MSK - Pediatric Hip
Samuel H. F. Lam, MD, MPH, FACEP
I. Introduction and Indications
- Hip pain/limping are common complaints in children presenting to the ED.
- Differential diagnosis includes septic arthritis, transient synovitis (toxic synovitis), osteomyelitis, neoplasm, Legg-Calve-Perthes disease, avascular necrosis of femoral head, fracture, muscle strain, and juvenile rheumatoid arthritis among others.
- Along with X-ray and blood tests, ultrasound is a valuable tool to narrow down differential diagnosis.1,2
- Presence of a hip effusion may raise suspicion for septic arthritis, osteomyelitis, and other time sensitive diagnoses; while absence of effusion may decrease need for further testing
- Ultrasound can detect effusion as small as 1mL, with sensitivity of 90-100%.3,4
- In a prospective study of 28 patients (55 hips), Vieira and Levy found that emergency physician performed point-of-care ultrasound (POCUS) was 80% sensitive and 98% specific in detecting hip effusions compared to the gold standard of radiology department ultrasound.5
- A retrospective study by the same group on 516 patients (926 hips) reported POCUS sensitivity of 85% and specificity of 98%, with overall accuracy of 93%.6
- Additional case series have also been published of emergency physicians using POCUS to facilitate evaluation of pediatric hip pain.7-10
II. Anatomy
- Hip joint is where the head of femur articulates with the acetabulum of the pelvis
- Surrounded by strong fibrous capsule
- Iliopsoas muscle lies anterior/superficial to the joint capsule
Scanning Technique, Normal Findings and Common Variants
- Typically a high frequency (5-10MHz), linear transducer is used due to superficial location of structures. Lower frequency, curvilinear transducer may be necessary in patients with thicker soft tissue layers.
- Lie patient supine. Hips in slight external rotation and flexion (“frog-leg” position), if possible.
- Place transducer on anterior hip, along the long axis of the femoral neck, slightly below and perpendicular to inguinal ligament and lateral to the femoral vessels.
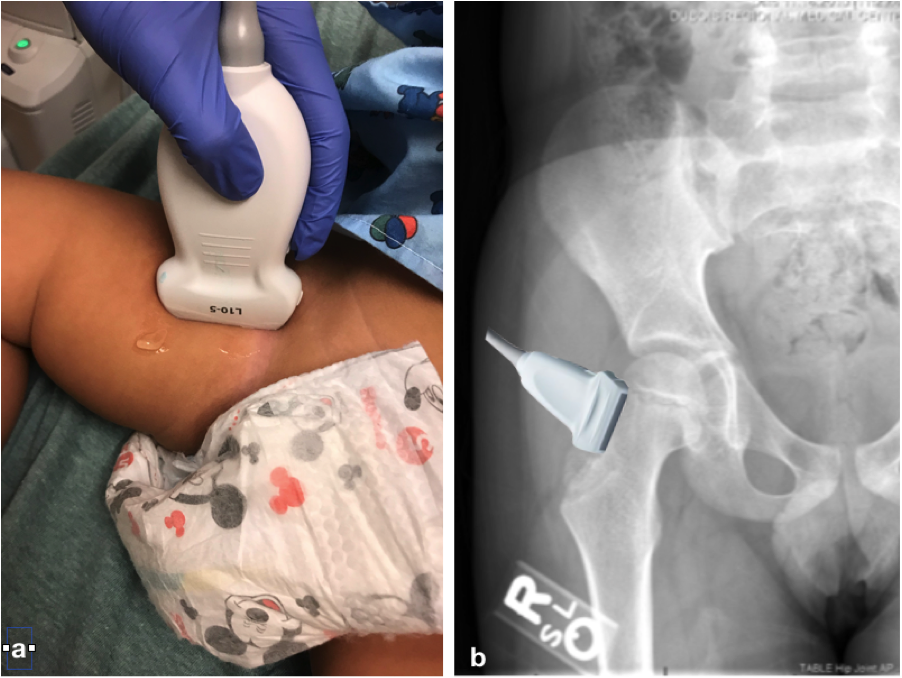
- Figure 1. Placement of ultrasound transducer (a) and X-ray of the hip (b)
- Indicator towards the patient’s head
- Locate the femur with its characteristic hyperechoic periosteum and posterior acoustic shadowing.
- Use femoral head and the slanting neck as landmark. Identify the hyperechoic fibrous joint capsule.
