Ocular Emergencies
Elaine Situ-LaCasse, MD and Srikar R. Adhikari, MD, MS, FACEP
Introduction and Indications
- Ocular emergencies account for 3% of all emergency department (ED) visits.1
- Point-of-care ocular ultrasound is helpful when there are no sophisticated tools, limited training, difficulty visualizing the ocular contents with traditional examination techniques, and/or lack of ophthalmology specialists for thorough evaluation of the eye.
- It provides a quick, accurate, well-tolerated, noninvasive tool for evaluating potentially vision-threatening conditions at the bedside.2,3
- Indications include eye trauma, eye pain, vision change or loss of vision, exophthalmos, foreign body, and headache.
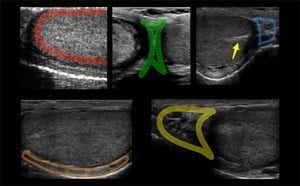
Anatomy
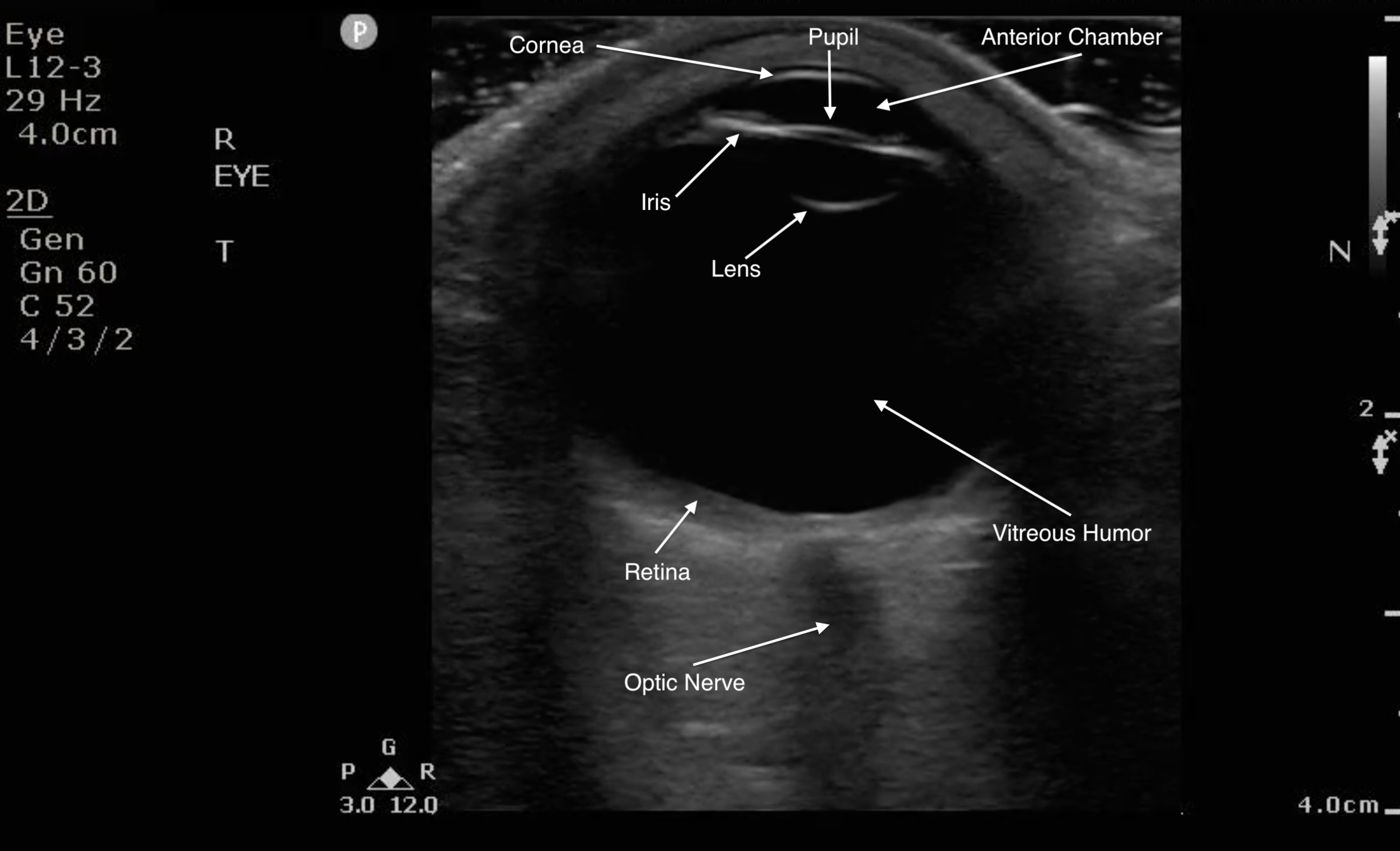
Figure 1. Sonographic eye anatomy
III. Scanning Technique, Normal Findings, and Common Variants
Scanning Technique
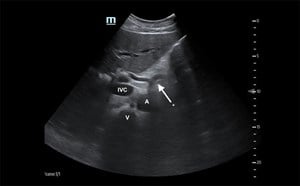
- The linear array transducer is the most appropriate for performing ocular ultrasound because of the higher frequency and resolution. Endocavitary probe can also be used in place of a linear array probe as it is high frequency as well.
