EMS Pre-Hospital Ultrasound
Mark Robidoux MD; Kolby Kolbet MSN; John L. Hick MD, FACEP; William G. Heegaard, MD, MPH, FACEP; Barrett Wagner, MD; Rob Reardon, MD
Background
- EMS is increasingly using sophisticated technologies for patient assessment, particularly during ground and aeromedical (rotor and fixed wing) critical care transport.
- Goal-directed, limited window ultrasounds can provide critical information to guide pre-hospital interventions, guide procedures, and support destination/triage decision-making.
- New tablet-based and other portable ultrasound machines provide a platform useful in the transport environment.
- Ultrasound can be particularly useful in the rotor-wing environment where ambient noise makes auscultation impossible.
- According to a survey published in 2014 about 4% of responding EMS agencies in North America were using ultrasound and 21.7% were considering using it – a majority of those services already using US involved physician operators.1
- Prehospital ultrasound is more prevalent in EMS systems that routinely utilize physician providers. (e.g., Australia, Europe, Canada)
- Prehospital physicians and paramedics have been shown to accurately perform components of the FAST exam with good accuracy.2,3
- Flight paramedics and flight nurses have also correctly identified lung sliding with comparable accuracy to in-hospital emergency physicians.4
- EMT/Paramedics can accurately perform FAST both in-hospital and out of hospital patients.5,6
- Paramedics have been trained to correct identify standstill in cardiac arrest patients.7
Applications
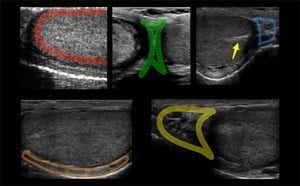
Primary
- FAST exam to detect free intra-abdominal fluid in trauma and medical conditions
- Cardiac ultrasound exam in hypotensive or cardiac arrest patients to place them in one of five states: Cardiac standstill, severe hypovolemia, cardiogenic shock, pericardial tamponade or right ventricular obstruction.
- Fetal monitoring and evaluation in obstetric patients
- Sliding lung signs for detection of pneumothorax
Secondary
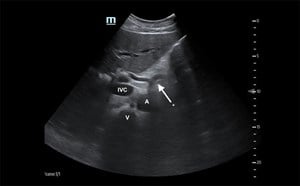
- Inferior vena cava assessment to guide resuscitation
- Thoracic exam for hemothorax or B-lines (pulmonary edema)
- Vascular access – potentially including central lines and arterial catheters
- Optic nerve sheath assessment for increased intracranial pressure
- Left ventricular function global assessment (good/poor ejection fraction)
- Abdominal Aortic Aneurysm - In patients with suspect rupture/hypotension
- Mass Casualty Triage - provides rapid diagnostic information, can better identify patient at risk for decompensation.8 US can also be utilized during a hospital mass casualty incident when other imaging sources (X-ray, CT) become overwhelmed.9
Impact on Care Provided
- Improved, actionable information provided to receiving facility
- Potential change in destination hospital
- Distinguish between cardiac standstill and severe volume deficit or severely impaired LV function (pseudo-PEA)
- Prompt interventions and confirm efficacy – eg, chest decompression, pericardiocentesis, vascular access, blood administration/fluid resuscitation10
- Accomplish procedures safely – pericardiocentesis, vascular access
- Rule out conditions and avoid ‘blind’ or unnecessary interventions11
- Dutch study (Ketelaars) – of 1495 abdominal studies, 12.6% impacted care, lower than intervention rate found in smaller Walcher (30%) and O’Dochartaigh (26% for EMT-P/RN, 45% for MDs) studies that looked at both abdominal and chest pre-hospital ultrasound12-14
- Review demonstrates pre-hospital ultrasound likely influences destination and interventions but unclear effect in current studies on outcomes15
- Brun demonstrated prehospital physicians performing eFAST exams with sensitivity/specificity in the 90th percentile on seen, but improved to near 100% when repeated during transport.3 This supports the value of serial exams on critically ill patients.
Training
- Studies have demonstrated successful acquisition and interpretation of images after a few hours of training.
- 20 firefighter-paramedics exhibited competence with image acquisition and interpretation for pneumothorax, cardiac activity, and pericardial effusion after 2 hours of training15
- Paramedics completing 6 hours of training completed 84 abdominal FAST exams with 100% concordance with physician image over-read6
- Ongoing assessments and competencies are necessary to assure skill maintenance
- Personnel tend to group into high, middle, and lower utilizers – additional training is often required for low utilizers to assure comfort and competence
- On-line interpretation testing using multiple clips of normal and abnormal can be a key component of training
- Training should be simple – single or few windows (eg, Morison’s pouch, anterior chest, subxiphoid and parasternal long cardiac views, and suprapubic fetal windows) and binary interpretations (present/absent)
- Training curricula – as an example, LifeLink III (Minnesota/Wisconsin) provides the following – for most clinicians this results in about 6 hours of training:
- 1 hour orientation to ultrasound imaging
- 2 hours of image acquisition training (hands-on)
- On-line imaging interpretation tests
- Competencies checked by base leads
- Incorporation of imaging into simulation cases
- Additional lectures by ultrasound fellows – live and online - optional
Quality Improvement
- Audits of ultrasound should include:
- Number of studies and indications by employee to determine use patterns
- Interpretation review – accurate interpretation? (inaccurate interpretation should lead to feedback with coaching and re-education as required)
- Number of cases in which US findings prompted an intervention or clinical decision
- Number of cases in which US finding prompted a change in destination
- Competency checks of personnel should occur on a regular basis
- Images and interpretation should be available for review/over-read by expert staff (LifeLink III uploads images and provider interpretations to a cloud-based system for review by ultrasound fellows and faculty at Hennepin County Medical Center) – real-time review should not be necessary for simple, goal directed ultrasound windows.
