August 18, 2020
Abscess Evaluation
Brian D. Euerle, MD, FACEP
I. Introduction and Indications
- Abscess and cellulitis are two of the most common soft-tissue infections seen in patients treated in emergency departments. Although they sometimes occur together, they are different disease processes requiring different treatments.
- An abscess is treated with incision and drainage and might not require antibiotics; cellulitis is treated with antibiotics alone.
- It can be difficult to differentiate cellulitis from abscess based only on history and physical examination findings. Both processes can generally be characterized by warmth, erythema, tenderness, swelling, and induration.1
- In some patients, an abscess is clearly evident because of obvious fluctuance and copious purulent drainage; however, this distinct presentation is not seen in the majority of cases.
- Because of the difficulty in diagnosis, the emergency physician might decide on an inappropriate treatment, resulting in one of two possible errors. Incision and drainage might not be done in a patient with an abscess, or incision and drainage could be performed on a patient who has cellulitis but no abscess. Increased pain and poor patient outcome can result from either of these errors.
- Many researchers, including emergency physicians, have reported on the utility of ultrasound in the evaluation of abscesses and cellulitis.1-14 One group of emergency physicians found that soft-tissue ultrasound changed the management strategy for approximately half of their patients and concluded that ultrasound was useful because it could detect occult abscesses and avoid invasive procedures.6
- The use of point-of-care ultrasound has been associated with a decreased length of stay for children with soft tissue infection.14
- Ultrasound also allows many procedures to be done with greater safety. In the case of abscess drainage, ultrasound can locate adjacent structures such as large blood vessels and nerves that need to be avoided during the drainage procedure.4
- The use of bedside ultrasound can also help determine the treatment of a specific abscess based on its size and depth. If an abscess is very small (<1 cm diameter), the physician might choose treatment with antibiotics and warm compresses rather than incision and drainage.6
- Although the majority of abscesses are treated with incision and drainage, in certain cases, usually because of cosmesis, treatment with needle aspiration and antibiotics may be an option.3,7 Ozseker and colleagues7 found that ultrasound-guided aspiration and irrigation of breast abscesses was preferred to surgical drainage for abscesses with a diameter less than 3 cm.7 Ultrasound provides dynamic real-time guidance for needle aspiration, increasing the likelihood of success.
II. Anatomy
- The structures that are imaged with bedside ultrasound for abscess evaluation are primarily the skin, subcutaneous tissue, and fascia.
- The skin consists of two layers: the superficial epidermis and the deeper, thicker dermis.
- Subcutaneous tissue, located beneath the dermis, consists of connective tissue septa and fat lobules.8
- Fascia, a deeper structure, is a dense, fibrous membrane.15
III. Scanning Technique, Normal Findings, and Common Variants
Equipment
- It is important to select an appropriate transducer when using bedside ultrasound for abscess evaluation. Because most subcutaneous abscesses are relatively superficial, a high-frequency (7‒12 MHz) linear array transducer is most useful.
- At times, a deeper abscess lies beyond the range of the linear transducer, so a lower-frequency transducer must be used. In this situation, a low-frequency linear-array transducer is preferred, but a curvilinear transducer can be used if none is available.
- Evaluation for peritonsillar abscess is a specialized application in which a high-frequency intracavitary probe is used.
- Color Doppler ultrasound can be useful in abscess evaluation, particularly in identifying large blood vessels adjacent to an abscess.
- Video 1. Color doppler demonstrating blood vessels around an abscess
- Color Doppler can also be helpful in the evaluation of groin masses because it can be used to differentiate an abscess from a pseudoaneurysm.4
- Video 2. Antecubital fossa pseudoaneurysm
- Power Doppler is a more advanced technique that detects low-velocity blood flow and movement. It can be useful for abscess evaluation because it allows visualization of hyperemia in the walls of abscesses and the surrounding tissues.5,16
Scanning Technique
- It is helpful to begin scanning a short distance away from the area of interest to gain an appreciation of the appearance of the normal, uninvolved anatomy.