- Lie the patient supine or partially upright position and ask them to close their eyes.
- Put copious amounts of gel on the patient’s closed eyelid(s).
- Gently place the transducer in transverse plane on top of the gel, making no direct contact with the eyelid and applying no pressure onto the eyelid.
- Steady your hand with your fifth digit on the patient’s nose or temple.
- The ocular structures are to be evaluated in the neutral position while the patient performs gentle eye movements from side to side and up and down.
- Video 1. Normal ocular ultrasound with the patient moving eye side to side
- Be sure to fan the transducer and move it from side to side to visualize the entire globe.
- Adjust the depth appropriately, so the area of interest is in the center of the image. Important to visualize the area posterior to the globe to identify the optic nerve sheath.
- In order to detect subtle findings in the vitreous, increase the gain to better visualize the region.
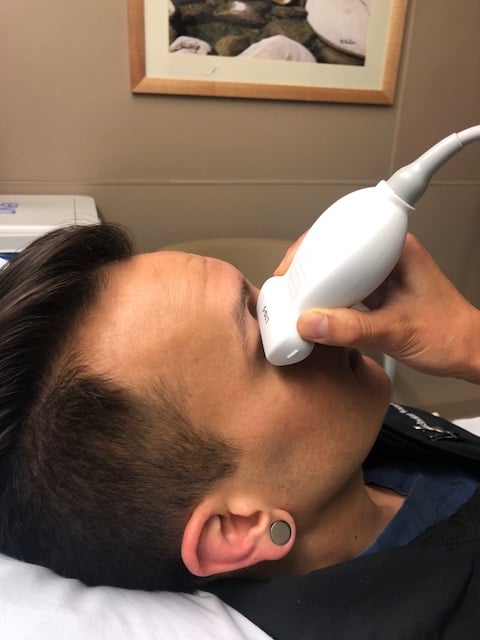
- Figure 2. A high-resolution linear array ultrasound transducer is being applied to the closed eyelid to perform an ocular examination.
Normal Findings
- Because the ocular chamber is fluid-filled, under ultrasound, it will appear as a round, anechoic structure.
- The most anterior structure seen, after the layer of ultrasound gel, is the eyelid.
- Just deep to the eyelid is the cornea and the anterior chamber. If too much pressure is applied during the ocular ultrasound examination, the anterior chamber may become compressed. It is important to avoid applying direct pressure to the eyelid.
- If the patient attempts to look down during the exam, you may be able to visualize the iris and pupil.
- The lens appears as a hyperechoic, curved line, located deep to the iris. If the patient has undergone cataract surgery, you may see two thin, hyperechoic parallel lines instead of the concave hyperechoic line.
- Normal vitreous humor will appear anechoic.
- The vitreous, retina, and choroid are located along the inside of the globe. Normally, you cannot differentiate one from the other.
- The most far field identifiable structure is the optic nerve. The parallel hyperechoic lines are the optic nerve sheath, since the optic nerve is hypoechoic and nondistinctive.
