ENT
Lucas Friedman, MD and Srikar Adhikari, MD, MS, FACEP
Ear, nose and throat (ENT) pathology are a common cause of complaints in the emergency department (ED). ENT emergencies vary widely from infectious, like tonsillitis, peritonsillar abscess, chondritis, sinusitis, dental abscess, to traumatic, such as facial fractures. Point-of-care ultrasound (POCUS) has become a valuable tool in patient care, with the benefits of being noninvasive, nonionizing, inexpensive, rapid and repeatable at the bedside.
- General indications: Swelling, pain, trauma, odynophagia/dysphagia, trismus, drooling, hoarseness and neck masses. A common mnemonic that can be utilized for differential diagnosis is VINDICATE:
- Vascular (Carotid Paraganglioma, pseudoaneurysm, etc.)
- Infection (Cat-scratch disease, abscess, etc.)
- Neoplasm (Warthin’s tumor, schwannoma, lipoma, etc.)
- Drugs (Sialadenitis sequela)
- Inflammatory/Idiopathic (Sialadenitis, esophageal diverticulum, etc.)
- Congenital (Thyroglossal duct cyst, 2nd branchial cleft cyst, etc.)
- Autoimmune (Sjogren’s syndrome, etc.)
- Trauma/Iatrogenic (Hematoma, arteriovenous fistula, etc.)
- Endocrine (Parathyroid adenoma, etc.)
Follow these links to the following sections:
EARS
I. Introduction and Indications
- Various ear pathologies from tumors, cysts, trauma and infection may occur. One common cause is ear piercing in the auricle, which is inherently more risky than in the lobe, because of the possibility of cartilage infection.
- Perichondritis is a connective tissue infection that covers the cartilaginous auricle or pinna, but the cartilage is also typically involved. Perichondritis/Chondritis can develop an abscess and progress into a liquefactive chondritis causing permanent disfigurement.
- Case reports and expert opinion comprise the majority of ultrasound evidence.
- In addition to diagnosing and documenting the degree of pathology, a common indication for POCUS is the evaluation for the presence of an imbedded foreign body in the lobe of the ear.
II. Anatomy
- Relevant anatomy:1
- Skin (Epidermis/Dermis)
- Underlying Cartilage
- Subcutaneous tissue
- Landmarks:
- Antihelix border site for measurement
- Antihelix border site for measurement

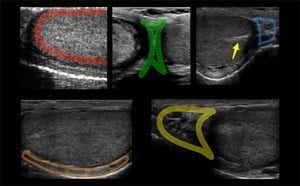
- Figure 1 and 2. Normal Ear
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- For anechoic structures, such as abscess, color Doppler and compression techniques can further help confirm findings.
- Superficial structures can be better visualized using an acoustic standoff pad or large amount of gel between the transducer and skin.
- Adjacent structures, such as vessels, nerves and lymphatics should be visualized, particularly when planning an invasive procedure, such as a needle aspiration or incision and drainage, so one can avoid injuring these other structures.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Cartilaginous structures appear homogeneously hypoechoic.
- Scanning technique1
- Probe selection: High frequency, 8 to 12 MHz linear transducer
- Scanning approach
- Transverse and longitudinal planes
- Color Doppler and cartilage measurement
- Normal findings
- Normal Cartilage:
Video 1. Normal Ear - Anterior and posterior skin layers have thin hyperechoic appearance.
- Middle layer containing cartilage appears as a thin hypoechoic band.
- Measurements:
- At the antihelix border the cartilage is thicker; the mean thickness is 0.8 ± 0.1 mm (at the middle third of the antihelix in transverse axis).
- At the lobule the mean thickness is 6.9 ± 1 mm.
- Normal Cartilage:
IV. Pathology
Chondritis/Perichondritis
- Infectious and traumatic disruptions in the blood supply, particularly if left untreated, develop the sequelae of “cauliflower ear.”
- Incidence:3
- 6% in post-operative patients on prophylactic antibiotics (Mohs reconstruction of auricular cartilage)

- Figure 3 and 4. Chondritis
Videos 2 and 3. Chondritis (Video 2) and Chondritis with Color Doppler (Video 3) - The tract of the earring or piercing appears as a hypoechoic area that follows the axis of insertion.
- Both the dermal layer and the cartilage have increased thickness and echogenicity.
- Sonographically, the thickened cartilage has a beaded appearance.
- The dissecting fluid collections divide the normally uniform 1-layer hypoechoic cartilage into a 2-layer structure resulting in double hypoechoic cartilage band.
- 6% in post-operative patients on prophylactic antibiotics (Mohs reconstruction of auricular cartilage)
V. Pearls and pitfalls
- Placing the patient in a lateral decubitus position.
- Place a piece of cotton inside the external meatus to avoid gel entering the external auditory canal.
DENTAL
I. Introduction and indications
- Ultrasound has been found to be valuable in the diagnosis and treatment of odontogenic facial abscess. When there is clinical concern for a dental infection with associated facial involvement (swelling, erythema, etc.), ultrasound can confirm an abscess formation in the superficial facial spaces, and reliably detect the stage of infection.
- Ultrasound can separate solid masses from fluid accumulations and determine the depth and extent of the fluid.
- Sensitivity and specificity of POCUS in diagnosing a dental abscess are 92% and 100%, respectively.4
II. Anatomy
- Relevant anatomy:
- Skin, underlying buccal mucosa, apposing alveolar mucosa, periapical space and bone
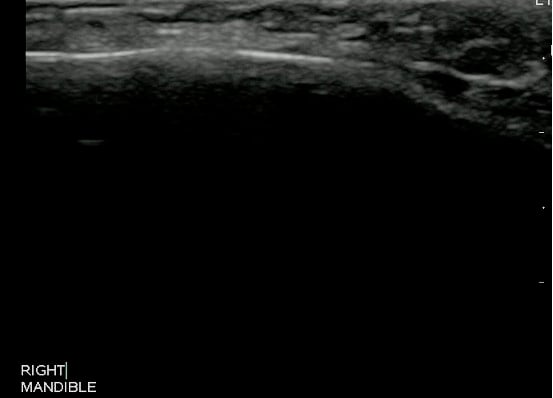

- Figure 5 and 6. Normal Mandible
- Skin, underlying buccal mucosa, apposing alveolar mucosa, periapical space and bone
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- For anechoic structures, such as abscess, color Doppler and compression techniques can further help confirm findings.
- Adjacent structures, such as vessels, nerves and lymphatics should be visualized, particularly when planning an invasive procedure, such as a needle aspiration or incision and drainage, so one can avoid injuring these other structures.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Muscles are generally visualized as hypoechoic structures but have a more heterogeneous striated appearance.
- Scanning technique4
- Probe selection:
- A high frequency, 8 to 12 MHz linear transducer.
- Scanning approach:
- Probe positioned outside the mouth against the skin corresponding to the area of interest.
- Scanning in two planes, both transverse and longitudinal, using color Doppler and compression can be used to determine if a subcutaneous mass is cystic, solid or complex.
- Ultrasound can also provide information regarding the depth and extent of the fluid collection.
- Probe selection:
- Normal Mandible:
-
Video 4. Normal Mandible
-
- Measurements:
- The objective identification of the size and depth of the fluid collection can assist in incision and drainage.
Pathology
Dental Abscess
- Mandibular Periapical Abscess:

- Figure 7. Mandibular Periapical Abscess
Video 5. Periapical Abscess - Maxillary Periapical Abscess:
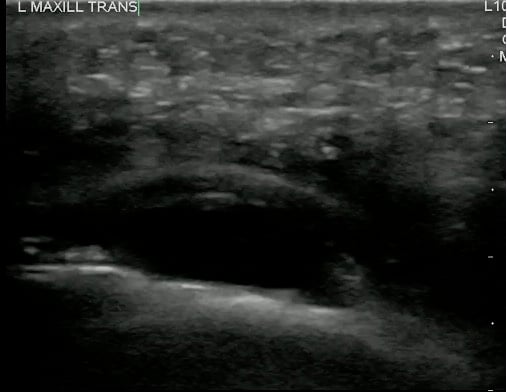
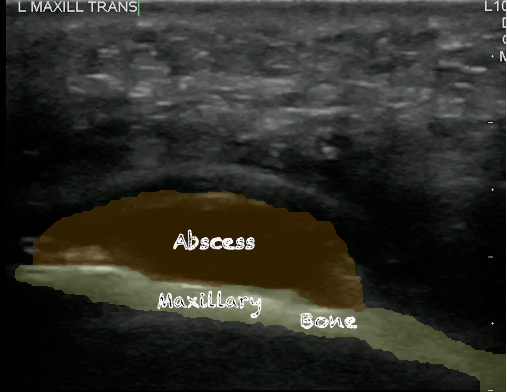
- Figure 8 and 9. Maxillary periapical abscess
Video 6. Periapical abscess with color Doppler
- Significance of pathology:
- Dental infections can have multiple sequelae, including Ludwig’s Angina, which has an 8% mortality.5
- Incidence of pathology: 4
- 22 million people with dental pain in any 6-month period
- 28% of dental claims from the ED related to periapical abscess
- Although abscesses can have a variety of sonographic appearances, the most common appearance is that of a hypoechoic mass relative to adjacent structures, or entirely anechoic.
- It can appear as a complex mass with scattered echoes that represent necrotic debris or tissue.
- Abscess cavity may contain septae or gas within it.
- Color Doppler may demonstrate hyperemia around the abscess cavity and absence of flow within it.
V. Pearls and pitfalls
- Ultrasound can be used to drain an abscess in real time. One will be able to visualize the scalpel or needle while inserting into the abscess cavity and can ensure that the pocket has been adequately drained.
