October 28, 2021
GI - Intussusception
Kahra Nix, MD
Joshua Guttman, MD, FACEP
I. Introduction and Indications
- Ultrasound is the first-line imaging modality for detecting intussusception in pediatric patients. It is safe and does not expose children to radiation as the abdominal x-ray and barium enema do. Ultrasound also has a higher sensitivity and specificity for detecting intussusception than a non-contrasted x-ray. Emergency clinicians are appropriately and effectively using point-of-care ultrasound to more rapidly detect intussusception, which is useful in directing utilization of healthcare resources and expediting definitive care.
- Importance of the ultrasound exam
- Early symptoms of intussusception are difficult to distinguish from more benign conditions. Less than 40% of pediatric patients have the classic triad that includes colicky abdominal pain, bloody (“currant jelly”) stool and emesis.1
- Missed diagnosis of intussusception occurs frequently; some centers have found a rate as high as 48%.2 Symptoms can be as non-specific as crying or lethargy.
- The consequence of missed diagnosis is increased morbidity and mortality due to ischemic bowel, necrosis and perforation.
- Enema reduction of intussusception is often less successful in the delayed diagnosis due to worsened bowel wall edema.
- After appendicitis, intussusception is the next most common cause of an acute abdominal emergency in pediatric patients.3
- Per the above concerns, point-of-care abdominal ultrasound should be considered in the appropriate patient to expedite care and therefore prevent delayed diagnosis leading to complications and worse outcomes.
- Accuracy/sensitivity of ultrasound for this exam
- US performed by radiology for ileocolic intussusception has a sensitivity of 97.9% and specificity of 97.8%. When performed by an experienced sonographer, US is an excellent primary imaging modality as it has a negative predictive value of 99.7%.4
- Point-of-care ultrasound performed by pediatric emergency medicine providers looking for intussusception—after only one hour of training—has a sensitivity of 85% and specificity of 97%. The negative predictive value was 97%.5
- Indications and clinical scenarios for which this exam should be used
- Consider abdominal US in pediatric patients with a clinical concern for intussusception. These include children between 3 months and 6 years with persistent vomiting in the absence of diarrhea, as well as patients who have bloody stool, colicky abdominal pain, episodes of crying or lethargy.
- Intussusception rarely occurs in children younger than 3 months and is most commonly diagnosed in children 6 months to 2 years.6,7
II. Anatomy
- Relevant anatomy
- Most commonly, intussusception occurs in pediatric patients as the terminal ileum is pushed into the cecum by peristalsis at the ileocecal junction due to a lead point.
- The cecum is found in the right lower quadrant in between the abdominal wall musculature and the psoas muscle.
- Surface anatomy used to help guide best scanning approaches
- Start in RLQ and make an upside-down U shape along the periphery of the abdomen. Finish in the LLQ after following the path of the colon. (Fig. 1)
- Intussusception is most commonly found in the RUQ at the hepatic flexure.
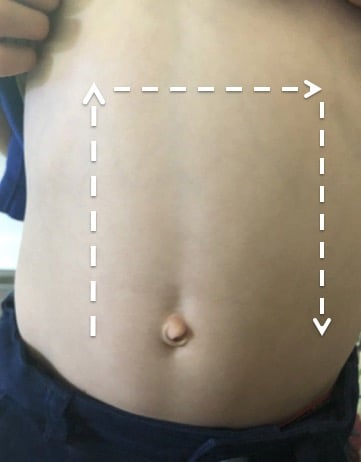
- Figure 1. Surface anatomy image detailing abdominal point-of-care ultrasound for intussusception
- If pathology is not found by sweeping the periphery of the abdomen (Fig. 1), and suspicion is high, consider the lawn mower technique. This is done by starting in the RLQ as show in the figure below and sweeping through the entire surface of the abdomen. (Fig. 2)
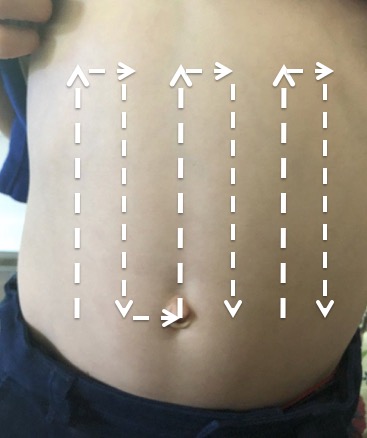
- Figure 2. Surface anatomy image describing the lawn mower technique to evaluate for intussusception
III. Scanning Technique and Normal Findings
- Scanning technique
- Transducer selection: The linear transducer is preferentially used as it provides the highest resolution and can visualize the bowel in almost all children presenting with concern for intussusception. The curvilinear transducer may be used if the patient’s body habitus does not allow for adequate bowel visualization with the linear transducer.
