November 29, 2021
Paracentesis
Michael Mirza, MD
Christopher Bryczkowski, MD, FACEP
I. Introduction and Indications
- Ascites is defined as an abnormal collection of fluid within the peritoneal cavity.
- The most common cause for ascites in the United States is alcoholic liver cirrhosis.
- Although small collections of fluid may by asymptomatic, larger amounts may cause abdominal pain, nausea, anorexia and infection.
- The process of aspirating fluid from the abdomen is called paracentesis and is commonly done by emergency physicians to relieve symptoms in these patients and to retrieve fluid samples for diagnostic testing.
- This procedure is invasive and presents a risk for complications with high morbidity such as bowel perforation and infection.1,2
- Ultrasound helps to localize intra-abdominal fluid and assists in direct, real-time visual guidance of fluid aspiration.
- Ultrasound can be employed in unstable patients with a positive FAST exam. Performing an ultrasound guided paracentesis can help distinguish the identity of fluid in these emergent situations and expedite needed care.3
Indications
- Diagnostic evaluation of new-onset ascites
- Therapeutic intervention in symptomatic patients
- Diagnostic evaluation of free intra-abdominal fluid in unstable patients
- Evaluation for spontaneous bacterial peritonitis
II. Anatomy
- Intra-abdominal structures that may impede the successful aspiration of fluid include: bladder, gravid uterus, and bowel.
- The bladder is usually tucked into the pelvic recess unless full.
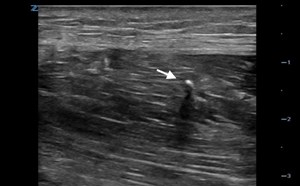
- Bowel is a moving structure that may float very close to the abdominal wall. It is usually echogenic and is visualized as an actively moving structure within the fluid, inferior to the echogenic abdominal wall musculature.
- Video 1. Ascites visualized with a linear probe
- Video 2. Ascites visualized with a curvilinear probe
III. Scanning Technique and Normal Findings - Procedure Technique
- Direct Ultrasound Guidance (Preferred method)
- A low frequency transducer (3.5 MHz) curvilinear probe or high frequency (8-12 MHz) linear probe are placed in a sterile sheath.
- It is then positioned in sagittal orientation either in the infra-umbilical or left lower quadrant of the supine patient.