- It may also be helpful to view the contralateral side of the patient’s body to obtain information about the normal appearance of structures.17
- Next, slide the probe over the extent of the abscess or cellulitis, maintaining the same orientation. Once the area has been visualized appropriately, rotate the transducer 90 degrees and repeat the process.
- If an abscess is present, place a gloved finger of the nondominant hand on the point of maximal fluctuance or “point” of the abscess. Then slide the transducer so that its mid-point is located against the finger. This can help you correlate the image on the screen with the anatomy and help plan the site of the incision.
- Body markings can also be used to indicate the extent of the abscess or the location of the incision.
- Once the presence of an abscess is confirmed, set the ultrasound probe aside and proceed with the incision and drainage. Another option is to incise the area while observing in real time under ultrasound. This technique may be helpful for deep or small collections, but it generally is not necessary.
- It may be helpful to repeat the ultrasound examination after incision and drainage to assess the success of the procedure and locate undrained collections of purulence.
Normal Findings
- With the equipment typically used for bedside ultrasonography, the epidermis and dermis cannot be differentiated. They appear together as a thin, hyperechoic layer.8
- The subcutaneous layer appears hypoechoic on ultrasound, with two components: hypoechoic fat interspersed with hyperechoic linear echoes running mostly parallel to the skin, which represent connective tissue septa.
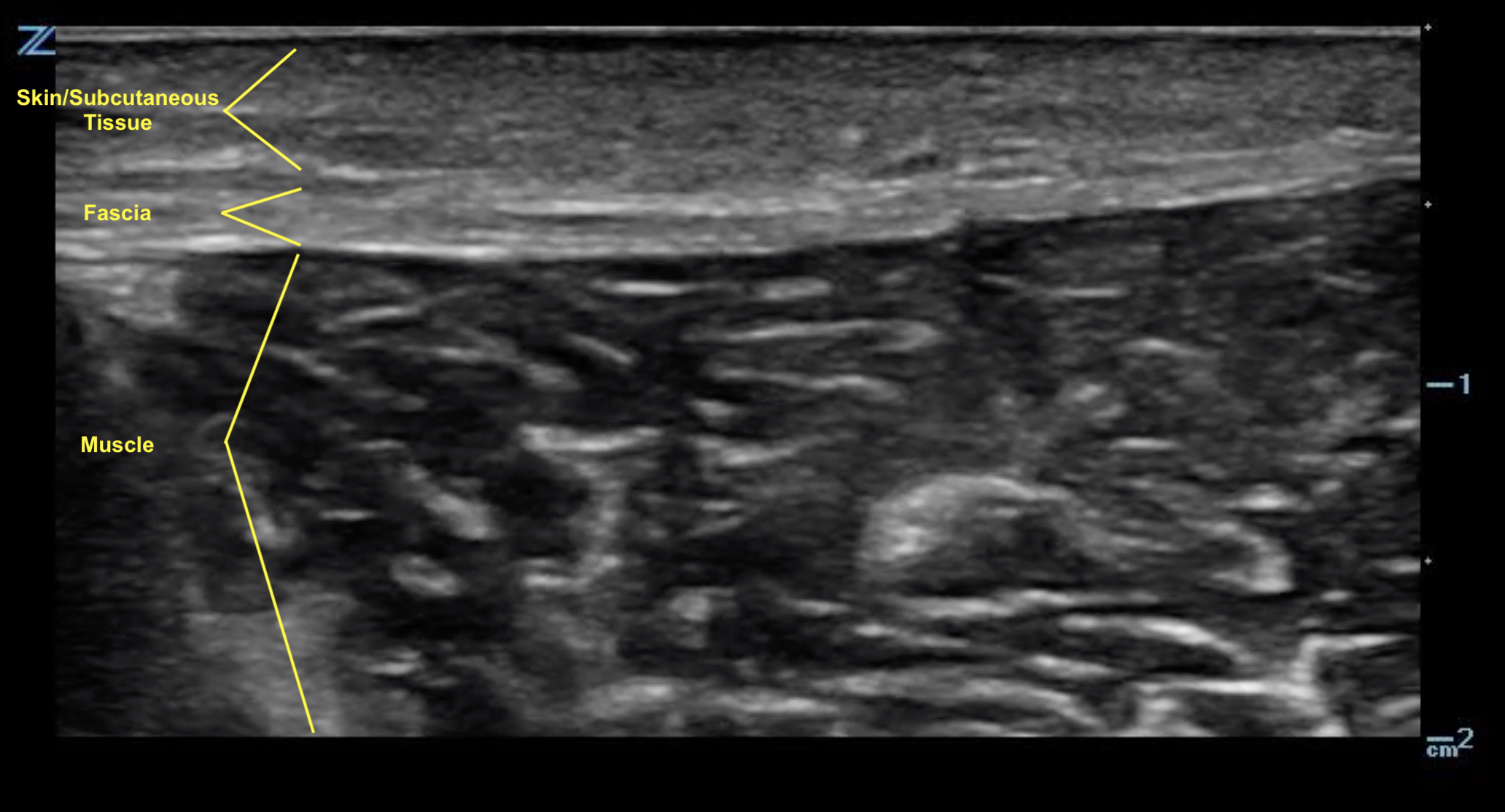
- Figure 1. Normal skin, subcutaneous tissue, and fascia.8
- Veins and nerves can be visualized within the subcutaneous layer.