- Scanning approach step-by-step. (Fig. 1)
- The child should be placed in the supine position. Consider keeping the child in the parent’s lap. This will assist with keeping the patient calm. The parents can also restrain arms and legs as needed.
- The probe indicator should point to the patient’s right.
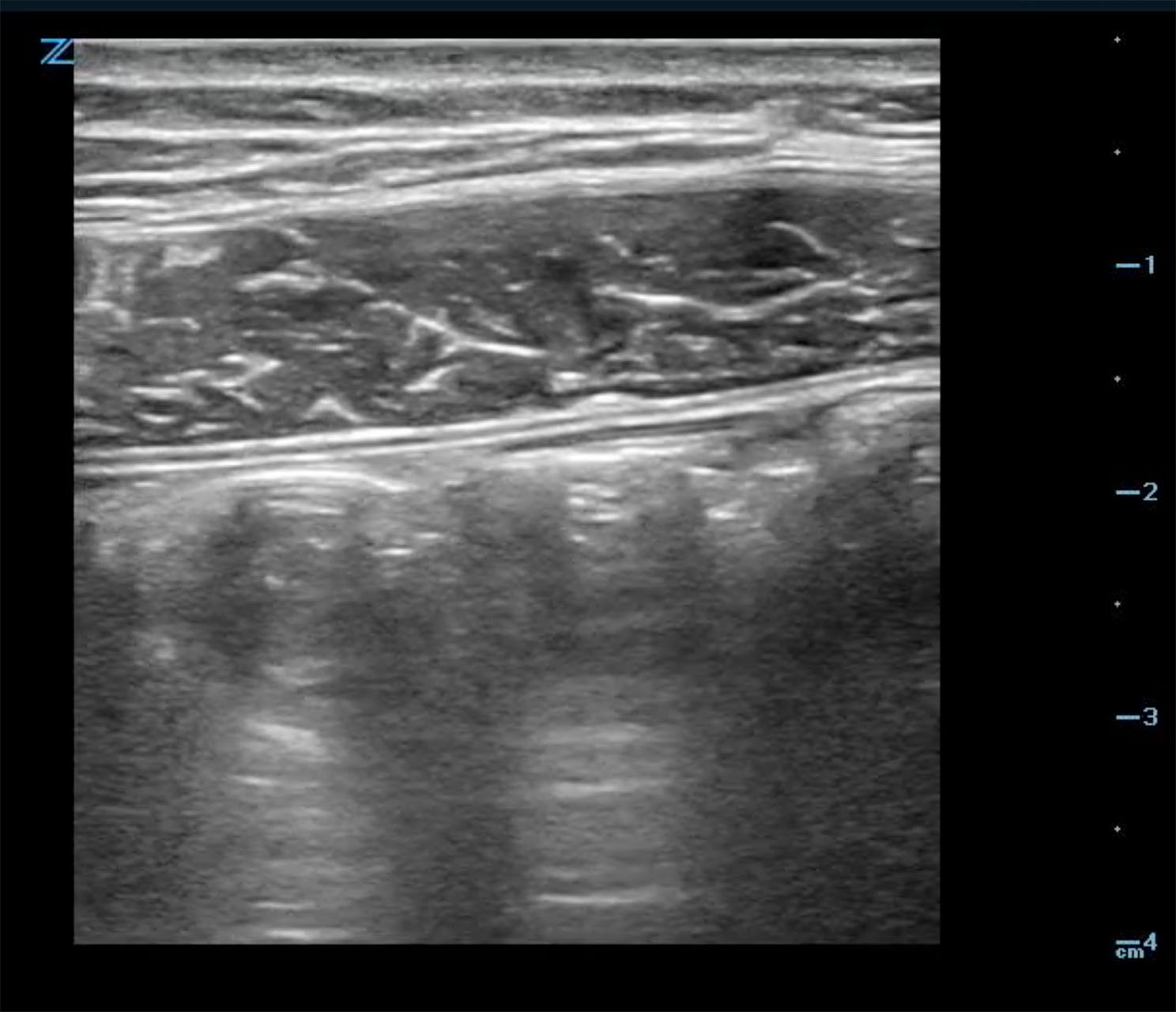
- Start in the RLQ with slow, steady pressure (graded compression) and find the psoas muscle. (Fig. 3)
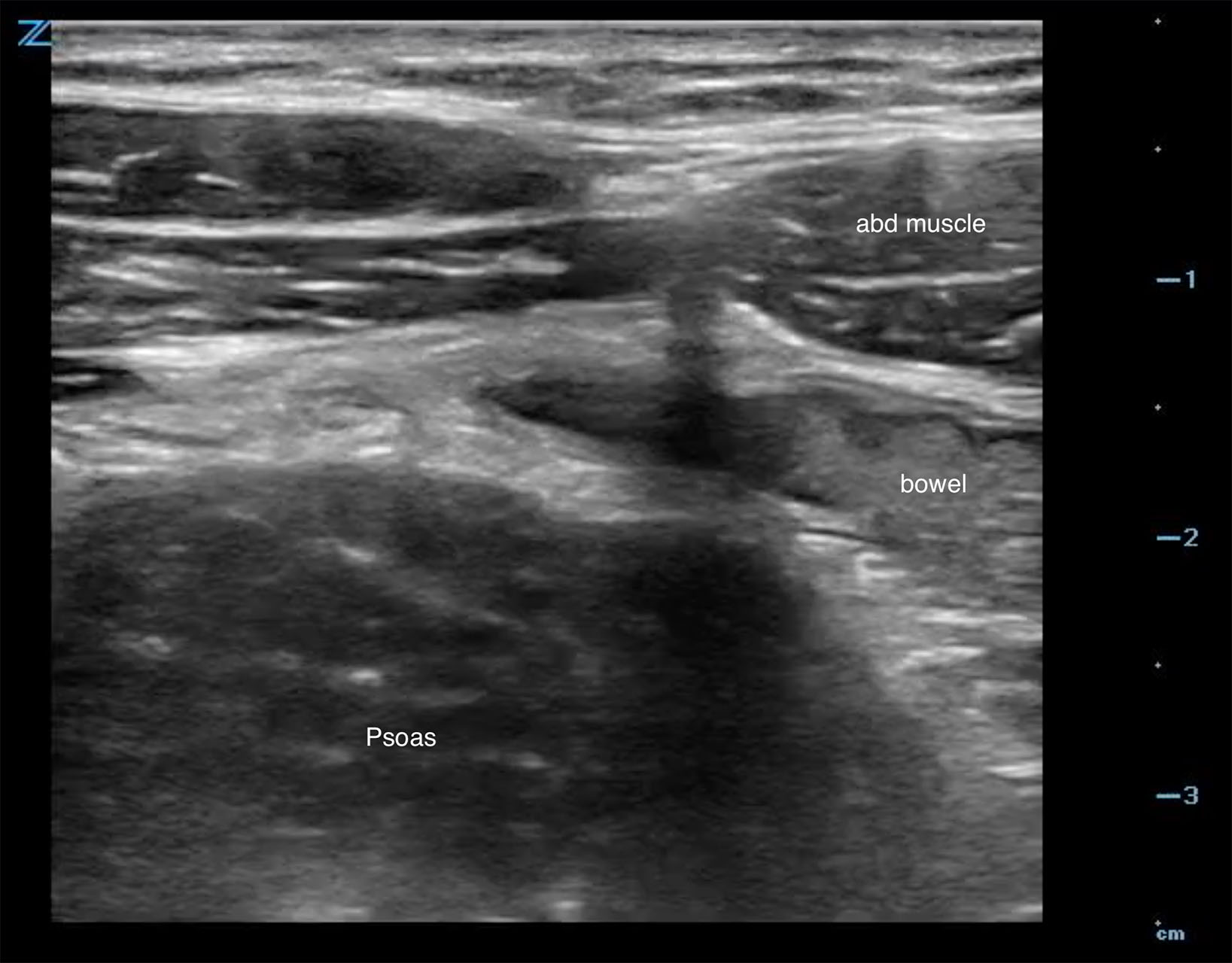
- Figure 3. The psoas muscle is seen here posterior to the anterior abdominal musculature in the RLQ
- Hold the transducer motionless to look for forward flow of bowel contents. This suggests normal peristalsis of the terminal ileum. (Video 1a, 1b)
- Video 1a. Normal peristalsis of bowel
- Video 1b. Normal peristalsis of bowel