- Awareness of anatomic proximity to adjacent structures like arteries, veins, ducts, lymph nodes and nerves will avoid serious complications.
Lymph Nodes
I. Introduction and Indications
- Ultrasound is a useful imaging modality in the assessment of neck masses.6,7 It can distinguish an abscess from cervical lymphadenitis, thus guiding further evaluation and treatment.
- Unfortunately, up to 30% of malignant lymph node infiltration occurs in lymph nodes less than 5 mm.8 However, with the development of contrast enhanced ultrasound (CEUS) and elastography, we may be able to more accurately differentiate these malignant lymph nodes from benign pathology.
- Although ultrasound is often used to determine metastasis and guide fine-needle aspiration, the primary POCUS application is to evaluate for sonographic evidence of lymphadenitis.
II. Anatomy
- Relevant anatomy:2,9
- Lymph node size, shape, parenchyma, the hilum, and margin with surrounding tissues
- Solitary versus multiple
- Comprehensive scanning includes:
- Submental and submandibular, parotid, and jugulodigastric regions (levels I and II)
- Carotid and internal jugular vessels to the clavicle (levels III and IV)
- Anterior portion of the posterior triangle to superior aspect of the clavicle to the trapezius muscle (level V) is accomplished. Then the posterior aspect, trapezius to the mastoid tip (level V).
- Midline region from the hyoid bone to the manubrium (level VI)
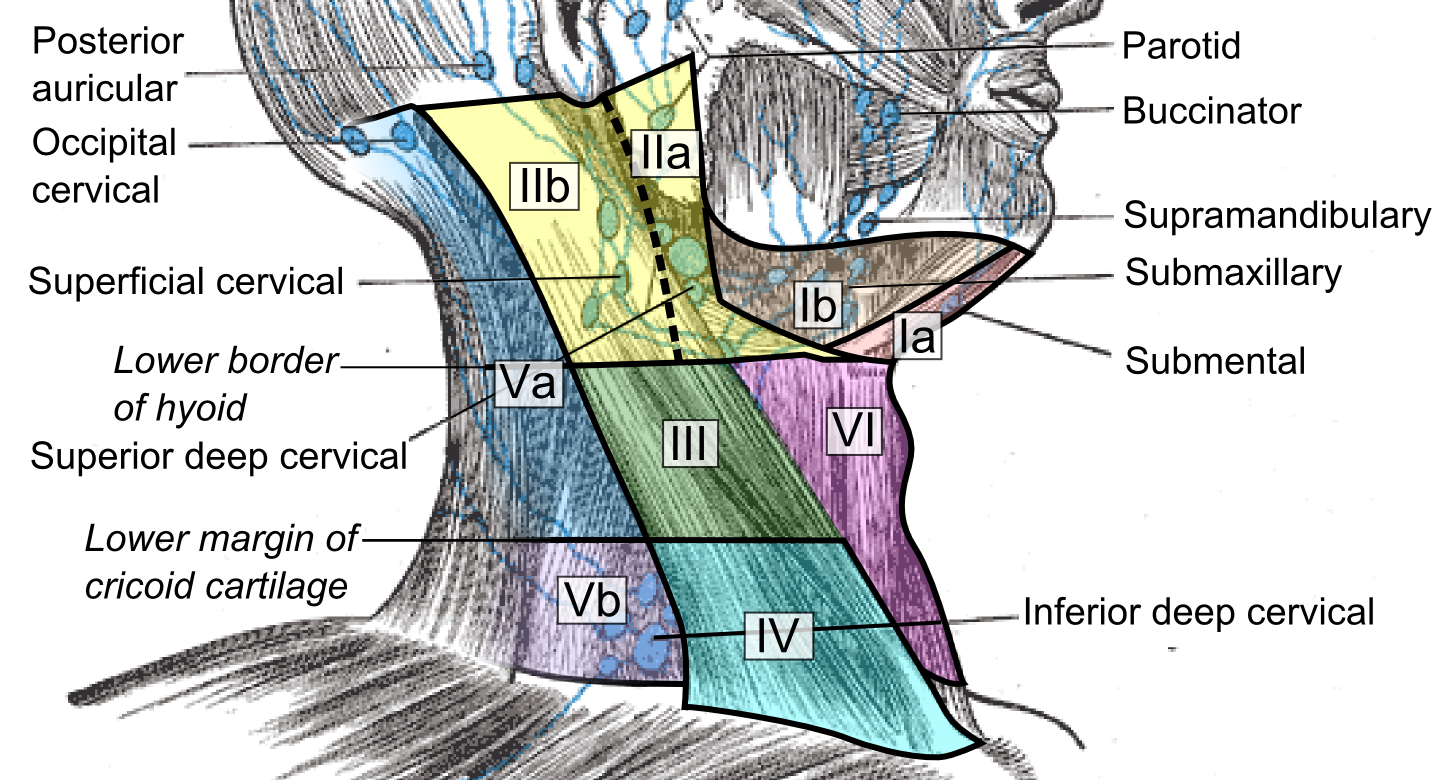
- Figure 10. Lymph Node Levels (https://commons.wikimedia.org/w/index.php?curid=78128747)
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Muscles are generally visualized as hypoechoic structures but have a more heterogeneous striated appearance.
- Glandular structures such as thyroid look homogeneous and are more echogenic in comparison with adjacent soft tissues, and muscles.
- Scanning technique9
- Probe selection: High frequency, 8 to 12 MHz linear transducer
- Scanning approach:
- Transverse, anteroposterior, and longitudinal planes
- Gray scale and power Doppler sonographic features are very helpful in differentiating neck masses.
- Doppler settings should be optimized for detecting low velocity flow. Doppler settings should be standardized for high sensitivity with a low wall filter and low pulse repetition frequency.
- Screen for the presence of macrocalcifications, colloid, cyst formation, and other unique findings.
- Videos 7 and 8. Lymph nodes
- Normal lymph node
- Oval in appearance
- Echogenic hilum
- Homogenous in echotexture
- Doppler blood flow is seen branching radially from the hilum and no flow is seen in the periphery
Video 9. Color doppler on lymph node 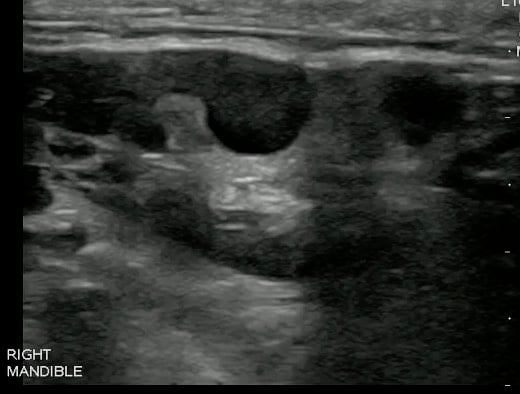
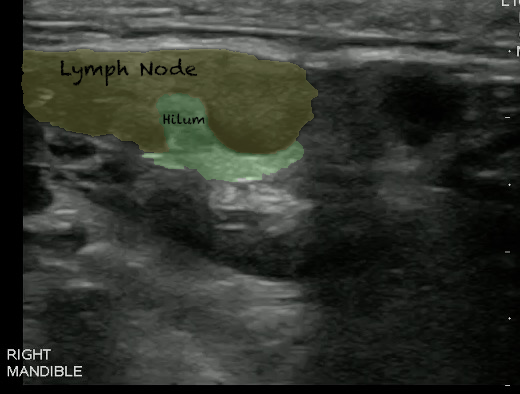
- Figures 11 and 12. Lymph Node
IV. Pathology
Lymphadenitis
- Reactive lymphadenitis:
- Local infection or inflammation such as infections involving the pharynx, salivary glands, and scalp often cause reactive lymphadenitis.
- Normal reactive lymph nodes are enlarged, hypoechoic when compared with the surrounding structures. They still remain oval in shape.
- Vascularity is still confined to hilum of the lymph node and may be increased.
- Color Doppler of reactive lymphadenitis shows vascularity (normal along the hilum) which can differentiate from abscess cavity which has no flow within it.
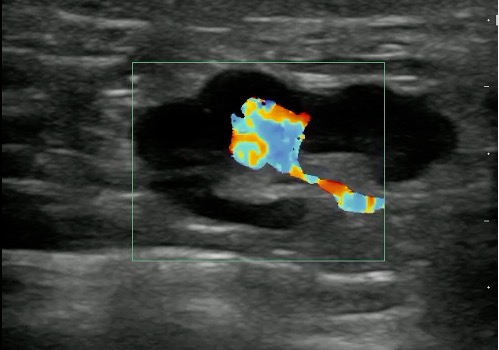
Figure 13 and Video 10. Reactive lymph Node with increased Color Doppler
- Abnormal lymph nodes (malignancy or metastasis):
- Round in shape (Nearly equal measurements in all axes)
- No echogenic hilum is seen
- Echotexture is heterogeneous
- Cystic degeneration (Intranodal necrosis)
- Large dimensions
- Microcalcifications
- Irregular margins and cortical thickening
- Through transmission
- Peripheral or transnodal vascularity is seen on power Doppler imaging
Video 11. Malignant lymph nodes
V. Pearls and pitfalls
Lymph Node
- Useful gray scale features include size, shape, echogenicity, intranodal necrosis, and calcification.10
- Lymph nodes in lymphomas may be indistinguishable from reactive lymph nodes.11
- Pattern of vascularity helps to distinguish reactive lymphadenitis vs. malignancy. Central in Lymphadenitis and peripheral and irregular in Lymphoma.
- A lesion within a lymph node that has internal vascularity on color Doppler ultrasound often portends a more serious pathology, such as malignancy, and should undergo follow up imaging and specialty consultation.
- Useful power Doppler features include vascular pattern and displacement of vascularity.