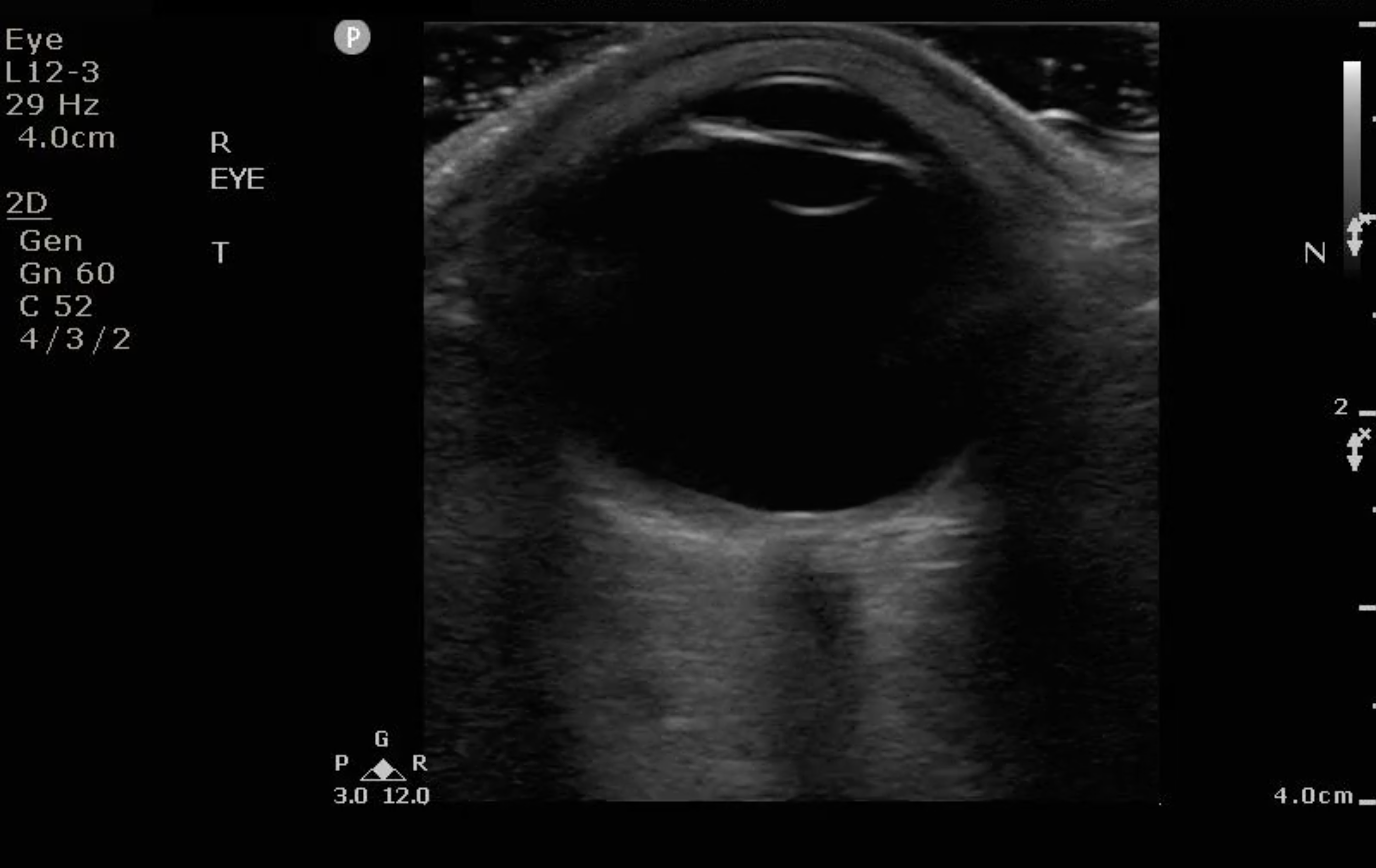
- Figure 3. Ultrasound image of a normal eye.
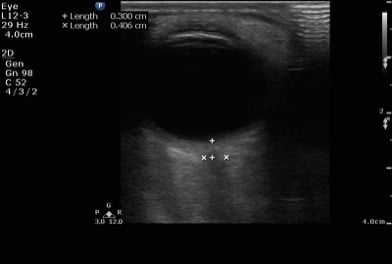
- Figure 4. Normal optic nerve sheath diameter measured 3mm from the insertion site of the optic nerve. Then it is measured transversely. Normal optic nerve sheath diameter in an adult is <5 mm.
Suggested Scanning Protocol for Identification of Pathology
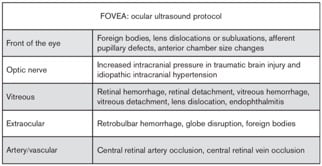
Figure 5. Suggested scanning protocol by Kilker et al 4
Common Variants
- Low reflective vitreous opacities (vitreous syneresis) are frequently seen in the normal aging eye when the ultrasound gain is increased.
- Age-related vitreous changes
- Collagen fibers extend throughout the vitreous and are attached around the optic nerve and are inserted in the peripheral retina near the ciliary body-optic nerve-visualized with high gain
- Retinoschisis
- Cataracts
Pathology
Globe Rupture
- Useful in evaluation of a traumatized eye, especially if patient’s eyelid is too edematous for direct visualization of the globe.
- Traumatic globe rupture is a major ophthalmologic emergency and almost always requires surgical intervention.
- Ultrasound findings include: decrease in globe size, anterior chamber collapse, and buckling of the sclera
- It is not recommended to routinely ultrasound a suspected globe rupture for concern of worsening the injury.
Video 2. Ultrasound of globe rupture with vitreous hemorrhage (Courtesy of Gavin Budhram, MD)
Ocular Foreign Body
- Intraocular foreign bodies are identified by their bright echogenic acoustic profile and either shadowing or reverberation artifacts seen in the usually echolucent vitreous.