- Sweep the transducer with continued graded compression towards the patient’s head (superiolaterally) into the RUQ.
- Rotate the transducer 90 degrees so the indicator is pointing towards the patient’s head. Sweep the transducer with continued graded compression towards the patient’s LUQ.
- Turn the indicator marker towards the patient’s right. Sweep the transducer with continued graded compression towards the patient’s LLQ.
- The ultrasound is completed after all four quadrants are evaluated.
- Normal findings
- Normal colon (Fig. 4) has haustra which are seen in the long axis view. Colon can be differentiated from small bowel by size and aperistalsis; but take care to not confuse with dilated loops of small bowel. (Fig. 5)
- Normal bowel often creates artifact due to bowel gas which looks like bright echoes with shadowing. If stool is present it can appear to have mixed echogenicity.8 Notably, identify where the ileum terminates into the cecum.
- Look for forward flow of bowel contents and normal peristalsis of the terminal ileum. (Video 1)
- Figure 4. Normal colon in long axis view
- Figure 5. Dilated loop of small bowel seen in long axis
- Measurements and reference ranges for relevant structures
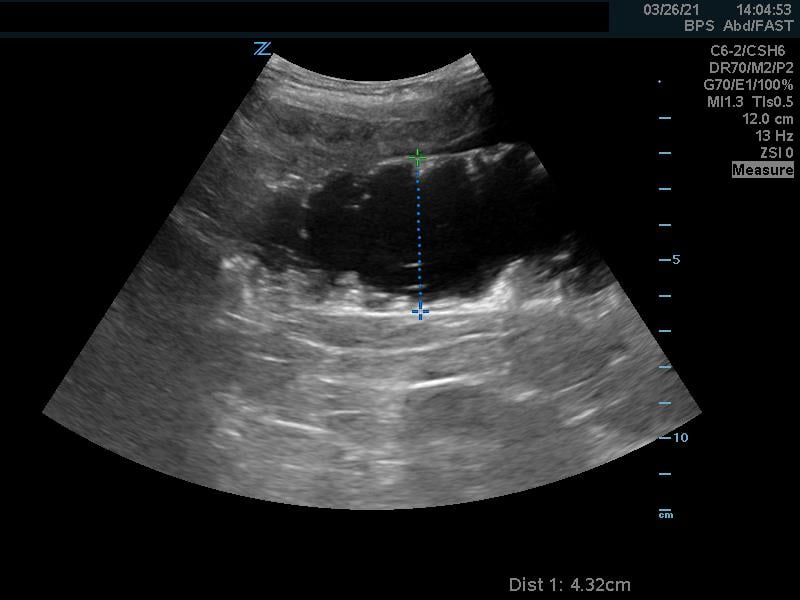
- The intussusception is usually 3-5 cm in diameter and often fills the screen, which makes it easier to diagnosis by point-of-care ultrasound.8
IV. Pathology
- Significance of pathology (morbidity and mortality)
- Missed diagnosis can lead to ischemic bowel, necrosis and perforation. Also, enema reduction of intussusception is often less successful in the delayed diagnosis due to worsened bowel wall edema.