- Vascular patterns on color/power Doppler sonography can help differentiate normal from abnormal lymph nodes.10
- Especially in pediatric neck masses, one needs to consider alternative diagnosis from the more common lymphadenitis or abscess, such as congenital lesions:
- Lymphangioma
- Hemangioma
- Parotid cyst
- Branchial cleft cyst
- Thyroglossal duct cyst
- Parathyroid and thymic cysts
- Undescended thyroid gland
Salivary Glands
I. Introduction and Indications
- Sonography has been used for decades in the diagnosis of the salivary gland pathology.12 Although in the United States CT and MRI are often considered the first line imaging modalities, in Europe and Asia ultrasound is often used initially.13
- Ultrasound can be used in facial swelling to evaluate for infectious/inflammatory diseases, sialolithiasis, sialosis/sialadenosis, Sjogren syndrome, neoplasms, cysts, and trauma.
- Even if one is able to clinically correlate facial swelling to a glandular structure, there are numerous disease states that require imaging to differentiate.
- Evidence for ultrasound diagnosis of Sialolithiasis varies (Sensitivity and Specificity of approximately 80%).14,15
II. Anatomy
- Relevant anatomy:13
- Triangular parotid gland
- Superficial and deep lobes divided by plane in which the facial nerve is located, which is superficial to the retromandibular vein and lateral to the external carotid artery.
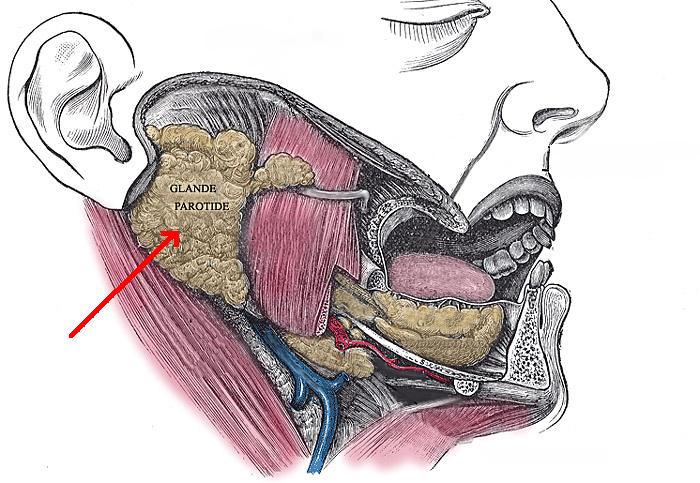
- Figure 14. Parotid gland (https://commons.wikimedia.org/w/index.php?curid=4024415)
- The difficult to visualize facial nerve and deep lobe of the parotid obscured by the mandible, can be compensated by visualization of the retromandibular vein as a sonographic landmark separating the superficial and deep lobes of the parotid gland.
- The superficial lobe overlies the masseter muscle, extending posterior to the angle of the mandible.
- Intraparotid lymph nodes are frequently found in the parenchyma of the upper and lower poles.

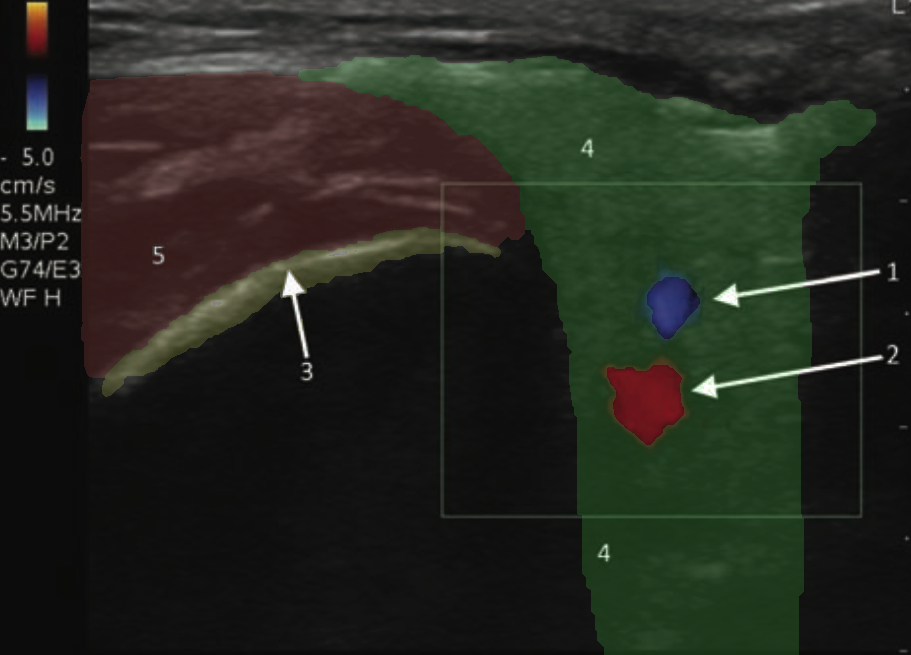
- Figure 15 and 16. Transverse view of normal left parotid gland with color doppler on vessels (1- Retromandibular vein; 2- External carotid artery; 3- Surface of the mandible; 4- Parotid gland; 5- Masseter muscle)
- Superficial and deep lobes divided by plane in which the facial nerve is located, which is superficial to the retromandibular vein and lateral to the external carotid artery.
- Triangular submandibular gland:
- Framed by the anterior and posterior bellies of the digastric muscle and the body of the mandible.
- The superficial and deep lobes connect around the border of the mylohyoid muscle.
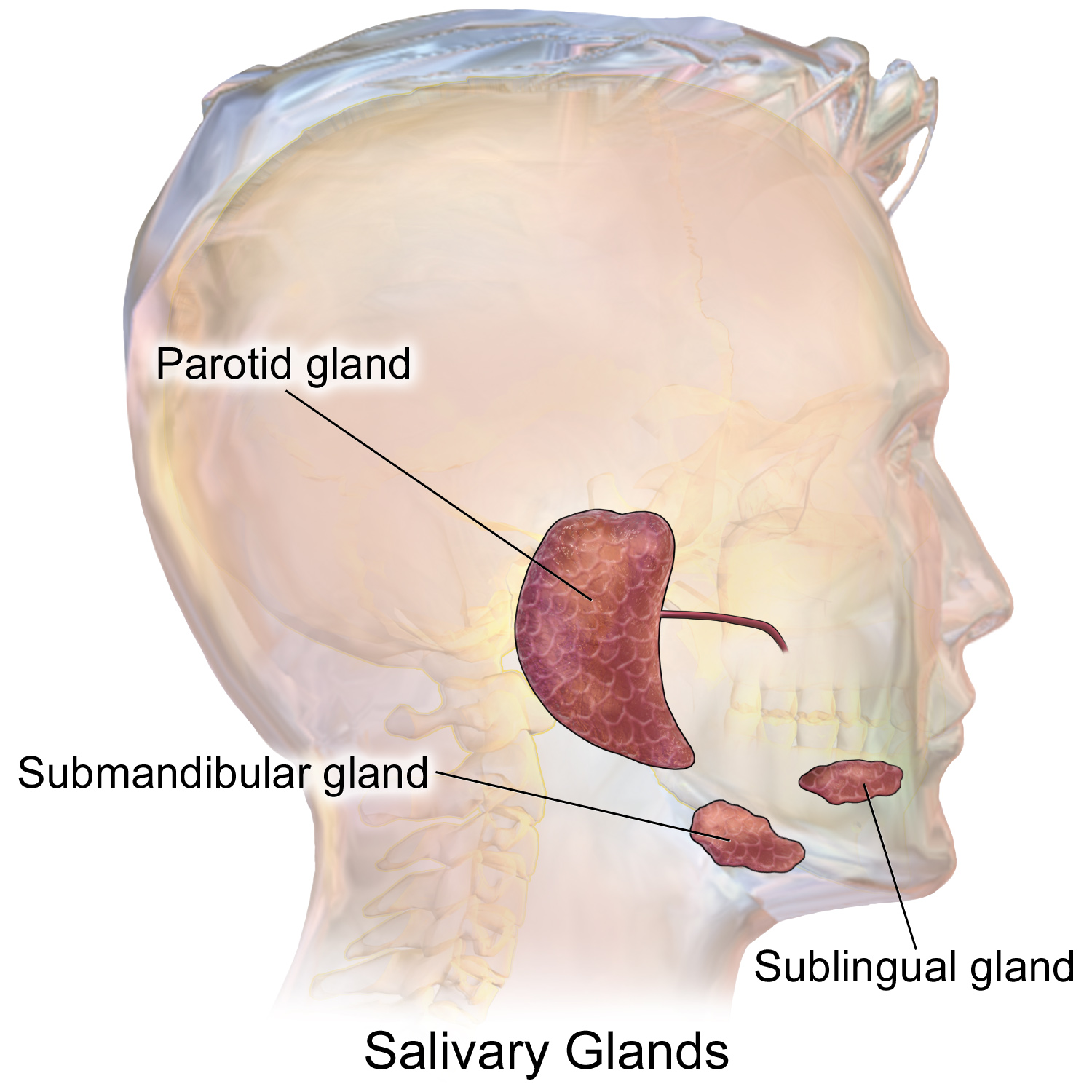
- Figure 17. Normal submandibular gland (https://commons.wikimedia.org/wiki/File:Blausen_0780_SalivaryGlands.png)
- Triangular parotid gland
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- For anechoic structures, such as abscess, color Doppler and compression techniques can further help confirm findings.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Cartilaginous structures appear homogeneously hypoechoic.
- Muscles are generally visualized as hypoechoic structures but have a more heterogeneous striated appearance.
- Glandular structures such as thyroid look homogeneous and are more echogenic in comparison with adjacent soft tissues, and muscles.