- Ultrasound patterns of shadowing and comet tails may help differentiate foreign body materials.
- If there is concern that he foreign body has penetrated into the globe. Treat it as a globe rupture and contact ophthalmology immediately.
- In a porcine model, ocular ultrasound for detection of metal foreign bodies5:
- Sensitivity of 87.5%
- Specificity of 85.2%
- Negative predictive value: 85.2%
-
Video 3. Hyperechoic focus noted over the surface of the patient’s left anterior chamber, suggestive of foreign body, especially in the appropriate clinical setting.
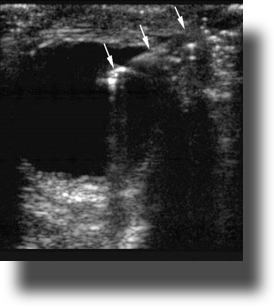
- Figure 6. Intraocular foreign body (Courtesy of Matthew Lyons, MD)
Lens Dislocation
- Typically caused by blunt trauma to the eye or may occur spontaneously in patients with Marfan’s syndrome.
- Ocular ultrasound is particularly useful when there is so much palpebral edema or hematoma that direct visualization is difficult.
- Lens can be partially dislocated or completed dislocated.
- If completed dislocated, the lens can be found in the anterior chamber, floating in the vitreous, or laying in the most dependent part of the globe.4
- Lens subluxation (partial dislocation) can be subtle, since it may only be slightly out of place. It may become more obvious with eye movement.

- Figure 7. The lens is noted in the posterior globe, in the shape of a coffee bean.
Vitreous Hemorrhage
- Vitreous hemorrhage can interfere with vision and can cause blindness if large.
- Appears as echogenic material in the posterior chamber.
- Sonographic appearance of vitreous hemorrhage depends on its age and severity.
- Fresh and/or mild hemorrhages: small dots with low reflectivity and swirl in the vitreous with eye movement.
- Older and/or severe hemorrhages: blood will organize and form membranes.
- May layer inferiorly due to gravity.
- Video 4. The hyperechoic blood is swirling in the vitreous compartment of the globe. This is called the “washing machine sign.”
Posterior Vitreous Detachment (PVD)
- It is a common cause for vision loss and decreased vision.
- Risk of development increases with age and can occur in 11-46% of patients 60-90 years old.6
- PVD will appear as thin, hyperechoic, mobile membranes in the posterior chamber that will NOT be tethered to the optic disk.
- Visualization can sometimes be very challenging without the gain maximized.
- Unlike retinal detachment, PVD can cross the midline of the globe.
Video 5. The thin hyperechoic line crossing over the midline is the vitreous detachment. Small amount of vitreous hemorrhage is seen posterior to the detachment.
Retinal Detachment (RD)
- RDs may be difficult to diagnose on physical examination, especially if the RD is small.
- Ocular ultrasound to diagnose RD has sensitivities of 0.97 to 1.00 and specificities of 0.83 to 1.00.7
- Attachment sites of the retina are: ora serrata in the anterior globe and the optic nerve posteriorly.
- Occasionally, retinal tears are accompanied by vitreous hemorrhages, retinal hemorrhages, and/or PVDs.
- Retinal hemorrhages will be located below the retina.
- A retinal detachment will be seen as a hyperechoic undulating membrane in the posterior globe, extending to the lateral globe.
- Complete RDs may appear as a V shape and will be tethered to the optic nerve.
- RD is usually seen as a thicker, more linear membrane then the undulating, thinner membrane of PVD.
- The macula is temporal to the optic nerve. It cannot be visualized sonographically though location can be approximated by the location of lens (see Fig. 8). If the RD extends temporally from the base of the optic nerve, it can be assumed that it has come off of the macula (“mac off retinal detachment”).
