sensitive and 86-100% specific.4,6-10
- Ultrasound performed by physician and nursing trainees have been found to be 78-85% sensitive and 50-82% specific in detecting foreign bodies with minimal instruction time.10,11
Indications
- Detection of radiolucent foreign body
- Assistance and verification of foreign body removal
II. Anatomy
- The area of interest will usually be the soft tissue, most often of the feet or hands.
- Size of the foreign body is most important factor in detection.
- Very superficial objects may be very difficult to detect as sound is not transmitted nor reflected well near the transducer footprint.
III. Scanning Technique and Sonographic Findings
Ultrasound Technique
- A high frequency linear transducer (7.5 to 10+ MHz) is placed on the structure of interest.
- Using a ‘stand-off pad’ or a water bath can elevate the transducer several millimeters above the structures of interest, allowing for better sound transmission and an improved resolution of superficial soft tissues.
- Use of a water bath is an excellent medium to transmit ultrasound waves, and especially useful for areas painful to touch as it does not require direct pressure.
- Video 1. Soft tissue ultrasound in a water bath
- Stand-off pads can be made using a bag of saline, filling a glove with ultrasound gel, or purchasing commercially available ones. (Figure 1)

- Figure 1. Stand-off pad using IV fluid bag
- Use of a water bath is an excellent medium to transmit ultrasound waves, and especially useful for areas painful to touch as it does not require direct pressure.
- Foreign bodies will usually appear hyperechoic to the surrounding soft tissue.
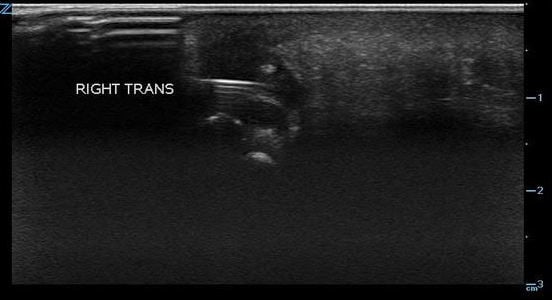
- Material such as wood, glass, and plastic tends to produce shadowing (Videos 2-4 and Figure 2) which will be visualized in the tissue deep to the foreign body.
- Video 2. Wood splinter visualized transversely causing shadowing
- Video 3. Wood splinter visualized transversely with arrow highlighting shadowing
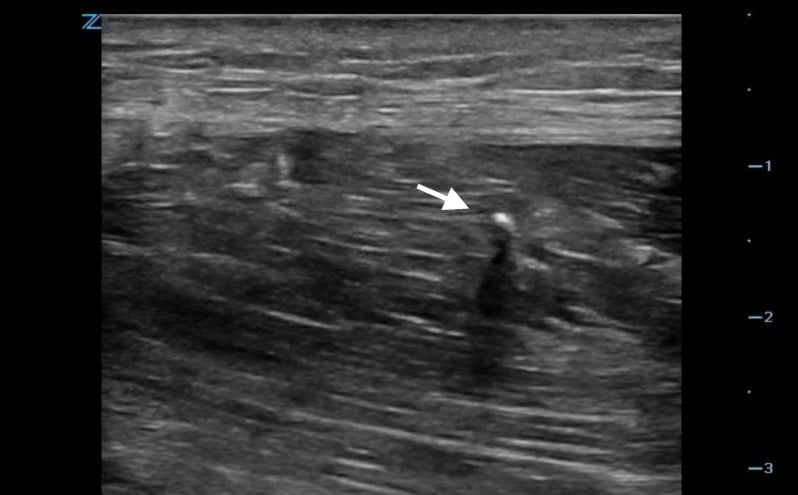
- Video 4. Glass foreign body (arrow)
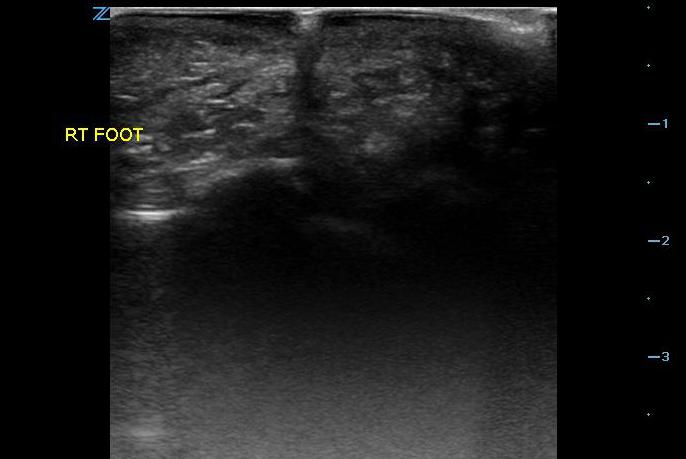
- Figure 2. Glass in foot with shadowing
- Metal objects tend to produce reverberation, comet tail artifacts or acoustic shadows (Video 5).