- Scanning technique13
- Probe selection:
- High frequency, 8 to 12 MHz linear transducer
- Phased or curved-array transducer may be needed better visualize the parotid gland at the angle of mandible.
- Scanning approach:
- Scanning the salivary glands in at least two perpendicular planes (long and short axis) to assess for size, echogenicity, vascularity and ductal dilatation
- Parotid gland is visualized in front of the lower ear to the angle of the jaw, both parallel and perpendicular to the ear.
- Submandibular gland is visualized parallel and perpendicular to the mandible, with the probe placed inferior to the body of the mandible.
- Any abnormality in the surrounding anatomy including the lymph nodes should be evaluated.
- Contralateral side should be evaluated for comparison.
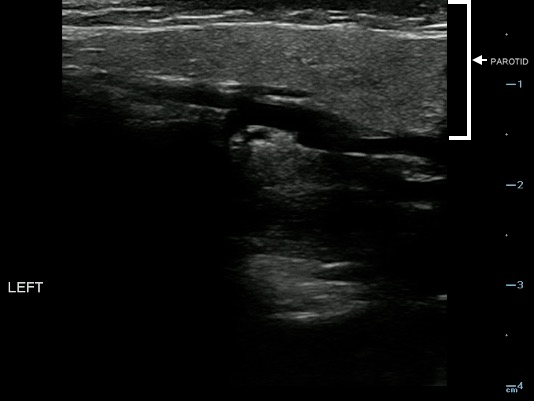
- Figure 18. Normal parotid gland (marked with arrow)
Video 12. Normal parotid gland
- Probe selection:
- Normal findings
- Sonographically, the normal parotid and submandibular glands appear homogeneous; the fatty glandular tissue composition causes an increased echogenicity relative to adjacent muscle.
- Parotid Gland:
- The homogeneity and echogenicity of the parotid gland is comparable to that of the thyroid gland.
- Normal intraglandular salivary ducts and the Stensen’s duct are generally not visualized with ultrasound.
- When dilated, Stensen’s duct is visualized superficially along the masseter muscle, typically 1 cm below the zygomatic arch.
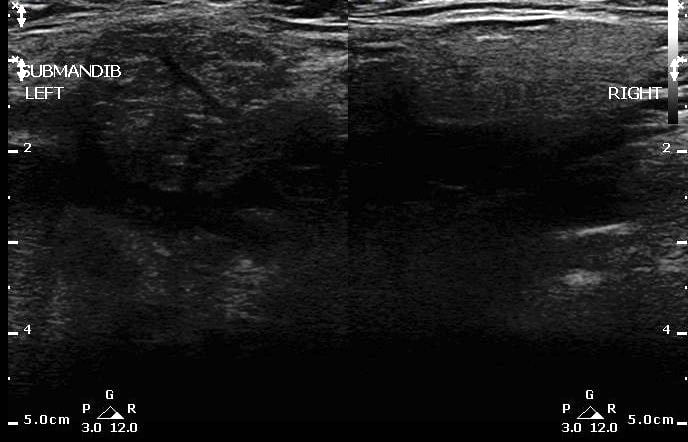
- Comparison of Sialadenitis on the left and normal submandibular gland on right:
- Measurements:
- Parotid short axis should be less than 5– 6 mm normally.13
- Submandibular Gland:
- Triangular in shape with a posterior base.
- More hypoechoic than parotid gland.
- Normal intraglandular ducts are rarely seen on ultrasound.
- The intraglandular ducts are seen as small linear hyperechoic stripes, including the Wharton duct, which emerges from the hilum and passes medially around the mylohyoid muscle. It can be clearly visualized when it is abnormally dilated.
Video 13. Normal submandibular gland
- Normal variants:
- The Parotid gland has intraglandular lymph nodes that are commonly seen within the parenchyma of the parotid gland.


- Figure 19 and 20. Parotid gland lymph nodes
Video 14. Parotid gland lymph nodes
- The Parotid gland has intraglandular lymph nodes that are commonly seen within the parenchyma of the parotid gland.
IV. Pathology
Sialoadenitis/sialolithiasis13
- Parotitis:
- Enlarged and hypoechoic salivary gland, with multiple enlarged, oval, hypoechoic intraglandular lymph nodes.
- Heterogeneous parenchyma with micro abscesses.
- Increased blood flow may be seen on Color Doppler. This increased vascularity is not seen in sialosis.
- Localized ductal dilatation or retention cysts may be seen.
- Abscesses-hypoechoic to anechoic lesions with posterior acoustic enhancement, avascular, and sometimes with moving debris, or hyperechoic foci from gas microbubbles. Typically with irregular borders, but as abscesses organize they become surrounded by a hyperechoic “halo.”13
- Figure 21. Sialadenitis (left) vs normal (right)

- Figure 22. Parotitis
Video 15. Parotitis
- Parotid gland sialolithiasis and Stenson duct dilation:
- Historically stones smaller than 2–3 mm were often missed because of the absence of acoustic shadow, however, these were studies from the 1980’s with inferior machine resolution.13
- Stones are visualized as hyperechoic lines/points with far-field shadowing, and often dilated proximal excretory ducts.
- Sialolithiasis can progress into suppurative sialolithiasis and abscess formation, as well as potential loss in glandular function.
- Incidence of sialolithiasis: Somewhere between 1 case annually per 10,000 to 300,000.15
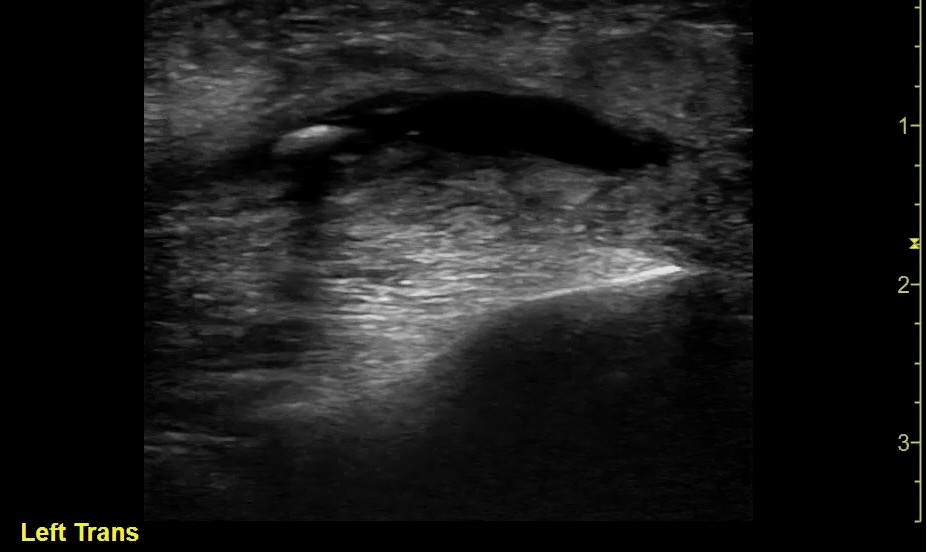
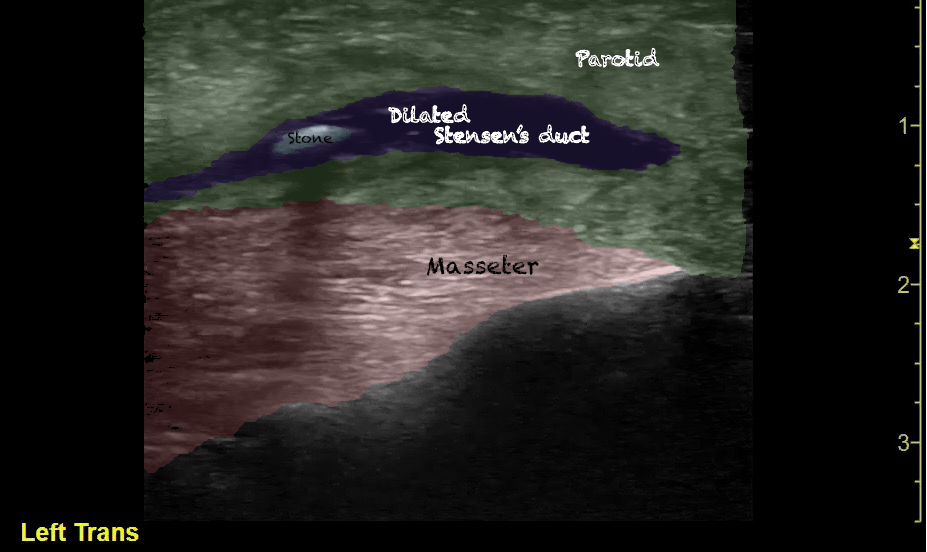
- Figure 23 and 24. Parotitis Sialolithiasis (Courtesy of Dr. Alejandro Alonso)
Video 16. Parotitis Sialolithiasis 
- Figure 25. Parotitis Sialolithiasis Coronal View (Courtesy of Dr. Alejandro Alonso)
Video 17. Parotitis Sialolithiasis Coronal
- Autoimmune disease (eg, Sjogren’s syndrome), granulomatous disease (eg, sarcoidosis), and neoplasms (eg, Warthin tumor, lymphoma, etc.) are often difficult to differentiate.
- For instance, sonographically, Sjogren syndrome often appears as an enlarged hyperechoic gland early, but may become multicystic with a reticular pattern and associated parenchymal atrophy, as well as intense hypervascularity.
- Submandibular gland sialoadenitis/sialolithiasis:
- Appears heterogeneous with dilatation of the salivary ducts.
- Increased vascularity can be seen on Doppler.
- Pus and debris may be visualized at the Wharton’s duct ostium in the floor of the mouth.