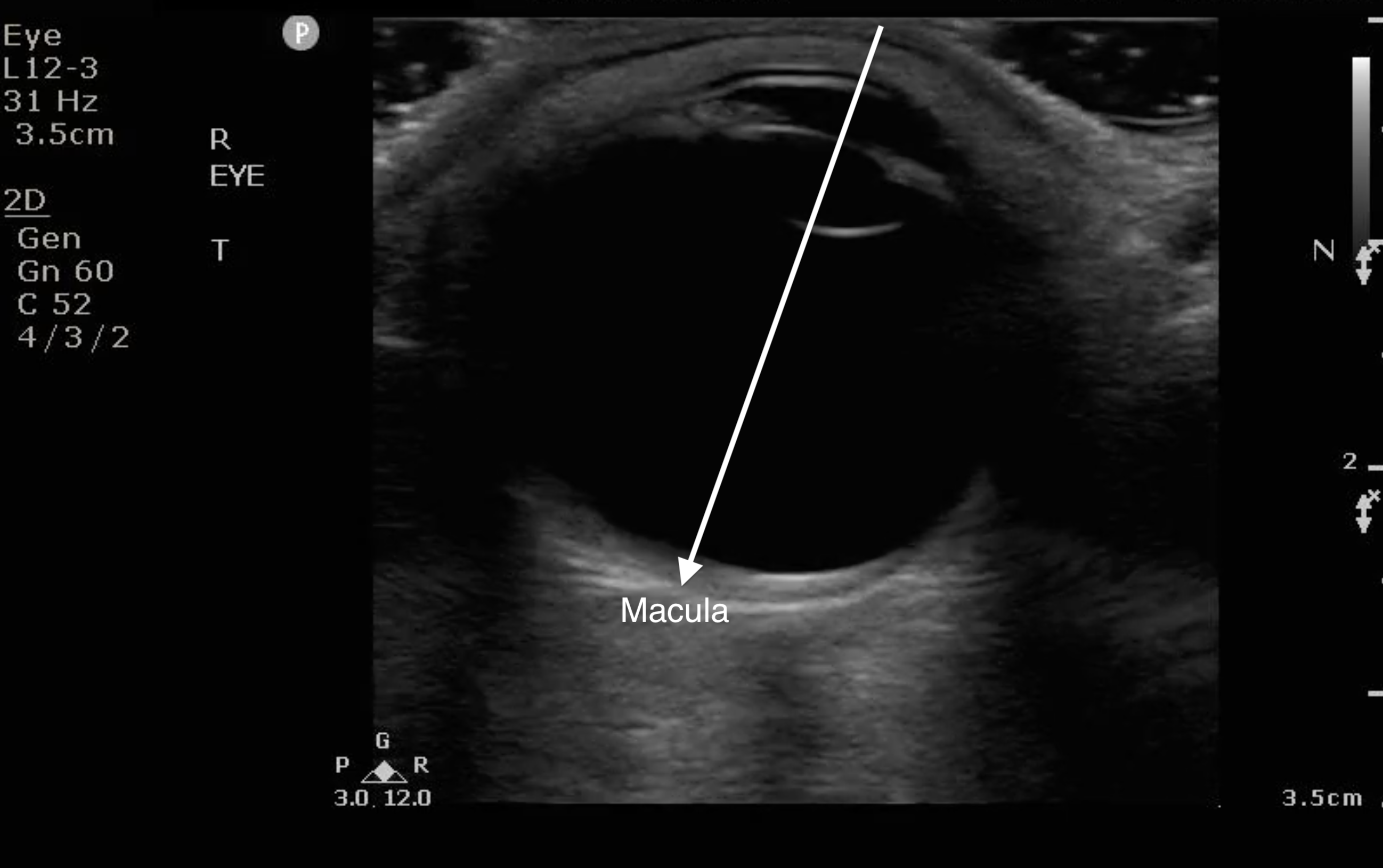
- Figure 8. When the anterior chamber is lined up with the lens, draw a line to bisect the globe to the back on the temporal side. That is where the macula is located.
- RD with the retina still over the macula is an ocular emergency warranting an emergent consultation to ophthalmology in order to take measures to prevent the retina from coming off of the macula.
- RD with the retina off the macula requires an urgent follow-up with ophthalmology.
Video 6. The two thick hyperechoic lines are the detached retinal membrane. It is retinal detachment because it is tethered at the optic nerve insertion site.
Choroid Detachment (CD)
- The choroid is the highly vascularized layer of the globe that is between the retina and the sclera.
- Three main categories of CD: serous, hemorrhagic, or mixed. Serous CDs are associated with low intraocular pressures, and patient may have some discomfort in the eye. Hemorrhagic CDs are painful and associated with high intraocular pressures.8
- Risk factors for serous CDs: inflammation, trauma, cancer, farsightedness, and certain medications.8
- Risk factors for hemorrhagic CDs: surgery, older age, atherosclerosis, and blood thinners.8
- Thick white membranes that form a central hour-glass shape. CDs spare the optic disk posteriorly but may detach anteriorly up to the ciliary bodies.
Video 7. Choroid detachment seen in this video. The two sides come together to form an hourglass shape in the center, as opposed to retinal detachment, which typically forms a V shape.
Periorbital Cellulitis
- Periorbital cellulitis is the infection that is anterior to the septum of the eye.
- Primary causes are trauma or nearby infection such as sinusitis.
- Needs to be differentiated from orbital cellulitis.
- On ocular ultrasound, you will see the thickening of the palpebral tissue.
- If severe, you may also see signs of abscess.