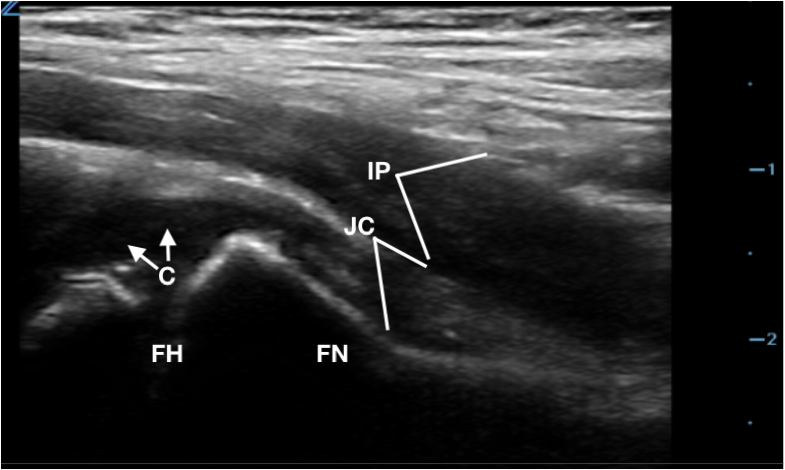
- Figure 2. Anatomy of hip joint on ultrasound (C: Cartilage/physis on femoral head, FH: Femoral Head, FN: Femoral Neck, JC: Joint Capsule, IP: Iliopsoas muscle)
- Measure thickness of joint (area from periosteum to outer joint capsule just deep to iliopsoas muscle) at the femoral neck.
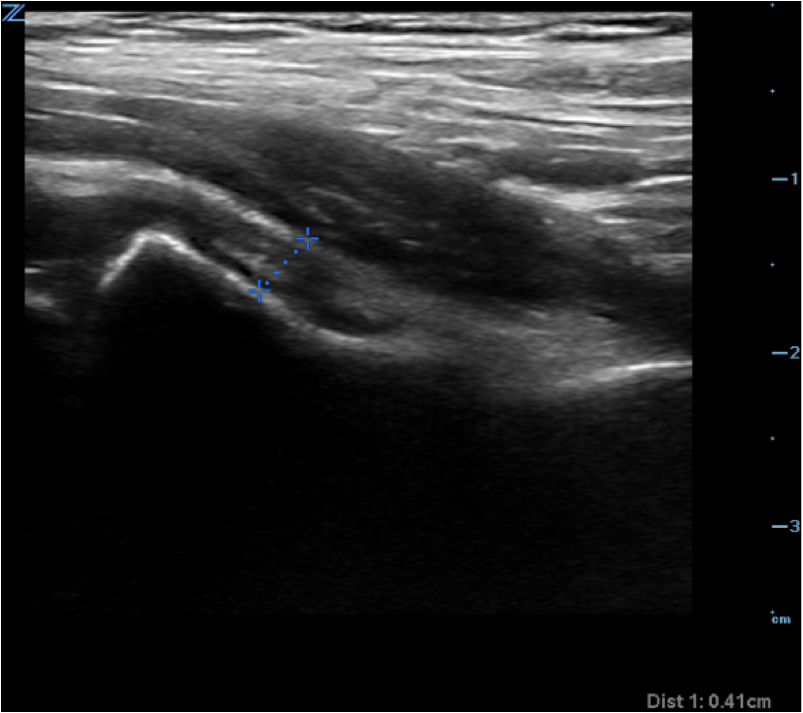
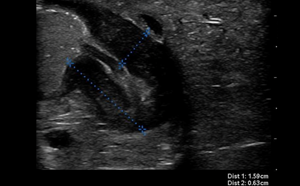
- Figure 3. Measurement of hip joint fluid thickness
IV. Pathology
- A capsular-synovial thickness >5 mm, or >2 mm difference compared to the asymptomatic contralateral side indicates hip joint effusion in children
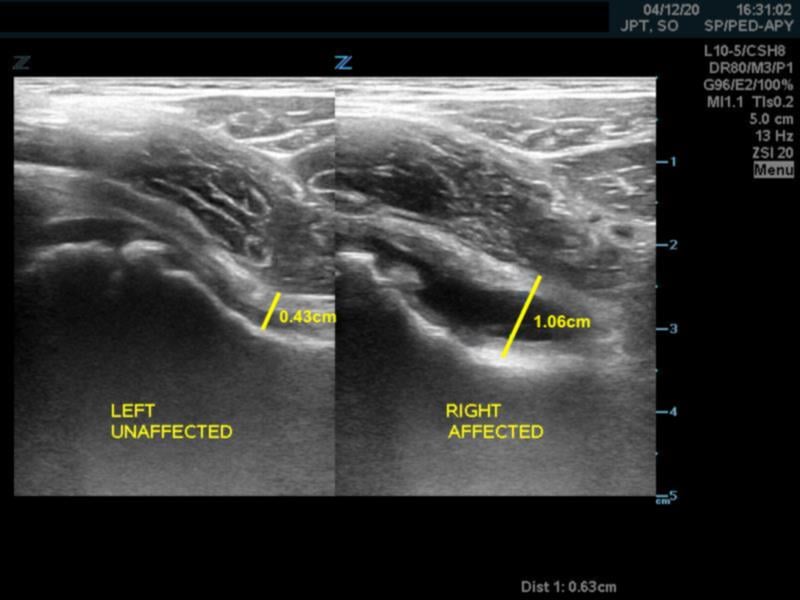
- Figure 4. Capsular-synovial thickness measurement >5mm in hip effusion (right)
- Joint capsule also appears convex instead of concave in case of effusion
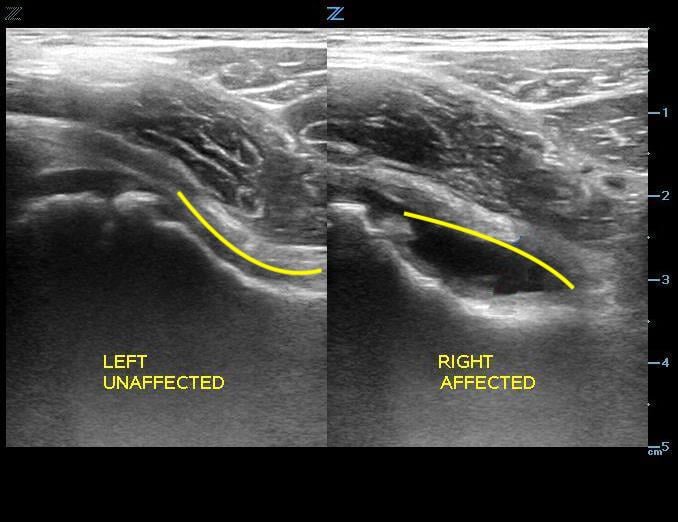
- Figure 5. Hip without effusion (left) has a concave shaped joint capsule and hip with joint effusion (right) has a convex shaped joint capsule.
- POCUS can also be used to guide diagnostic arthrocentesis
- Septic arthritis may progress to destruction of cartilage and bone if untreated, leading to permanent disability
- Treatment is intravenous antibiotics +/- open joint irrigation
- However, 46-86% of patients with transient synovitis of the hip also have effusion present.11
V. Pearls and Pitfalls
- Pearls
- Effusion can sometimes be heterogeneous or even hyperechoic, especially with purulent material.
- Presence of hip effusion cannot distinguish between a benign condition (eg, transient synovitis) and a more serious condition (eg, septic joint, osteomyelitis). Hence clinical context and other diagnostic tests would be necessary to distinguish one from another.
- Pitfalls
- Too much pressure from the transducer may compress effusion leading to false negative result.