- Submandibular gland stone appears hyperechoic with distal acoustic shadowing.
V. Pearls and pitfalls
- Rotate head to the side opposite to the area of study.
- Color Doppler can help differentiate the salivary ducts from vessels.
Sinus
I. Introduction and Indications
- Rhinosinusitis affects more than 30 million adults in the United States annually.16 In the last few decades, ultrasound has been used to diagnose acute maxillary sinusitis as it is safe, noninvasive, inexpensive, rapid and repeatable at the bedside.
- Clinically distinguishing between rhinitis and sinusitis can be challenging.17 Although, ultrasound is not as accurate as CT and MRI, it is a more practical tool that can be routinely used for diagnosing uncomplicated sinusitis in ambulatory settings, and could potentially reduce unnecessary antibiotic use.18
- Ultrasound is very sensitive in detecting fluid in sinus cavities, with accuracies exceeding 90% for the diagnosis of maxillary sinusitis have been reported in otolaryngology (ENT) practices.17 Emergency physician performed POCUS compared to CT was shown to have a sensitivity and specificity are 81% and 89%, respectively, for maxillary sinusitis.19
II. Anatomy
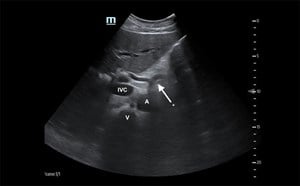
- Relevant anatomy:
- The maxillary sinus located in the maxillary bone caudal to the orbital floor, is lined by mucous membrane and normally filled with air. It is lateral to the nasal wall, with its floor cranial to the premolar and molar teeth. Of note, the posterior maxillary wall contains the pterygopalatine fossa.
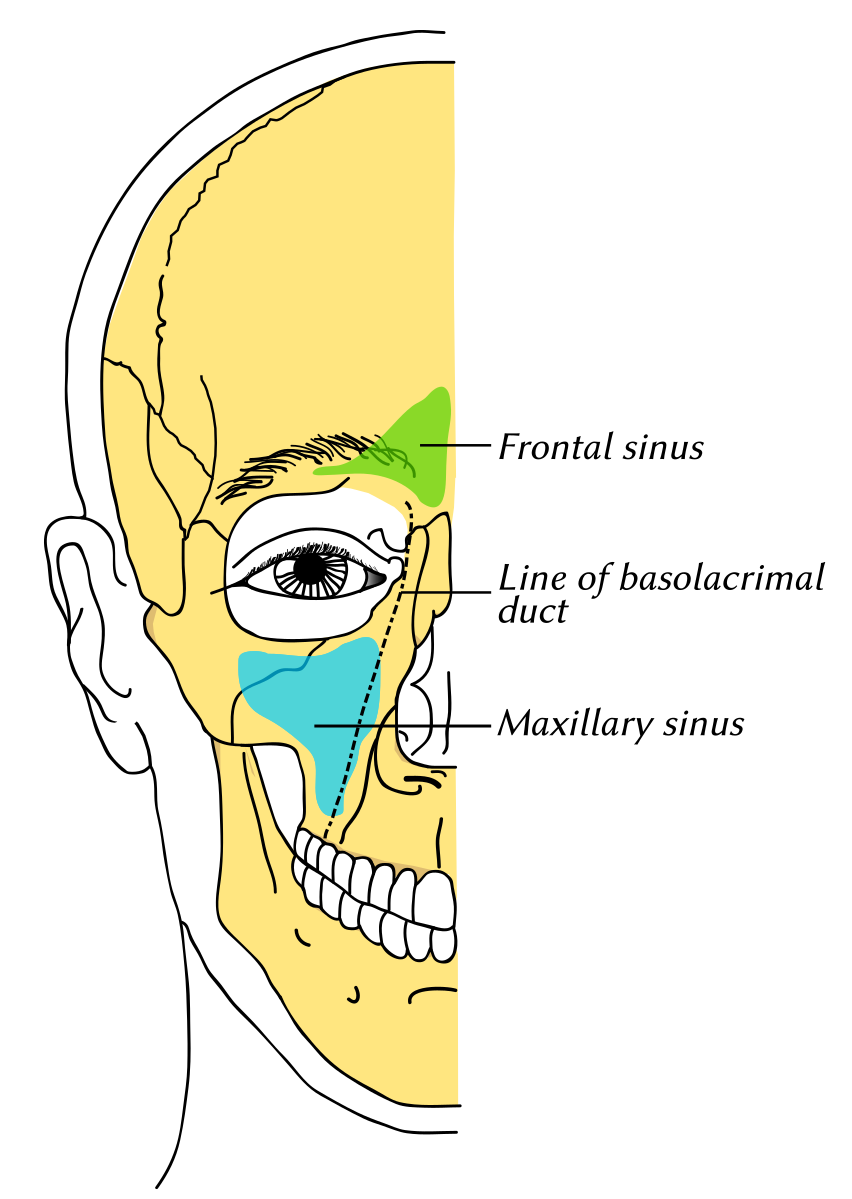
- Figure 26. Maxillary sinus (https://commons.wikimedia.org/wiki/File:Gray1199_en.svg)
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Muscles are generally visualized as hypoechoic structures but have a more heterogeneous striated appearance.
- Scanning technique20
- Probe selection:
- High frequency, 8 to 12 MHz linear transducer
- Begin scanning with highest frequency available for best resolution.
- Scanning approach:
- Of the paranasal sinuses, the maxillary sinuses are most amenable for POCUS.
- The scanning hand should be stabilized over the facial bones to prevent sliding.
- Scan between the nose and the zygoma, roam the orbital floor superiorly to the hard palate inferiorly.
- The depth setting should be adjusted to visualize entire sinus cavity.
- The gain should be appropriately adjusted to identify abnormalities and prevent artifacts.
- Scan both in sagittal and transverse planes.
- Adjust the gain to identify abnormalities and avoid artifacts.
- As always, the contralateral side should routinely be scanned for comparison.
Video 18. Scanning maxillary sinus
- Probe selection:
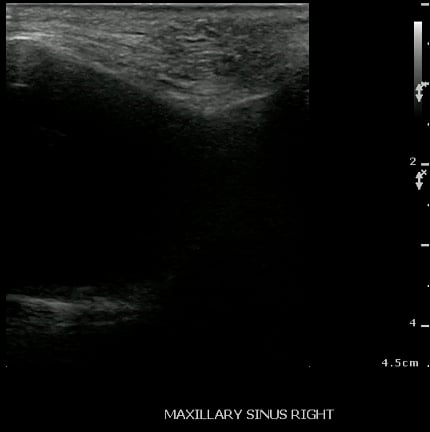
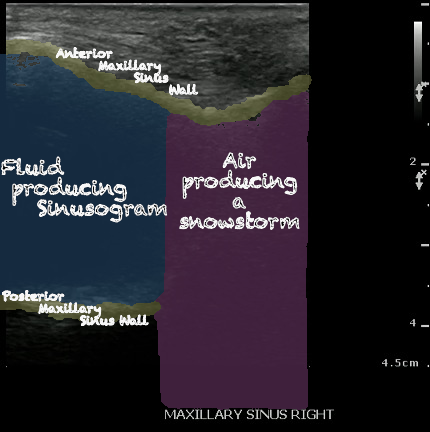
- Normal Maxillary Sinus:
- The normally air-filled maxillary sinus prevents the transmission of ultrasound beams (Air reflects most of the signal, thus preventing visualization of deep structures).
- The anterior maxillary sinus wall produces a bright echo in the near field, with reverberation artifact posteriorly (producing a snowstorm appearance), and preventing visualization of the posterior wall.
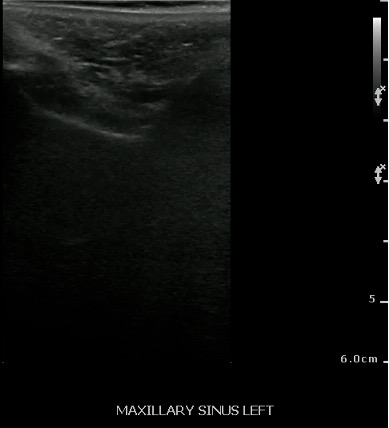
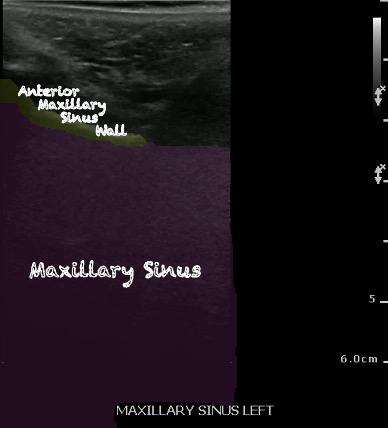
- Figure 27 and 28. Normal maxillary sinus
Video 19. Normal Maxillary Sinus
IV. Pathology
Maxillary sinusitis21
- Scanning in both the upright and supine positions can help differentiate acute sinusitis from mucosal thickening when a partial sinusogram is found (An image where the walls are not well defined).21
- Viral sinusitis, polyps, cysts, a mass or blood in the sinus can also produce the appearance of a sinusogram.
- Sinus fluid (Maxillary Sinusitis):
- Figure 29 and 30. Sinusitis
Video 20. Maxillary Sinusitis - Significance of pathology:
- More than 1 in 5 antibiotics prescribed in adults are for sinusitis.22
- Incidence:
- 1 in 8 adults in the United States (more than 30 million annually).22
- Rhinosinusitis is a common disorder, however, only 50% of patients presenting to the ED with sinus symptoms actually have acute bacterial sinusitis.16,23
- If the sinus cavity is fluid-filled, then the ultrasound signal will penetrate through the thin hyperechoic anterior wall, through the anechoic appearing fluid in the sinus cavity, and reflect off of the posterior walls, thus producing an image of the entire sinus cavity (Sinusogram) with the posterior wall of the sinus seen as a bright echogenic line in the far-field of the image.