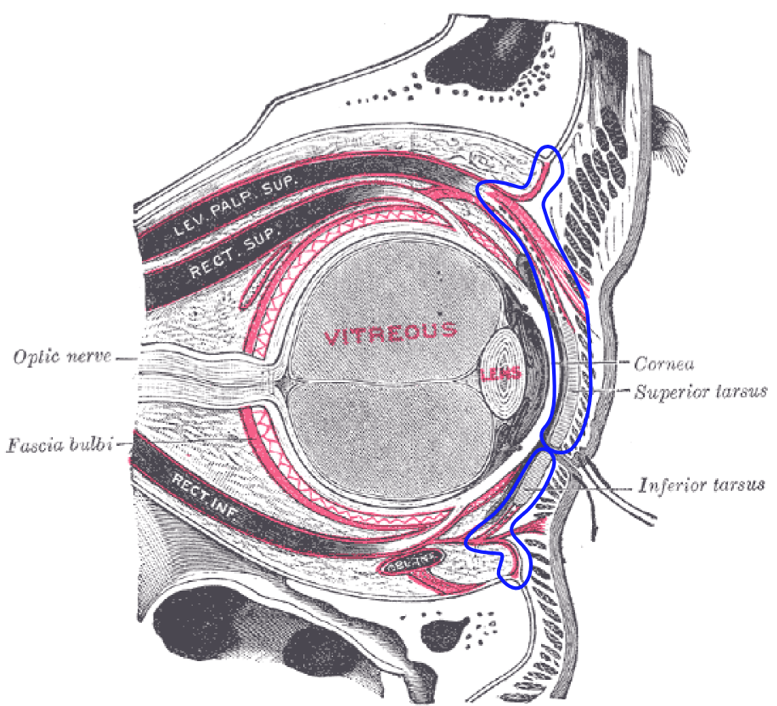
- Figure 9. The blue line denotes the ocular septum (courtesy of Mikael Häggström, 20149)
Video 8. You can see that the eyelid, which is directly overlying the anterior chamber, is thickened, concerning for preseptal cellulitis.
Video 9. There is an abscess on the nasal side of the right eye in the video above, a known complication of preseptal cellulitis.
Orbital Cellulitis
- Patients typically present with atraumatic eye swelling, redness, and pain with extraocular movements.
- They may have been initially diagnosed with preseptal cellulitis and returning for worsening symptoms.
- Up to 41% of patients with orbital cellulitis also have evidence of sinusitis.10,11
- Concomitant diagnoses of patients who go to surgery for orbital cellulitis: Exophthalmos, acute osteomyelitis, acute sinusitis, conjunctival edema, diplopia, chronic sinusitis, and facial cellulitis.12
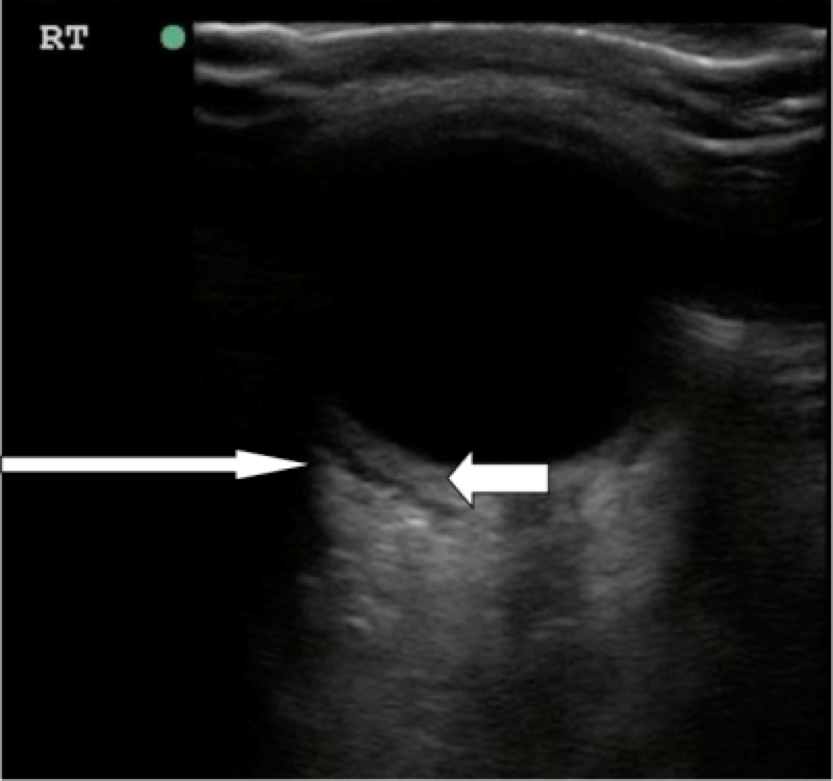
- Figure 10. Orbital cellulitis. Long arrow shows hypoechoic rim concerning for postseptal fluid tracking posterior to the globe. Short arrow shows thickening of the posterior segment of the eye.12 (Source: Seif D et al.13)
Video 10. Orbital cellulitis (Courtesy of Dr. J. Chris Fox)
Asteroid Hyalosis (AH)
- Benign degenerative condition that leads to the accumulation of vitreous calcium phospholipids.14
- This can be mistaken for vitreous hemorrhage.