- Fascia appears as a linear hyperechoic layer. Its thickness will vary depending on the location.
- Video 3. Normal skin, subcutaneous tissue, and fascia.
IV. Pathology
- On ultrasound, an abscess is a spherical or oblong structure that is largely anechoic or hypoechoic.

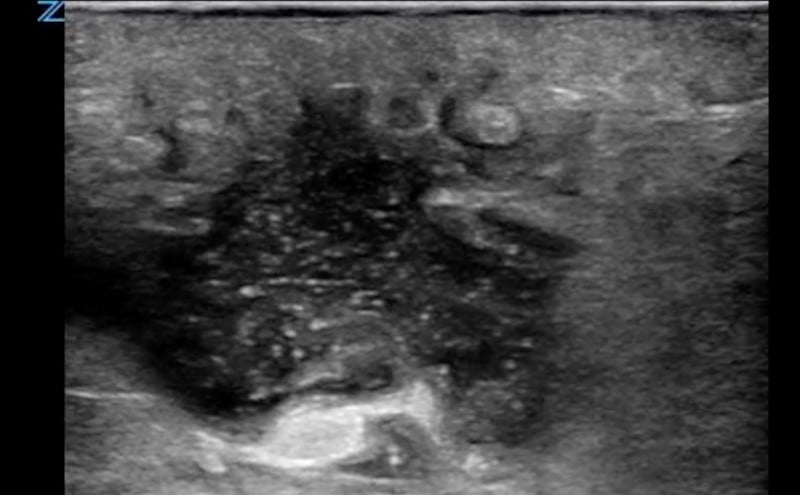
- Figure 2. Abscess containing hyperechoic debris
- However, as opposed to a simple cyst that will be uniformly anechoic throughout, an abscess will contain hyperechoic debris. This feature can be used to differentiate an abscess from a cyst.
- The walls of the abscess cavity might be distinct and hyperechoic, or they might have a ragged appearance and intermix with the adjacent tissue. Because of the anechoic nature of the abscess, posterior acoustic enhancement might be seen.
- Dynamic scanning, achieved with gentle compression of the probe, might cause the contents of the abscess to swirl, which can be diagnostic of an abscess.
- Video 4. Abscess with swish sign
- Video 5. Necrotizing fasciitis
- The ultrasound appearance of cellulitis will vary depending on its stage and severity. The initial appearance is typically generalized swelling and increased echogenicity of the skin and subcutaneous tissues.2,5
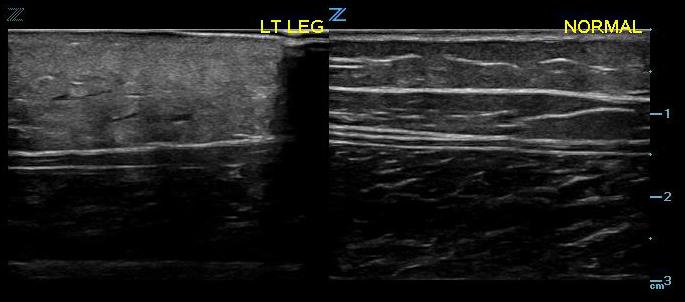
- Figure 3. Early cellulitis vs normal
- As cellulitis progresses and the amount of subcutaneous fluid increases, hyperechoic fat lobules become separated by hyperechoic fluid-filled areas. This later stage of cellulitis is most typical and has been described as having a cobblestone appearance.5
- Video 6. Cellulitis with cobblestoning
V. Pearls and Pitfalls
- Abscess and cellulitis are two common soft-tissue infections that can have similar appearances on physical examination.
