Renal
Barbara K. Blok, MD, FACEP
I. Introduction and Indications
- Point-of-care (POC) renal ultrasound (US) is a rapid, bedside test for the evaluation of the patient with suspected renal colic or urinary retention.
- Because ureteral stones can be difficult to visualize by US,1 the secondary finding of hydronephrosis is used to diagnose nephrolithiasis when the clinical suspicion for renal colic is high.
- POC renal US for the diagnosis of nephrolithiasis has a reported sensitivity and specificity of 70% and 75%, respectively using the gold standard of CT examination2 and can decrease cumulative radiation exposure.3
- POC US should be used as part of a treatment pathway to safely diagnose and disposition patients with uncomplicated renal colic. Studies demonstrate that patients with mild hydronephrosis on POC US are less likely to have large ureteral calculi or require urologic intervention4-6 and those with moderate to severe hydronephrosis are likely to have stones >5mm in size.6,7
- POC US can also be used to estimate bladder volume for the diagnose of urinary retention.8-11
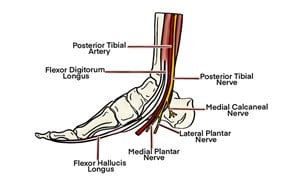
II. Anatomy
- The kidneys are retroperitoneal organs that are protected by the lower ribs posteriorly. The right kidney lies just below the liver, while the left lies just below the spleen. The superior pole of each kidney is tilted slightly medially and posteriorly (oblique lie).
- Grossly, each kidney consists of (from periphery inward):
- Fibrous capsule that supports and protects kidney
- Outer cortex
- Inner medulla containing 6-8 renal pyramids and surrounding columns of cortical tissue.
- Renal sinus, a central cavity on the medial aspect of each kidney which primarily houses the calyces and renal pelvis which collect urine produced in the renal pyramids, but also contains renal sinus fat, branching blood vessels, lymphatics and nerves.
- Renal hilum, which is the entrance/exit for the renal pelvis, blood vessels, lymphatics, and nerves.
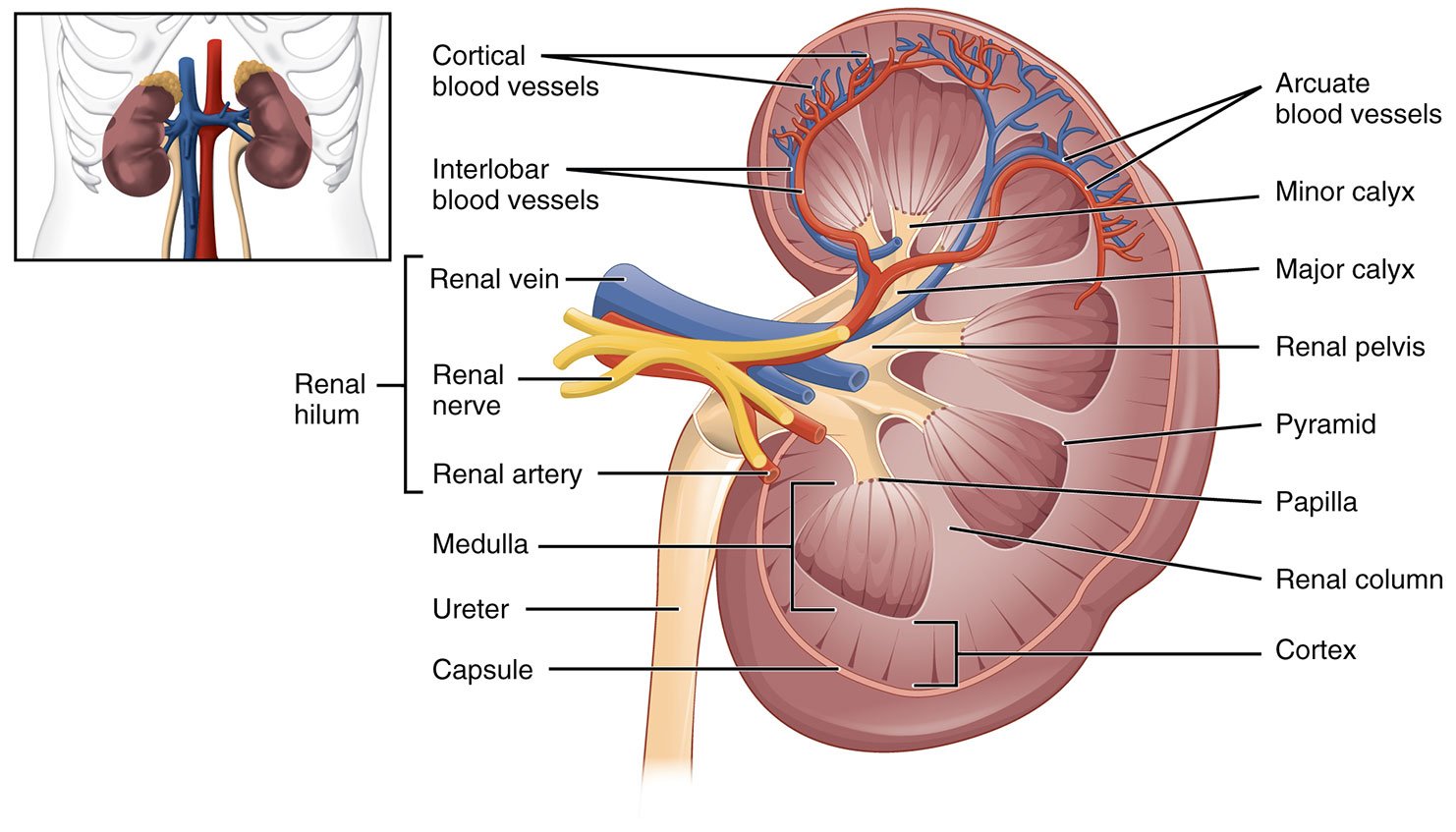
- Illustration 1. Normal renal anatomy (Source: https://commons.wikimedia.org/wiki/File:2610_The_Kidney.jpg)
- The whole renal complex is surrounded by a fascial layer, called Gerota’s fascia.
- The ureter is a tubular, muscular structure that originates from the renal pelvis and travels retroperitoneal and anterior to the psoas muscle towards the bladder. It courses medially then crosses over the iliac vessels and travels along the pelvic sidewalls before turning anteriorly and medially to enter the fundus of the bladder.