- The deepest pocket of fluid is identified and a needle is inserted through the abdominal wall under real time ultrasound guidance.
- The tip of the needle is seen as a hyperechoic structure entering through the abdominal wall into the fluid and steering clear of the moving bowel and the bladder, especially with the infra-umbilical approach.
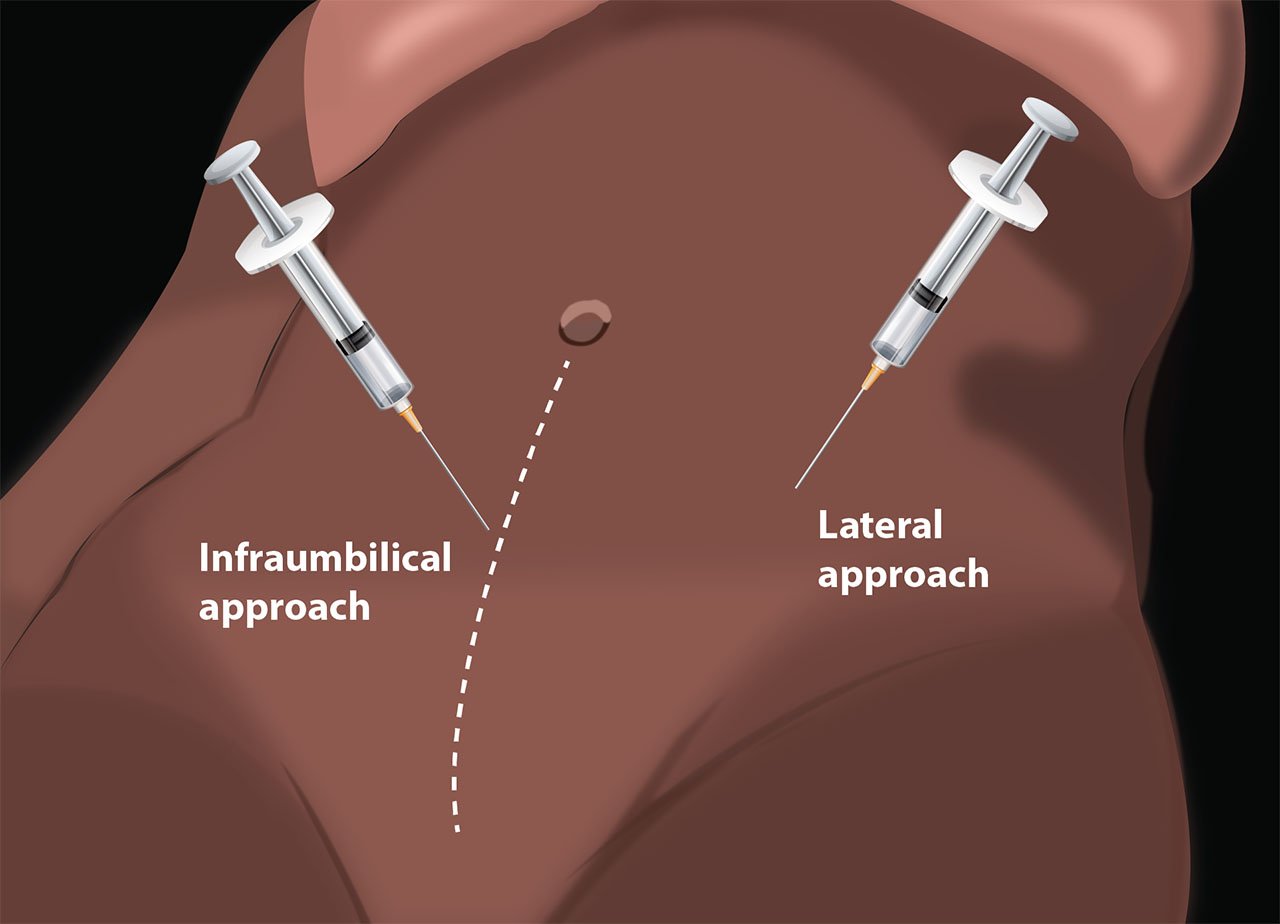
- Illustration 1. Schematic view of paracentesis needle placement
- Video 3. Paracentesis with ultrasound guidance/direct visualization
- Indirect Ultrasound Guidance
- Probe selection and set up is essentially the same as above. However, use of a probe cover may be omitted if the area is prepped & cleaned after initial scanning.
- Visualize the area with the largest pocket, and mark this with a blunt instrument (eg, cap of a needle) or skin marker.
- Subsequently, prep and drape the patient, and anesthetize this area with a wheal over the marked area.
- Recall the depth at which hypoechoic fluid was seen and advance your needle to this point while aspirating back on the syringe.
- Recall the maximum depth before which bowel was seen and be sure to not advance the needle beyond this point, preferably no more than least 1 cm anterior to this point.
- The indirect approach is quicker but is advised only for large pockets of fluid.
- If the indirect approach fails to produce a successful aspiration of fluid, direct visualization is indicated.
IV. Pathology
Complications can include bowel perforation with infection and sepsis, puncture of bladder or cystic masses.
V. Pearls and Pitfalls
- Failure to visualize the deepest pocket of fluid or having the patient switch positions after scanning fluid pockets may lead to complications.
- Insertion of needle in close proximity to bowel risks bowel perforation.
- The bladder or cystic masses may be mistaken for ascites - if possible, have the patient empty the bladder prior to the procedure.
VI. References
- Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005;23(3):363-7.
- Tibbles CD, Porcaro W. Procedural applications of ultrasound. Emerg Med Clin North Am. 2004;22:797-815.
- Blaivas M. Emergency diagnostic paracentesis to determine intraperitoneal fluid identity discovered on bedside ultrasound of unstable patients. J Emerg Med. 2005;29(4):461-5.