- Bedside ultrasound can be very helpful in differentiating them.
- Ultrasound is effective at identifying occult abscesses in emergency department patients initially suspected of having cellulitis.
- On ultrasound imaging, an abscess appears as a spherical or oblong anechoic or hypoechoic collection containing hyperechoic debris.
The author thanks Linda J. Kesselring, MS, ELS, for her assistance in preparing the manuscript.
VI. References
- Ramirez-Schrempp D, Dorfman DH, Baker WE, Liteplo AS. Ultrasound soft tissue applications in the pediatric emergency department: to drain or not to drain? Pediatr Emerg Care. 2009;25(1):44-8.
- Chao HC, Lin SJ, Huang YC, Lin TY. Sonographic evaluation of cellulitis in children. J Ultrasound Med. 2000;19(11):743-9.
- Blaivas M. Ultrasound-guided breast abscess aspiration in a difficult case. Acad Emerg Med. 2001;8(4):398-401.
- Squire BT, Fox JC, Anderson C. ABSCESS: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12(7):601-6.
- Chau CL, Griffith JF. Musculoskeletal infections: ultrasound appearance. Clin Radiol. 2005;60(2):149-59.
- Tayal VS, Hasan N, Norton HJ, Tomaszewski CA. The effect of soft-tissue ultrasound on the management of cellulitis in the emergency department. Acad Emerg Med. 2006;13(4):384-8.
- Ozseker B, Ozcan UA, Rasa K, Cizmeli OM. Treatment of breast abscesses with ultrasound-guided aspiration and irrigation in the emergency setting. Emerg Radiol. 2008;15:105-8.
- Valle M, Zamorini MP. Skin and subcutaneous tissue. In: Bianchi S, Martiloni C, eds. Ultrasound of the Musculoskeletal System. Springer: Berlin; 2007: 19-43.
- Sivitz AB, Lam SH, Ramirez-Schrempp D, et al. Effect of bedside ultrasound on management of pediatric soft-tissue infection. J Emerg Med. 2010;39(5):637-43.
- Berger T, Garrido F, Green J, et al. Bedside ultrasound performed by novices for the detection of abscess in ED patients with soft tissue infections. Am J Emerg Med. 2012;30(8):1569-73.
- Adams CM, Neuman MI, Levy JA. Point-of-care ultrasonography for the diagnosis of pediatric soft tissue infection. J Pediatr. 2016;169:122-7.
- Gaspari RJ, Sanseverino A. Ultrasound-guided drainage for pediatric soft tissue abscesses decreases clinical failure rates compared to drainage without ultrasound. J Ultrasound Med 2018;37(1):131-6.
- Iverson K, Haritos D, Thomas R. The effect of bedside ultrasound on diagnosis and management of soft tissue infections in a pediatric ED. Am J Emerg Med. 2012;30(8):1347-51.
- Lin MJ, Neuman M, Rempell R, et al. Point-of-care ultrasound is associated with decreased length of stay in children presenting to the emergency department with soft tissue infection. J Emerg Med. 2018;54(1):96-101.
- O’Neill J. Introduction to musculoskeletal ultrasound. In: O’Neill J, ed. Musculoskeletal Ultrasound: Anatomy and Technique. Springer: New York; 2008:3-17.
- Robben SG. Ultrasonography of musculoskeletal infections in children. Eur Radiol. 2004;14:L65-77.
- Kaplan PA, Matamoros A Jr, Anderson JC. Sonography of the musculoskeletal system. Am J Roentgenol. 1990;155(2):237-45.