- Patients may complain of floaters in their vision.
- On ultrasound, AH will appear as hyperechoic specks suspended in the vitreous, giving it a snow globe appearance.14
- The sparkling appearance of AH differs from the layering of the less echogenic blood in VH that tend to settle posteriorly.14
Video 11. Asteroid hyalosis has the appearance of a snow globe or starry sky in the vitreous.
Optic Nerve Head Drusen (ONHD)
- ONHD are hyaline bodies that result from calcification of mitochondria of optic nerve axons.15
- This calcification will be seen protruding from the optic nerve head.
- Can be confused for papilledema, so ONHD is called “pseudopapilledema.”
- This is typically a benign finding and does not affect vision, some patients may complain of peripheral vision loss.16
- Under ultrasound, you can see a hyperechoic outpouching from the optic nerve disk that is immobile with ocular movements.
Video 12. The drusen (hyperechoic focus) is seen protruding from the optic nerve head.
Elevated Intracranial Pressure – Optic Nerve Sheath Measurement
- Measuring the optic nerve sheath diameter (ONSD) is helpful in determination of elevated intracranial pressure (ICP), especially those who present to the ED with head injury and those with spontaneous intracranial bleed.
- Increased ONSD as a proxy for elevated ICP has also been associated with poor neurologic outcomes in cardiac arrest patients.17
- Ocular ultrasound is a rapid, non-invasive means of detecting elevated ICP particularly for patients who have altered mental status, unconscious, or intubated and sedated.
- The optic nerve attaches to the globe posteriorly and is wrapped in a sheath that contains cerebrospinal fluid. The optic nerve sheath is contiguous with the dura mater and has a trabeculated arachnoid space through which CSF slowly percolates.
- Evaluation of the optic nerve sheath diameter can detect elevated ICP.
- On ultrasound, a normal optic nerve sheath measures up to 5.0 mm in diameter. The ONSD is measured 3mm posterior to the globe for both eyes.
- A position of 3mm behind the globe is recommended because the ultrasound contrast is greatest, and the results are more reproducible.
- Two measurements are averaged.
- An averaged ONSD > 5 mm in adults is considered abnormal and elevated ICP should be considered.4
- An averaged ONSD > 4.5 mm in children (1-15 years) and > 4mm (less than 1 year of age) are abnormal.4
- Ohle et al published a systematic review and meta-analysis of 478 patients showing sonographic evaluation of the optic nerve sheath corresponding well with signs of elevated ICP on CT head, with sensitivity of 95.6% and specificity of 92.3%.18

- Figure 11. Example of increased optic nerve sheath diameter. Optic nerve sheath diameter > 5mm is considered abnormal and should raise concern for elevated intracranial pressure.
Retrobulbar Hematoma (RH) or Orbital Emphysema
- RH can be secondary to traumatic or nontraumatic causes.
- It will appear as a hypoechoic area posterior to the globe and may distort the posterior globe.
- Orbital emphysema is air tracking along the posterior surface of the globe, and it will cause “dirty shadowing,” which is shadowing that is bright white and obscures the structures in the far field.
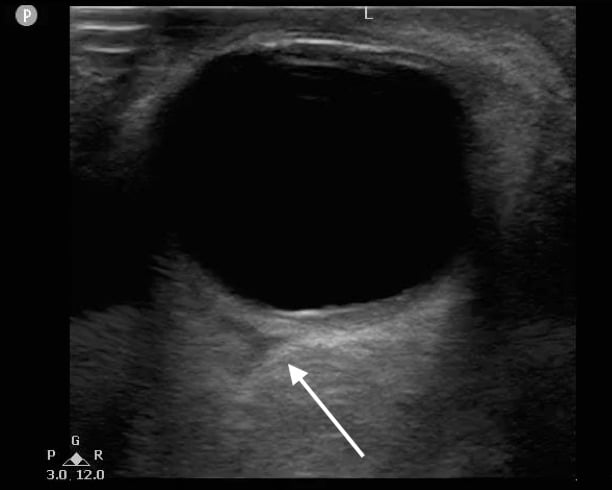
- Figure 12. Triangular hypoechoic area (white arrow) suggestive of retrobulbar hematoma also known as “Guitar Pick Sign.”
Central Retinal Artery Occlusion (CRAO)
- Patients will typically present with painless loss of vision.