V. Pearls and pitfalls
- The examination is done with the patient in an upright position; head tilted forward, so that any sinus fluid that is present will layer in the floor and against the anterior wall.
- Ultrasound is not helpful in differentiating between a viral and or bacterial sinusitis.
- Mucosal thickening can be mistaken for partially fluid-filled sinus cavity.
- Scanning in upright position can help differentiate between these two entities.
Thyroid
I. Introduction and Indications
- The topic of thyroid gland ultrasonography is extensive, including the various disease states, comprising entire textbooks, and sonographer specialization.
- Undiagnosed and untreated thyroid pathology can lead to significant morbidity and mortality.
- Ultrasound is often the first line imaging modality for thyroid pathology.
- Indications and clinical scenarios for which this examination should be used include:
- Masses, hyper/hypothyroidism, ultrasound guided fine needle biopsy (FNA), and surveillance
- Additionally, extra glandular pathology such as thyroglossal duct cyst may be present.
- Results from a congenital anomaly where segments of the duct fail to regress, resulting in an epithelial-lined cyst.
- 50% are diagnosed before 10 years of age.24
- It typically presents as a painless midline or near midline cervical location between base of the tongue and thyroid.
II. Anatomy
- Relevant anatomy:
- Normal Thyroid Isthmus and Bilateral Lobes
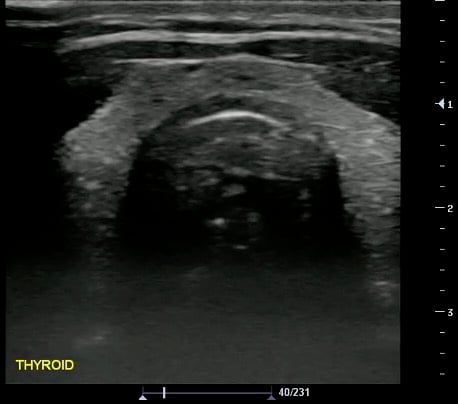
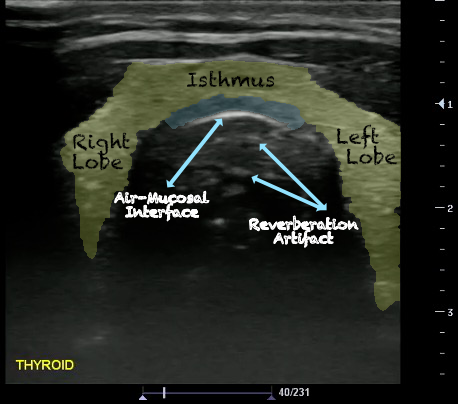
- Figure 31 and 32. Thyroid
- Figure 33. Neck Anatomy (https://commons.wikimedia.org/wiki/File:Structure_of_Adam%27s_apple.png)
- Normal Thyroid Isthmus and Bilateral Lobes
III. Scanning technique, normal findings and common variants
- High frequency, 8 to 12 MHz linear array transducer, which has low penetration, but high resolution should be used to examine the ear, face, and neck.2
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- Normal findings:
- Bony structures like mandible, maxilla appear hyperechoic with a posterior hypoechoic acoustic shadow underneath.
- Fat has hyperechoic appearance on ultrasound.
- Cartilaginous structures appear homogeneously hypoechoic.
- Muscles are generally visualized as hypoechoic structures but have a more heterogeneous striated appearance.
- Glandular structures such as thyroid look homogeneous and are more echogenic in comparison with adjacent soft tissues, and muscles.
- Scanning technique25
- Probe selection:
- A high frequency, 8 to 14 MHz linear transducer.
- Scanning approach:
- Extension of the neck
- Supine or semirecumbent position
- Longitudinal and transverse planes
- Probe selection:
- Normal findings
- Homogeneous ground-glass appearance
- Hyperechoic relative to adjacent muscles
Video 21. Normal Thyroid - Measurements:
- Obtained in 3 dimensions (anteroposterior, transverse, and longitudinal)
- Nodule > 10 mm concerning for malignancy (controversial; not the only criteria)
- Additional measurements: Isthmus thickness (Transverse > 5mm abnormal), Lobe volume (Width x Length x Depth x 0.5)
- Common Variants
- Normal parathyroid glands are usually not visualized
IV. Pathology
Thyroglossal duct cyst26
- Thyroglossal duct cysts typically related to hyoid bone:
- Often midline
- 25%-suprahyoid-submental region
- 75%-Infrahyoid or at the level of hyoid
- Variable sonographic appearance:
- Well-circumscribed anechoic cyst
- Increased through transmission
- Hypoechoic with internal debris
- No internal vascularity
- Heterogeneous pattern seen in repeated infections and hemorrhage due to prior aspirations
- Pseudo-solid echogenic appearance from proteinaceous contents secreted by epithelial lining

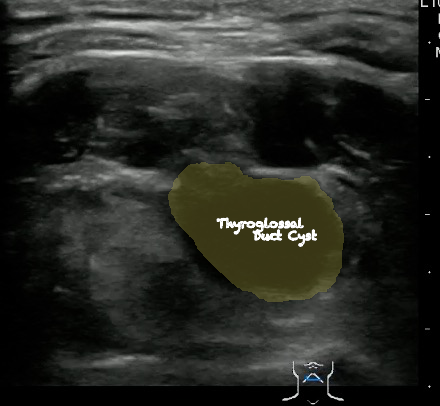
- Figure 34 and 35. Thyroglossal Duct Cyst
Video 22. Thyroglossal Duct Cyst
- Thyroglossal Duct Cyst with ring enhancement on CT:
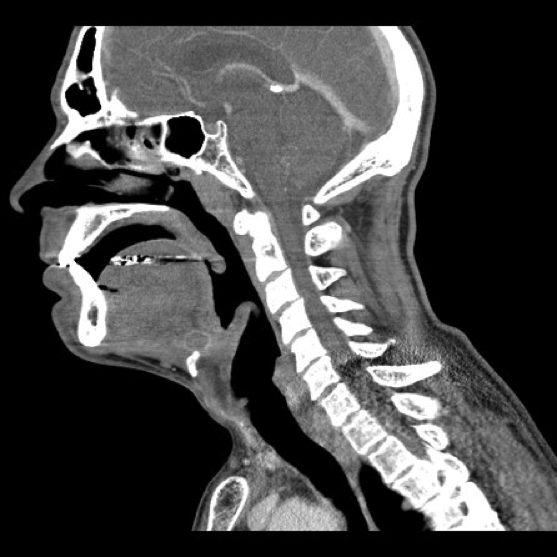

- Figure 36 and 37. Thyroglossal Duct Cyst on CT
Thyroid nodule25,27
- Multinodular Thyroid:

- Figure 38. Multinodular Thyroid with Internal Cystic Degeneration
Video 23. Multinodular Thyroid with Internal Cystic Degeneration
- Malignant Thyroid abnormalities:
- Hypoechogenicity, cystic change, irregular margins, calcifications, taller greater than wide, vascularization, extrathyroidal extension.
- Two popular scoring systems to predicting malignancy:
- The American College of Radiology Thyroid Imaging, Reporting and Data System (TI-RADS) scoring system:
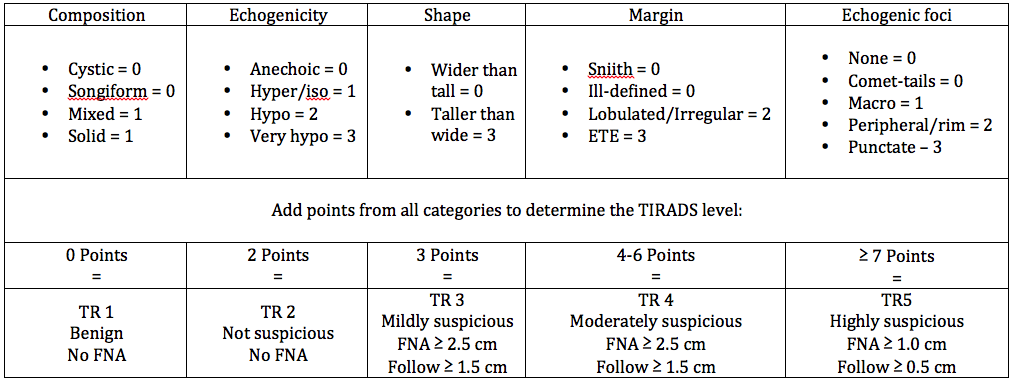
- Figure 39. TI-RADS
- American Thyroid Association (ATA) visual patterns:25
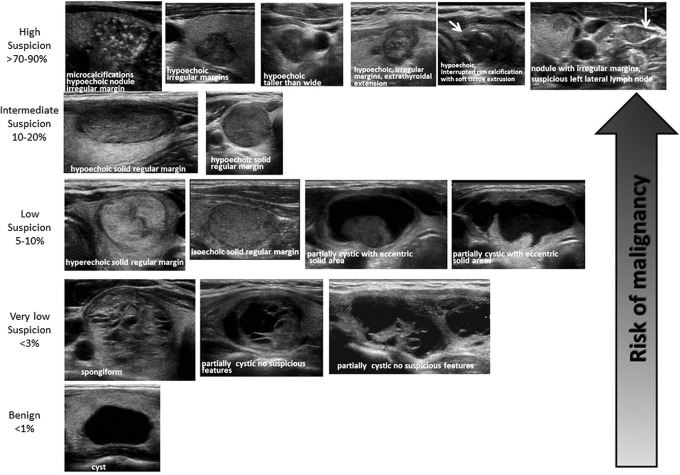
- Figure 40. ATA Nodule Sonographic Patterns and Risk of Malignancy (Used with permission. License no: 4463231228489)
- The American College of Radiology Thyroid Imaging, Reporting and Data System (TI-RADS) scoring system:
- Benign Thyroid abnormalities:
- Spongiform nodule (microcysts > 50% of nodule), halo sign, and absent vascularization
- Incidence of pathology (Thyroid nodules):28
- Prevalence = 2-6% (Palpation)
- Prevalence = 19-35% (Ultrasound)
- Prevalence = 8-65% (Autopsy data)
V. Pearls and pitfalls
- Improved visualization of neck anatomy can be achieved by placing the patient supine with neck in mild hyperextension.