Experience and Limitations
Ground
- Current relatively high cost of units and need for training is problematic for larger services – benefits may be greater for smaller services with longer transport times – this is an area for future study.
Aeromedical
- Many rotor-wing services are providing or considering ultrasound
- Few services provide image storage and review, limiting quality improvement opportunities. Cloud-based and other systems are beginning to offer options for auditing.
- Patient access may limit windows obtainable during transport
Summary
- Ultrasound technology allows for high quality ultrasound imaging to occur in the pre-hospital settings. Studies can be rapidly performed.
- The use of ultrasound in the pre-hospital setting has the potential to improve trauma, cardiac and obstetric care.
- Several research projects on rotor-wing ultrasound and ground EMS ultrasound are ongoing in the USA and Europe.
- Larger well-designed multicenter pre-hospital ultrasound studies are needed to reduce bias and assess impact on care.
Video 1. Positive Morison’s pouch – prompted early blood and tranexamic acid administration
Video 2. Absent sliding signs – not resolved after needle thoracostomy
Video 3. Sliding lung signs after finger thoracostomy performed
References
- Taylor J, McLaughlin K, McRae A, et al. Use of prehospital ultrasound in North America: a survey of emergency medical services medical directors. BMC Emerg Med. 2014;14:6.
- Walcher F, Weinlich M, Conrad G, et al. Prehospital ultrasound imaging improves management of abdominal trauma. Br J Surg. 2006;93:238-42.
- Brun PM, Bessereau J, Chenaitia H, et al. Stay and play eFAST or scoop and run eFAST? That is the question! Am J Emerg Med. 2014;32:166-70.
- Quick JA, Uhlich RM, Ahmad S, et al. In-flight Ultrasound Identification of Pneumothorax. Emerg Radiol. 2016;23:3-7.
- Kim CH, Shin SD, Jun Song K, et al. Diagnostic Accuracy of Focused Assessment with Sonography for Trauma (FAST) Examinations Performed by Emergency Medical Technicians. Prehosp Emerg Care. 2012;16(3):400-6.
- Heegaard W, Hildebrandt D, Spear D, et al. Prehospital ultrasound by paramedics: results of field trial. Acad Emerg Med. 2010;17(6):624-30.
- Rooney KP, Lahham S, Lahha S, et al. Pre-hospital assessment with ultrasound in emergencies: implementation in the field. World J Emerg Med. 2016;7(2):117-23.
- Wydo SM, Seamon MJ, Melanson SW, et al. Portable ultrasound in disaster triage: a focused review. Eur J Trauma Emerg Surg. 2016;42:151-9.
- Eyre AJ, Stone MB, Kimberly HH. Point-of-care ultrasonography in a domestic mass casualty incident: The Boston marathon experience. Emerg Med Open J. 2016;2(2):32-5.
- Ketelaars R, Beekers C, Van Geffen GJ, et al. Prehospital Echocardiography During Resuscitation Impacts Treatment in a Physician-Staffed Helicopter Emergency Medical Service: an Observational Study, Prehospital Emergency Care, 2018 DOI: 10.1080/10903127.2017.1416208 (accessed April 12, 2018)
- Ketelaars R, Holtslag JM, Hoogerwerf N. Abdominal prehospital ultrasound impacts treatment decisions in a Dutch Helicopter Emergency Medical Service. European J Emerg Med. 2018.
- Ketelaars R, Hoogerwerf N, Scheffer Prehospital chest ultrasound by a Dutch helicopter emergency medical service. J. Emerg. Med. 2013;44(4):811-7.
- O’Dochartaigh D, Douma M, MacKenzie M. Five-year retrospective review of physician and non-physician performed ultrasound in a Canadian Critical Care Helicopter Emergency Medical Service. Prehosp Emerg Care. 2017;21:24-31.
- O’Dochartaigh D, Douma M. Prehospital ultrasound of the abdomen and thorax changes trauma patient management: a systematic review. Injury. 2015;46:2093-102.
- Chin EJ, Chan CH, Mortazavi R, et al. A pilot study examining the viability of a prehospital assessment with ultrasound for emergencies (PAUSE) protocol. J Emerg Med. 2013;44(1):142-9.