- There are three natural anatomic narrowings of the ureters:
- The ureteropelvic junction, as the renal pelvis narrows to become the ureter
- The crossing of the iliac vessels, due to external bending and compression
- The ureteral vesicular junction, due to intrinsic narrowing
- The muscular bladder lies just posterior to the pubis and anterior to the rectum (males) or uterus (females).
III. Scanning Technique, Normal Findings and Common Variants
Sonographic Technique for Kidney and Ureter
- A 2- to 5-MHz curvilinear probe is used to scan the kidney and bladder.
- For the right kidney, have the patient lie supine and place the probe in the right lower intercostal space in the midaxillary line.
- Use the liver as your sonographic “window” and aim the probe slightly posteriorly to visualize the kidney.
- Gently rock the probe (up and down or side to side) to scan the entire kidney. If needed, you can have the patient inspire, which allows for subtle movement of the kidney inferiorly.
- Obtain longitudinal (long axis) and transverse (short axis) views. On longitudinal view the kidney will appear football-shaped and on transverse view the kidney appears C-shaped.
Video 1. Longitudinal view of normal right kidney
Video 2. Longitudinal view of normal right kidney
Video 3. Longitudinal view of normal right kidney
Video 4. Transverse view of normal right kidney
- For the left kidney, have the patient lie supine or in the right lateral decubitus position. Place the probe in the lower intercostal space on the posterior axillary line. The placement will be more cephalad and posterior than when visualizing the right kidney.
- Gently rock the probe to scan the entire kidney.
- Obtain longitudinal and transverse views.
- Always scan both kidneys for comparison.
Video 5. Longitudinal view of normal left kidney
Video 6. Longitudinal view of normal left kidney
Video 7. Transverse view of normal left kidney
Normal Findings and Common Variants for Kidney and Ureter
- The normal kidney will have the following characteristics:
- Bright outer covering which is made up of Gerota’s fascia and perinephric fat.
- Grainy gray periphery which is made up of the renal cortex and pyramids. Sometimes you can see the individual pyramids, but this is not always the case.
- Central bright (echogenic) area which is the renal sinus containing the calyces, renal pelvis and renal sinus fat, plus branching vessels, lymphatics and nerves.
- Length of 9-12 cm and width of 4-5 cm in the normal adult. The left kidney is often slightly larger than the right, but both should be within 2 cm of each other.