- Hypo-echogenicity is defined relative to the strap muscles (Normal thyroid is hyperechoic compared to the strap muscles and similar echogenicity to other glands, like the submandibular gland).29
- Cystic and complex thyroid nodules can appear similar to an abscess.
- Referral for specialty trained sonographers and radiologist is ideal for evaluating thyroid pathology.
Tonsil
I. Introduction and Indications
- Ultrasonography is a valuable tool in the assessment and management of suspected peritonsillar abscess (PTA).
- It is noninvasive, can be rapidly performed at the bedside in the emergency department, and if an abscess is found it can be aspirated under direct ultrasound guidance.
- Peritonsillar infections include tonsillitis, cellulitis and abscess. A distinction between a peritonsillar cellulitis and peritonsillar abscess should be made, as the former is generally treated with analgesics and antibiotics while the latter may require aspiration or incision and drainage.
- Clinical differentiation of peritonsillar abscess from peritonsillar cellulitis can be difficult and the traditional management approach has been to perform a diagnostic needle aspiration of the tonsillar fossa.
- Blind needle aspiration carries serious complications such as puncturing of the carotid arteries, jugular veins, or parotid gland.
- In addition, blind needle aspiration has a reported false-negative rate of 10-24 %.30-32
II. Anatomy
- Relevant anatomy:20
- The tonsils (palatine) are bundles of lymphatic tissue located on either side of the oropharynx (between the palatoglossal muscle anteriorly and the palatopharyngeal muscle posteriorly). Laterally, the pharyngobasilar fascia forms a fibrous capsule and septations in the tonsils. Medially, the free surface of the tonsil is seen in the oropharynx with crypts.
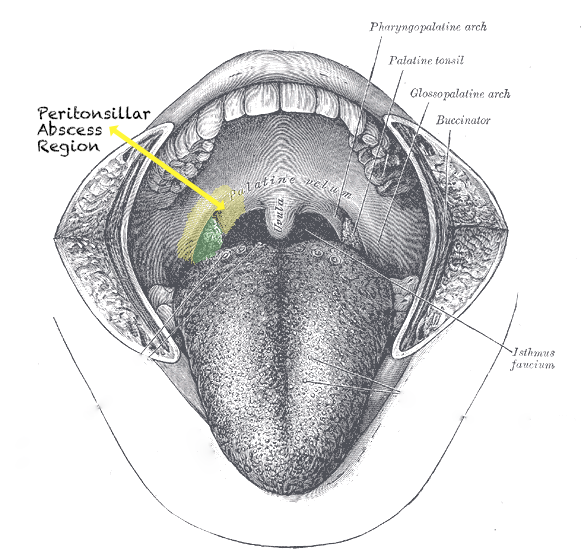
- Illustration 41. Peritonsillar abscess region (Modified from https://commons.wikimedia.org/wiki/File:Gray1201.png)
- The tonsils (palatine) are bundles of lymphatic tissue located on either side of the oropharynx (between the palatoglossal muscle anteriorly and the palatopharyngeal muscle posteriorly). Laterally, the pharyngobasilar fascia forms a fibrous capsule and septations in the tonsils. Medially, the free surface of the tonsil is seen in the oropharynx with crypts.
III. Scanning technique, normal findings and common variants
- Endocavitary probe can be used for the evaluation of tonsils.
- Any abnormality should be visualized in at least two planes, longitudinal and transverse, and comparison to the contralateral normal side is recommended.
- For anechoic structures, such as abscess, color Doppler and compression techniques can further help confirm findings.
- Adjacent structures, such as vessels, nerves and lymphatics should be visualized, particularly when planning an invasive procedure, such as a needle aspiration or incision and drainage, so one can avoid injuring these other structures.
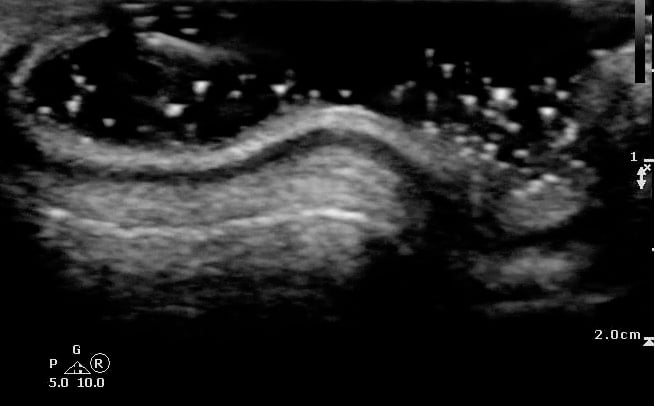
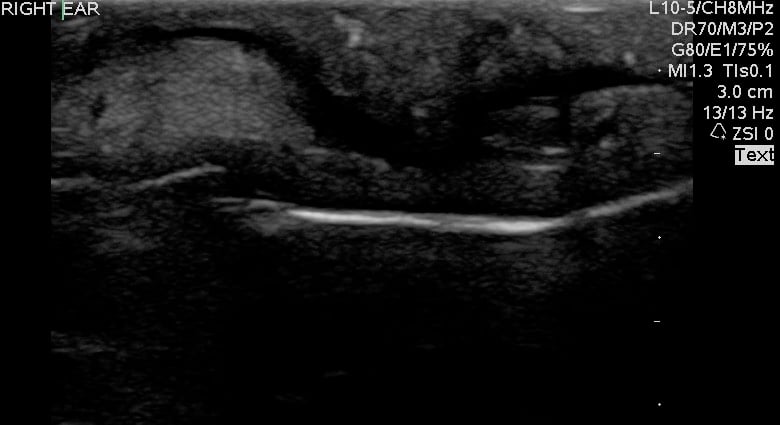
- Scanning technique20
- Probe selection:
- A 5.0 to 10.0 MHz curved array intracavitary probe is used to evaluate a suspected PTA for intraoral ultrasound. Alternatively, a high frequency linear array transducer can be used for transcervical approach, especially in children or patients with severe trismus.
- Scanning approach:
- Cover intracavitary probe with either a proprietary cover, glove or condom.
- Place probe into the oral cavity over the area in question.
- The peritonsillar area should be systematically scanned in both long and short axes.
- Color Doppler should be used to identify the depth of the carotid artery and surrounding vessels.
- Alternatively, place the linear array transducer inferior and adjacent to the angle of the mandible with rotation of the head to the contralateral side. The tonsil is deep to the submandibular gland, medial to the facial vessels, and lateral to the tongue.
Video 24. Scanning tonsils
- Probe selection:
- Normal findings
- Normal Tonsil
- The ovoid tonsils appear striated with hyperechoic bands and hypoechoic parenchyma, as well as lobulated margins.


- Figure 42 and 43. Normal Tonsil
Video 25. Normal tonsil
- The ovoid tonsils appear striated with hyperechoic bands and hypoechoic parenchyma, as well as lobulated margins.
- Tonsillolith
- Calcified accumulated debris appears as millimeter sized hyperechoic lesions within the hypoechoic tonsillar parenchyma.
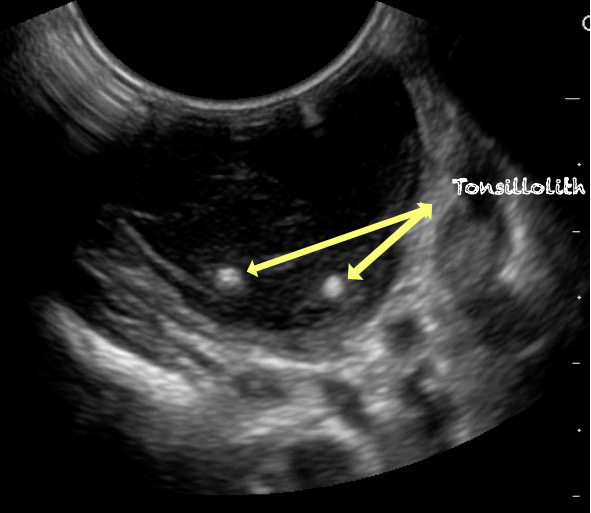
- Figure 44. Tonsillolith
Video 26. Tonsilloliths
- Calcified accumulated debris appears as millimeter sized hyperechoic lesions within the hypoechoic tonsillar parenchyma.
- Normal Tonsil
IV. Pathology
Peritonsillar abscess (PTA)33,34
- Significance of pathology:
- Complications of a PTA may include development of a parapharyngeal abscess, mediastinitis, airway obstruction, and other life-threatening pathology.
- Incidence of pathology:
- 37 per 100,000 PTA33,34
- Peritonsillar abscess is visualized as a hypoechoic or complex cystic structure
- Ultrasound-guided needle aspiration of a PTA:
- The depth of the abscess cavity from the mucosal surface should be noted to determine the length of the needle required to drain the abscess.


- Figure 45. and 46. PTA aspiration
- The depth of the abscess cavity from the mucosal surface should be noted to determine the length of the needle required to drain the abscess.
- The carotid artery is seen as an anechoic tubular structure along the posterolateral aspect of the tonsil on ultrasound. Its relationship to the abscess cavity should be determined. Color Doppler can help locate the carotid artery.