- Ultrasound can predict failure in enema reduction through the following findings: trapped free fluid, intramural air, or absence of flow on Doppler imaging.8
- Intussusception can resolve and recur. It is possible to have a positive point-of-care ultrasound and a negative radiology ultrasound or vice versa.
- Incidence of pathology
- In the first year of life 38 per 100,000 live births are affected; in the second year of life 31 per 100,000 live births are affected.9
V. Pearls and Pitfalls
- Perforated appendicitis can be confused for intussusception because the fat surrounding the appendix appears hyperechoic due to inflammation.10 Therefore, take the entire clinical picture into account prior to making a definitive diagnosis
- Sonographic evidence of bowel obstruction (including dilated, fluid-filled loops, free-fluid between bowel, and to-and-fro peristalsis) may be noted proximal to the area of intussusception. (Videos 2 and 3)
- Video 2. Dilated loops of bowel, free fluid and to-and-fro peristalsis showing small bowel obstruction proximal to the intussusception
- Failing to use continual graded compression while sweeping the abdomen will lead to less optimal visualization due to artifact from bowel gas.
VI. Tips on Image Acquisition and Interpretation
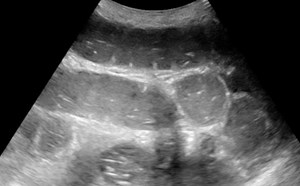
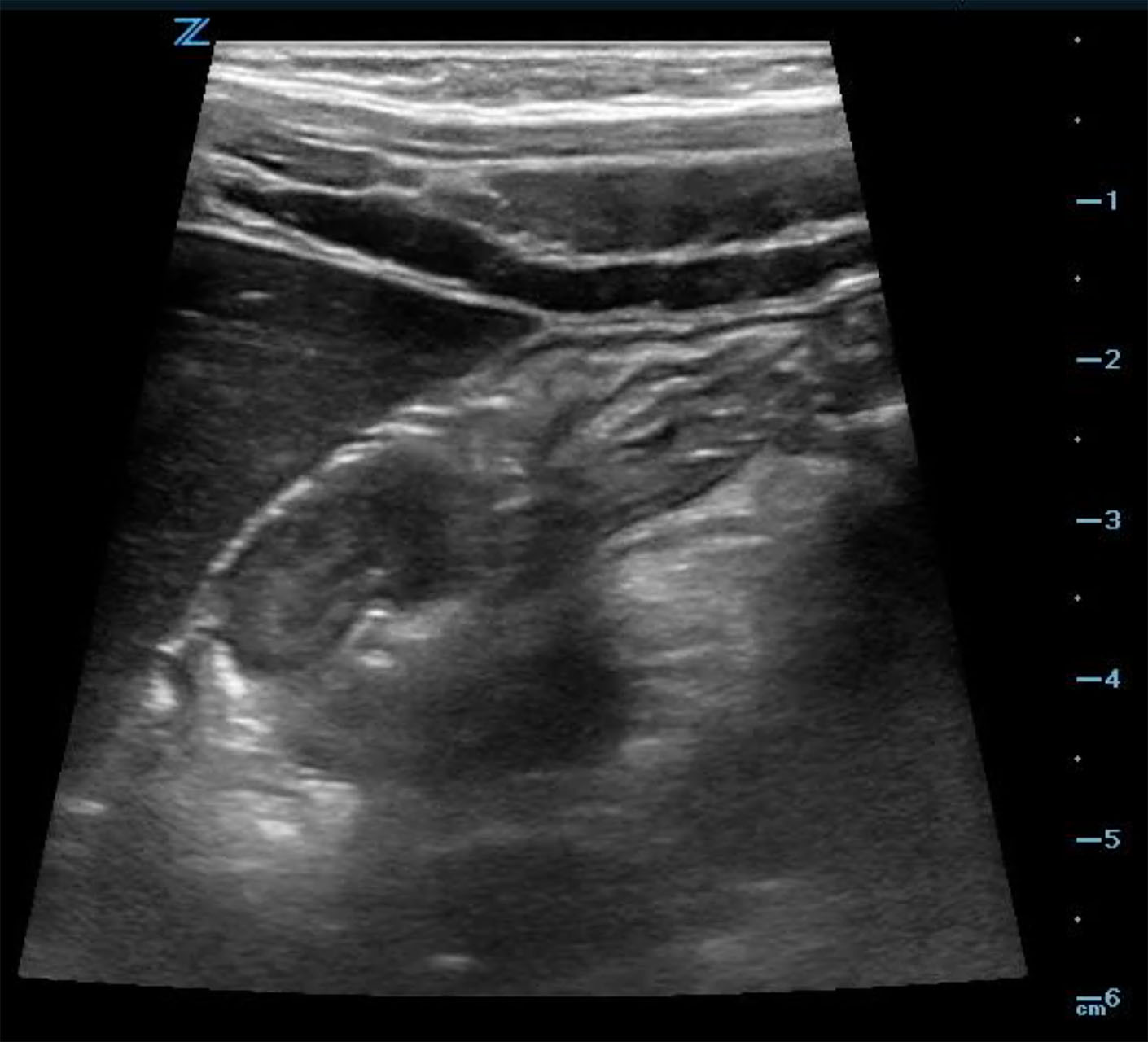
- When the intussusception is seen it should be imaged in both long (Fig. 6a, Video 3) and short (Fig. 6b, Video 3) axis.
- In the long axis, a kidney-shaped mass, which is often called the pseudokidney sign, is seen. This is an oblique view of the invaginated bowel. (Fig. 6a)
- In the transverse axis, a target or doughnut sign, is seen. This is a cross sectional view of a mass made up of invaginated bowel intussusceptum and receiving bowel intussuscipiens, which creates the appearance of concentric rings. (Fig. 6b)
- Identifying surrounding free fluid can be useful in prognostication and is an important finding to discuss with a consultant. (Video 2)