- Cartilage over femoral head may be mistaken as effusion as it is hypoechoic. True effusion crosses the femoral head and extends along the femoral neck while cartilage does not.
Figure 6. Normal femoral head with hypoechoic cartilage
VI. References
- Dorr U, Zerger M, Hauke H. Ultrasonography of the painful hip. Prospective studies in 204 patients. Pediatr Radiol. 1988;19(1):36-40.
- Nimityongskul P, McBryde AM Jr, Anderson LD, et al. Ultrasonography in the management of painful hips in children. Am J Orthop. 1996;25(6):411-4.
- Siegel MJ, ed. Pediatric Sonography 4th Ed. Philadelphia: Lippincott Williams & Wilkins, 2011.
- Miralles M, Gonzalez G, Pulpeiro JR, et al. Sonography of the painful hip in children: 500 consecutive cases. Am J Roentgenol. 1989;152(3):579-82.
- Vieira RL, Levy JA. Bedside ultrasonography to identify hips effusions in pediatric patients. Ann Emerg Med 2010;55(3):284-9.
- Cruz CI, Vieira RL, Mannix RC, et al. Point-of-care hip ultrasound in a pediatric emergency department. Am J Emerg Med 2018; 36(7):1174-77.
- Garrison J, Nguyen M, Marin JR. Emergency department point-of-care ultrasound hip ultrasound and its role in the diagnosis of septic hip arthritis: a case report. Pediatr Emerg Care. 2016;32(8):555-7.
- Deanehan J, Gallaher R, Vieira R, et al. Beside hip ultrasonography in the pediatric emergency department: a tool to guide management in patients presenting with limp. Pediatr Emerg Care. 2014;30(4):285-7.
- Tsung JW, Blaivas M. Emergency department diagnosis of pediatric hip effusion and guided arthrocentesis using point-of-care ultrasound. J Emerg Med. 2008;35(4):393-9.
- Shavit I, Eidelman M, Galbraith R. Sonography of the hip-joint by the emergency physician: its role in the evaluation of children presenting with acute limp. Pediatr Emerg Care. 2006;22(8):570-3.
- Plumb J, Mallin M, Bolte RG. The role of ultrasound in the emergency department evaluation of the acutely painful pediatric hip. Ped Emerg Care. 2015;31(1):54-8.