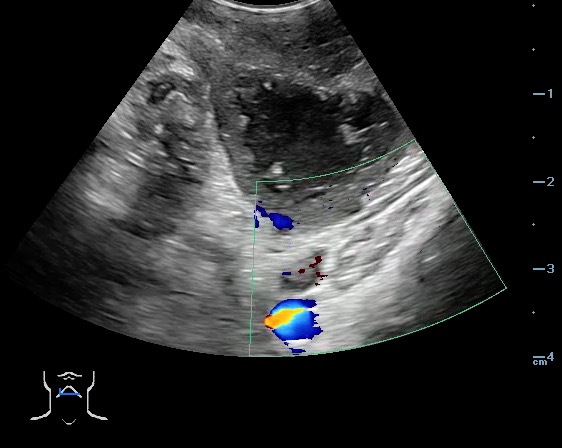
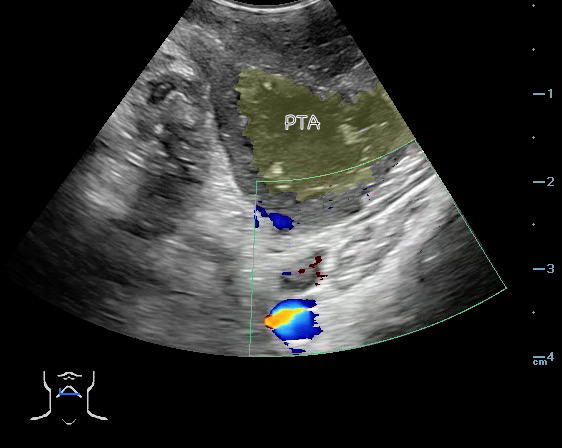
- Figure 47 and 48. PTA with color Doppler of carotid artery
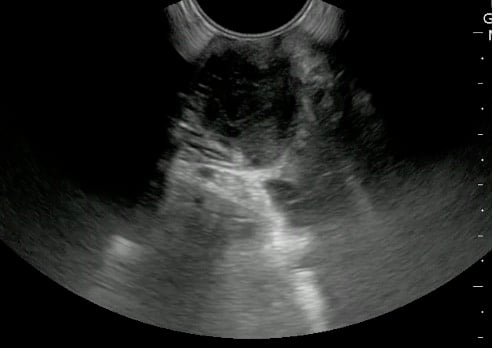
Video 27. PTA Aspiration - Complete aspiration verified by ultrasound:

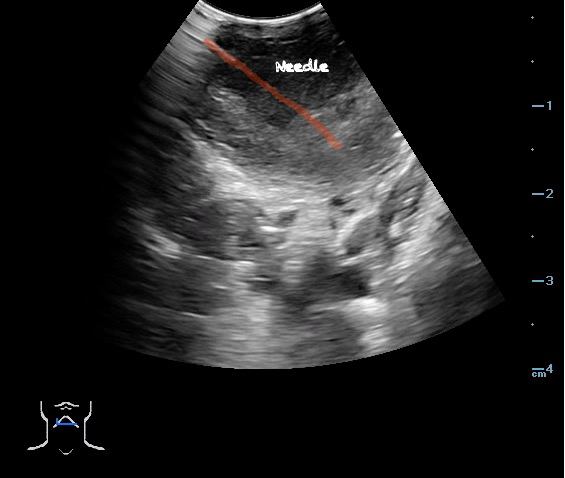
- Figure 49 and 50. PTA Aspiration Resolution
Video 28. PTA - Aspiration Resolving
Video 29. PTA Aspiration Resolution - Tonsillitis:
- Tonsillar hypertrophy with preserved homogeneous echotexture, but no fluid collection.
- Figure 51. Tonsillitis
Video 30. Tonsillitis
- Tonsillar hypertrophy with preserved homogeneous echotexture, but no fluid collection.
V. Pearls and pitfalls
- Application of a topical anesthetic spray is recommended to reduce gagging and overcome trismus. This will facilitate insertion of endocavity probe and use real time ultrasound guidance for aspiration.30-32
- If unable to perform intraoral ultrasound, consider transcervical approach.
- The ability to simultaneously image and introduce the needle allows the emergency physician to track the entire course of needle and prevent complications such as puncturing the carotid artery.30-32
- Use Color Doppler to determine the relationship of the carotid artery to the abscess cavity prior to performing aspiration.
References
- Wortsman X, Jemec GB. Sonography of the ear pinna. J Ultrasound Med. 2008;27(5):761–70.
- American Institute of Ultrasound in Medicine. AIUM Practice Parameter: Ultrasound Examinations of the Head and Neck. 2013. https://www.aium.org/resources/guidelines/headNeck.pdf
- Kaplan AL, Cook JL. The incidences of chondritis and perichondritis associated with the surgical manipulation of auricular cartilage. Dermatol Surg. 2004;30(1):58-62; discussion 62.
- Adhikari S, Blaivas M, Lander L. Comparison of bedside ultrasound and panorex radiography in the diagnosis of a dental abscess in the ED. Am J Emerg Med. 2011;29:790-5.
- Candamourty R, Venkatachalam S, Ramesh Babu MR, et al. Ludwig's Angina – An emergency: A case report with literature review. J Nat Sci Biol Med. 2012; 3(2):206-8.
- Ying M, Ahuja A, Brook F, et al. Vascularity and grey-scale sonographic features of normal cervical lymph nodes:variations with nodal size. Clin Radiol. 2001;56:416-9.
- Peleg M, Heyman Z, Ardekian L, et al. The use of ultrasonography as a diagnostic tool for superficial facial space infections. J Oral Maxillofac Surg. 1998;56(10):1129-31.
- Cui XW, Jenssen C, Saftoiu A, et al. New ultrasound techniques for lymph node evaluation. World J Gastroenterol. 2013;19(30): 4850-60.
- Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evaluation of neck metastatic adenopathy. AJR Am J Roentgenol. 2000;174(3):837-44.
- Na DG, Lim HK, Byun HS. Differential diagnosis of cervical lymphadenopathy: usefulness of color Doppler sonography. Am J Roentgenol. 1997;168(5):1311-6.
- Białek EJ, Jakubowski W. Mistakes in ultrasound diagnosis of superficial lymph nodes. J Ultrason. 2017;17(68):59-65.
- Gritzmann N. Sonography of the salivary glands. AJR Am J Roentgenol. 1989;153(1):161-6.
- Bialek EJ, et al. US of the major salivary glands: anatomy and spatial relationships, pathologic conditions, and pitfalls. Radiographics. 2006;26(3):745-63.
- Jäger L, Menauer F, Holzknecht N, et al. Sialolithiasis: MR sialography of the submandibular duct--an alternative to conventional sialography and US? Radiology. 2000;216(3):665-71.
- Marchal F, Dulguerov P. Sialolithiasis Management: The State of the Art. Arch Otolaryngol Head Neck Surg. 2003;129(9):951-6.
- Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137(3 Suppl): S1-31.
- Laine K, Määttä T, Varonen H, et al. Diagnosing acute maxillary sinusitis in primary care: a comparison of ultrasound, clinical examination and radiography. Rhinology. 1998;36(1):2-6.
- Varonen H, Mäkelä M, Savolainen S, et al. Comparison of ultrasound, radiography, and clinical examination in the diagnosis of acute maxillary sinusitis: a systematic review. J Clin Epidemiol. 2000;53(9):940-8.
- Price D, Park R, Frazee B, et al. Emergency department ultrasound for the diagnosis of maxillary sinus fluid. Acad Emerg Med. 2006;13(3):363-4.
- Cosby, Karen S. and John L. Kendall. Practical Guide to Emergency Ultrasound. Srikar Adhikari. Chapter 24: Infections of the Head and Neck. Wolters and Kluwer. August 13, 2013.
- Lichtenstein D, Biderman P, Mezière G, et al. The “sinusogram,” a real-time ultrasound sign of maxillary sinusitis. Intensive Care Med. 1998;24(10):1057-61.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): Adult Sinusitis Executive Summary. Otolaryngol Head Neck Surg. 2015;152(4):598-609.
- Piccirillo JF, Mager DE, Frisse ME, et al. Impact of first-line vs second-line antibiotics for the treatment of acute uncomplicated sinusitis. JAMA. 2001;286(15):1849-56.
- Zander DA, Smoker WRK. Imaging of Ectopic Thyroid Tissue and Thyroglossal Duct Cysts. Radiographics. 2014;34(1):37-50.
- Haugen BR, Alexander EK, Bible KC, et. al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
- Etzkorn, James and Maria Cristina Chammas. Ultrasound of the Thyroid: Guidelines and Controversies in the Management of Incidental Thyroid Nodules. AIUM Video Lecture. http://s3.amazonaws.com/aium/CommLectures/141.mp4
- Sipos JA. Advances in ultrasound for the diagnosis and management of thyroid cancer. Thyroid. 2009;19(12):1363-72.
- Dean DS, Gharib H. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008;22(6):901-11.
- Kim EK, Park CS, Chung WY, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002;178(3):687-91.
- Blaivas M, Theodoro D, Duggal S. Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. Am J Emerg Med. 2003;21(2):155-8.
- Lyon M, Blaivas M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad Emerg Med. 2005;12(1):85-8.
- Dewitz A. Soft tissue applications. In: Ma OJ, Mateer J, eds. Emergency ultrasound. New York: McGraw-Hill, 2003:385.
- Herzon FS. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope. 1995;105(8 Pt 3 Suppl 74):1-17.
- Risberg S. Incidence of peritonsillar abscess and relationship to age and gender: retrospective study. Scand J Infect Dis. 2008;40(10):792-6.