
Carbon Monoxide Poisoning: Mixed-Acid Cocktail Suicide Attempt
Introduction
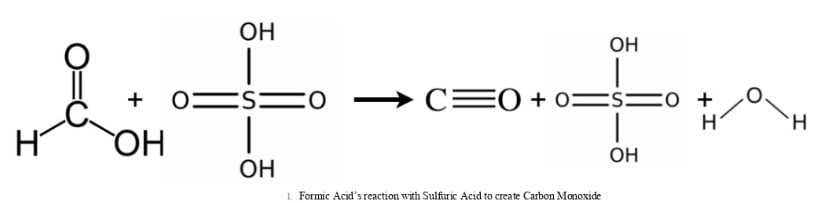
Acute carbon monoxide (CO) poisoning is a leading cause of toxicological death. Typically, CO is formed by the incomplete combustion of carbonaceous materials; the most common mechanism exploited for suicide attempts. This is an extremely rare case of suicide attempt by intentionally combining formic and sulfuric acids to generate CO. Previous case reports reflect this cocktail’s near universal fatality due to inhalation with carboxyhemoglobin (COHb) levels ranging from 64-93% and caustic injury.
Case
A 27-year-old female medical student was found unresponsive in her car by family members at 10:30 AM. She was last seen by her sister less than 12 hours earlier, journaling in her room. It was later discovered that she was, in fact, writing her suicide note. Per EMS report, she was found unresponsive in the backseat of the car with the engine not running. Next to her face lay the end of a tube running from a 5-gallon drum containing a green “oily” fluid. On scene, first responders discovered marked containers of formic and sulfuric acid. They ventilated the car for scene safety and, despite standard HAZMAT procedures, reported residual CO levels of 150-200ppm. Patient’s initial evaluation revealed a GCS 8 (E2V2M4). Upon arriving to the closest hospital ED, initial COHb was 17%. She was intubated for airway protection. Based on the severity of the exposure and her presentation, she was transferred to the University of Pennsylvania for hyperbaric oxygen therapy (HBOT). Our initial evaluation was significant for an intubated age appropriate female with decerebrate posturing.
Discussion
In our case detailed above, the patient was treated with a time-course consistent with Weaver’s 2002 study design. Given the severity of the presenting symptoms and the workup findings, she was treated immediately upon arrival with a 2.8 ata treatment table (USN TT5). This decision was made, in the setting of presumed anoxic brain injury and risk of pharmaceutically lowered seizure threshold, to provide the air-breaks built into the USN TT5 at the maximal depth to mitigate risk of oxygen-induced toxicity. Within 24 hours, she received two additional treatments with identical profiles (2.0 ata for 90 minutes). She had appreciable interval improvement between her second and third treatment. She had been extubated in the MICU and was oriented to person/place/time with appropriate following of commands. Despite the grim initial presentation and the implications of posturing on exam, she was now moving all extremities with purpose where she had been hemiplegic hours before. A minor residual complaint that patient described was a bilateral buttock pain. This was corroborated with an elevated LFT panel and CK level consistent with Rhabdomyolysis. The etiology likely being tied to her acute CO poisoning, dependent positioning for an unknown period of time, and other toxin-mediated injury. Her Troponin T that had been elevated, presumably from acute hypoxic injury, continued to trend lower. Following her completion of the three dives, she remained inpatient for further neuropsychiatric rehabilitation.
When contacted for six-week follow-up, she was back home, exercising and playing sports without any residual physical limitation or impairment. She had no otic symptoms, despite emergent prophylactic myringotomies. When discussing the litany of possible residual neurologic symptoms, she only endorsed focally limited short-term memory. This short term seemed to be most significantly centered around the poisoning event. She added that, as noticed by herself and family, her recollection is improving both in terms of broad recall and specificity. Subjectively, she reports no cognitive slowing in returning to her previous high level of mental function. Given the severity of the exposure and her clinical course, it was recommended she follow up with cognitive neurology, cardiology, psychiatry, and her primary care physician, as appropriate. When seen by Penn Neurology at five months post-exposure, she reported improvement in her short-term memory impairment, with no recrudescence of symptoms. No further neurologic testing or follow-up was recommended.
Zack Gaskill DO
Department of Undersea and Hyperbaric Medicine
University of Pennsylvania, Philadelphia, PA