- If a hyperechoic focus is seen posterior to the globe within the optic nerve sheath, there is concern for CRAO secondary to a calcified embolus. This is called the “spot sign.”
- Nedelmann et al stated that the retrobulbar spot sign may predict the ineffectiveness of thrombolytic treatment in patients with CRAO with the spot sign, as opposed to absence of the spot sign which may point to a thrombus causing CRAO that would more likely be amenable to thrombolysis.19
- Color Doppler imaging and pulse wave Doppler can also be used to search for flow into the central retinal artery. Be cautious and not keep the gate on the posterior globe for prolonged periods of time, since there is higher energy and heat transferred to this sensitive region.
Video 13. You can see a hyperechoic focus, or “spot sign,” in the retrobulbar space, concerning for a calcified embolus causing CRAO (Courtesy of Austin Gross, MD).
V. Pearls and pitfalls
- Copious amounts of gel should be applied to the closed eyelid so that the transducer does not actually have to make contact with the eyelid, especially if there is any trauma to the eye making globe rupture a possibility. Any pressure on the traumatic eye could be detrimental and ultrasound should not be performed if globe rupture likely.
- As with fetal ultrasound, it is important to limit the duration of the examination as much as possible, especially when using spectral and color Doppler, which are thought to produce increased levels of mechanical energy.
- Various artifacts may interfere with the examination, especially air artifacts around the eyelids.
- PVD and RD can occur together. PVD can cause RD.
- Chronic PVD may become stiffer and denser, causing it to resemble RD.
- Membranes from vitreous hemorrhage can mimic RD.
- Inappropriately low gain can cause you to miss posterior segment pathology.
- If your machine’s “ocular” preset is not allowing you to see the ocular structures well enough, consider turning up the gain.
- When in doubt, ultrasound the unaffected eye to see what may be “normal.”
VI. References
- Rosen P (ed). Emergency Medicine Concepts and Clinical Practice, ed 4. St. Louis: Mosby, 1997, pp 2243-5.
- Blaivas M, Theodoro D, Sierzenski P. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10(4):376-81.
- Blaivas M, Theodoro D, Sierzenski P. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9:791-9.
- Kilker BA, Holst JM, Hoffmann B. Bedside ocular ultrasound in the emergency department. Eur J Emerg Med. 2014;21(4):246-53.
- Garcia JPS, Garcia PMT, Finger PT. Dynamic ultrasound movements of the eye and orbit [video report]. Br J Ophthalmol. 2006.
- Weber-Krause B, Eckardt C. Incidence of posterior vitreous detachment in the elderly. Ophthalmologe. 1997;94(9):619-23.
- Vrablik ME, Snead GR, Minnigan HJ, et al. The diagnostic accuracy of bedside ocular ultrasonography for the diagnosis of retinal detachment: A systematic review and meta-analysis. Ann Emerg Med. 2015;65(2):199-203.e1.
- American Society of Retina Specialists. Fact Sheet: Choroid Detachment. 2016.
- Häggström, Mikael (2014). "Medical gallery of Mikael Häggström 2014." WikiJournal of Medicine 1(2):8. doi:10.15347/wjm/2014.008. ISSN 2002-4436.
- Bae Ca, Bourget D. “Periorbital Cellulitis.” StatPearls. StatPearls Publishing LLC. 2017.
- Garrity J, MacMillan B. “Preseptal and Orbital Cellulitis.” Merck Manual. Oct. 2017.
- Marchiano E, Raikundalia MD, Carniol ET, et al. Characteristics of patients treated for orbital cellulitis: An analysis of inpatient data. Laryngoscope. 2016;126(3):554-9.
- Seif D, Mailhot T, Chilstrom M, et al. Case Report: To see or not to see…ACEP Emergency Ultrasound Section Newsletter, June 2013.
- Lema PC, Mantuani D, Nagdev A, et al. Asteriod hyalosis masquerading as vitreous hemorrhage on point-of-care sonography. J Ultrasound Med. 2018;37(1):281-4.
- Auw-Haedrich C, Staubach F, Witschel H. Optic disc drusen. Surv Ophthalmol. 2002;47(6):515-32.
- Porter D. “What Are Drusen?” American Academy of Ophthalmology. Apr 2018.
- You Y, Park J, Min J, et al. Relationship between time related serum albumin concentration, optic nerve sheath diameter, cerebrospinal fluid pressure, and neurological prognosis in cardiac arrest survivors. Resuscitation. 2018;131:42-7.
- Ohle R, McIsaac SM, Woo MY, et al. Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography. 2015;34(7):1285-94.
- Nedelmann M, Graef M, Weinand F, et al. Retrobulbar spot sign predicts thrombolytic treatment effects and etiology in central retinal artery occlusion. Stroke. 2015;46(8):2322-4.