- Video 5. Shadowing from metal sewing needle
- Figure 3. Reverberation from metal foreign body
- Figure 4. Comet tail artifact from metal foreign body
- Material such as wood, glass, and plastic tends to produce shadowing (Videos 2-4 and Figure 2) which will be visualized in the tissue deep to the foreign body.
- The area is scanned throughout its entirety in search for a hyperechoic object in both the sagittal and transverse planes as it can sometimes be much easier to visualize an object in one plane but not the other. Be aware of possible surrounding tissue inflammation or abscess.
- Visualization of foreign bodies is easiest when the probe is parallel to the object and therefore attempts should be made to visualize the area in question from many angles if possible.
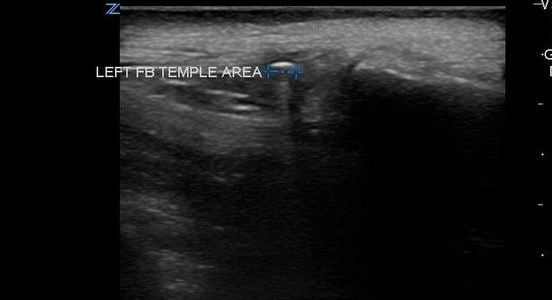
- Once a foreign body is localized, the depth from the skin can be measured as well as the size of the object.
- Survey the area surrounding the object for vessels. Vessels in close proximity to the object may prompt the practitioner to avoid probing the area.
Foreign Body Removal
- Center the transducer over the foreign body and mark the skin to identify the optimal incision site.
- Video 6. Foreign body located in soft tissue of finger using a water bath
- Ample anesthetic should be injected under ultrasound guidance.
- After making a lateral incision, image the foreign body in the long axis and insert forceps or hemostat under ultrasound towards the object.
- Video 7. Foreign body located in soft tissue with forceps using ultrasound guidance
- Video 8. Metal foreign body removed with ultrasound guidance
- If unable to remove the foreign body in the long axis view, attempt in a short axis. In general, the technique works better for linear shaped objects.
- As another option, a needle can be inserted under the foreign body in order to lift it up towards the surface of the skin or incision, where it can be grasped.
IV. Pathology
- Unsuccessful location and manipulation of the foreign body can lead to increased tissue injury, increased infection risk, and wound healing problems.
V. Pearls & Pitfalls
- Small foreign bodies may be difficult to visualize.
- Bony, articular surfaces & scars may appear hyperechoic.
- Brisk irrigation may introduce subcutaneous gas into the wound, but this does not appear to diminish the capability of ultrasonography to localize foreign bodies.12
- Inadequate knowledge of regional anatomy and failure to assess for surrounding vascular structures prior to foreign body removal can lead to potential injury.
- Detection can be time consuming.
VI. References
- Trautlein JJ, Lambert RL, Miller J: Malpractice in the emergency department—Review of 200 cases. Ann Emerg Med 13(9, Pt 1):709–711, 1984.
- Manthey DE, Storrow AB, Milbourn JM, et al. Ultrasound versus radiography in the detection of soft-tissue foreign bodies. Ann Emerg Med. 1996;28(1): p. 7-9.
- Graham DD, Jr: Ultrasound in the emergency department: Detection of wooden foreign bodies in the soft tissues. J Emerg Med. 22(1):75–79, 2002.
- Rockett MS, Gentile SC, Gudas CJ, et al. The use of ultrasonography for the detection of wooden foreign bodies in the foot. J Foot Ankle Surg. 1995;34(5):478-484.
- Crawford R, Matheson AB. Clinical value of ultrasonography in the detection and removal of radiolucent foreign bodies. Injury.1989;20:341-3.
- Hill R, Conron R, Greissinger P, et al. Ultrasound for the detection of foreign bodies in human tissue. Ann Emerg Med 29:353–356, 1997.
- Mohammadi A, Ghasemi-Rad M, Khodabakhsh M. Non-opaque soft tissue foreign body: sonographic findings: BMC Med Imaging. 2011;11(9):1-4.
- Orlinsky M, Knittel P, Feit T, et al. The comparative accuracy of radiolucent foreign body detection using ultrasonography. Am J Emerg Med. 2000;18:401-3.
- Gilbert FJ, Campbell RSD, Bayliss AP. The role of ultrasonography in the detection of non-radiopaque foreign bodies. Clin Radiol. 1990;41:109-12.
- Nienaber A, Harvey M, Cave G. Accuracy of bedside ultrasound for the detection of soft tissue foreign bodies by emergency doctors. Emerg Med Australas. 2010;22:30–4.
- Atkinson P, Madan R, Kendall R, et al. Detection of soft tissue foreign body by nurse practitioner-performed ultrasound. Crit Ultrasound J. 2014;6:2.
- Lyon M, Brannam L, Johnson D, et al. Detection of soft tissue foreign bodies in the presence of soft tissue gas. J Ultrasound Med. 2004;23:677-81.