- Sometimes a mass can be palpated on physical exam, which can be useful in guiding your scanning location.
- Make sure to scan any palpable mass in multiple planes.
- Video 3a. Intussusception in short axis
- Video 3b. Intussusception in long axis
- Figure 6a. Image in long axis of ileocolic intussusception

- Figure 6b. Image in short axis of ileocolic intussusception
VII. Common Mistakes
- Scanning only the RUQ will miss a minority of cases.
- One study suggested that fecal matter in the colon is the most common mimic of intussusception.8
- Another mimic of intussusception is bowel wall hematoma and bowel wall edema associated with Henoch-Schonlein purpura.8
VIII. References
- Morrison J, Lucas N, Gravel J. The role of abdominal radiography in the diagnosis of intussusception when interpreted by pediatric emergency physicians. J Pediatr. 2009;155(4):556-9.
- Budwig K, Rothrock SG, Sudhipong V, et al. Misdiagnosis of pediatric intussusception. Ann Emerg Med. 1994;23(3):611-612.
- Wolford RW, Browning B. 237 Retrospective review of symptoms and signs of intussusception present on initial evaluation. Ann Emerg Med. 2015;66(4):Supplement, Page S86.
- Hryhorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009;39(10):1075-9.
- Riera A Hsaio AL, Langhan ML, et al. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med. 2012;60(3):264-8.
- Parashar UD, Holman RC, Cummings KC, et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000;106(6):1413-21.
- Roeyne G, Jansen M, Hubens G, et al. Intussusception in infants: An emergency in diagnosis and treatment. Eur J Emerg Med. 1999;6(1):73-6.
- Ma, et al. Ma and Mateer’s Emergency Ultrasound. McGraw-Hill Education. 2014. Print
- Buettcher M, Baer G, Bonhoeffer J,et al. Three-year surveillance of intussusception in children in Switzerland. Pediatrics. 2007;120(3):473-80.
- Doshi V, Ho CH, Chan RY. A Perplexing “Target Sign.” J Pediatr. 2016;169:324.