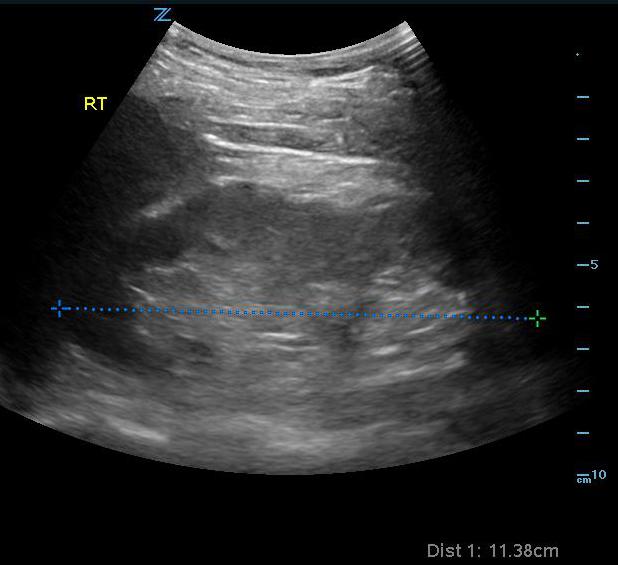
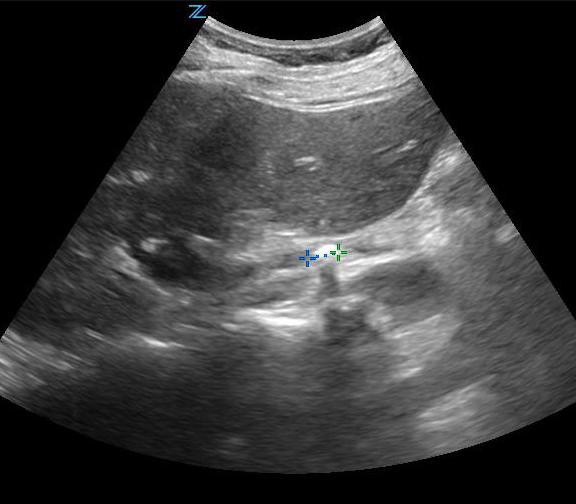
- Figure 1. Measurement of normal right kidney in longitudinal view
- There are many normal variations in the anatomic structure of the kidneys. Some common ones that you may identify include:
- Extrarenal pelvis, where the renal pelvis is lying outside of the renal hilum instead of within the renal sinus. This is found in approximately 10% of the population.
- Duplicate collecting system, where there are 2 separated collecting systems within one kidney, resulting in 2 ureters. Incidence is 1-2% of the population.
- Video 8. Duplicate collecting system
- Horseshoe kidney, where the left and right kidney are connected to each other, usually at the lower aspect. Incidence is approximately 1 in 400-500 people.
- Renal ectopia, where one or both kidneys are outside the normal renal fossa. Incidence is approximately 1 in 900 people.
- The ureters are generally not well visualized by US, but, when distended may appear as a tubular structure extending inferiorly from the kidney
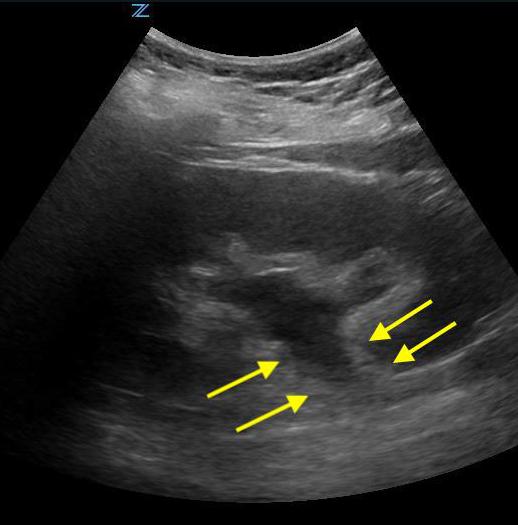
- Figure 2. Moderate hydronephrosis demonstrating location of ureter (surrounded by arrows) exiting renal pelvis
Sonographic Technique for Bladder
- For the bladder have the patient lie supine. Place the probe in the midline above the symphysis pubic with the marker directed towards the patient’s head.
- Gently rock the probe side to side to scan the entire bladder
- Obtain sagittal and transverse views
Video 9. Sagittal view of bladder in female patient with uterus seen deep to bladder
Video 10. Transverse view of bladder in female patient
- For measuring bladder volume, use the US volume measurement feature or the formula 0.52 × Depth × Width × Height.
- In the transverse view, find the largest bladder size and measure both the vertical and horizontal length of the bladder image from inner wall to inner wall. This corresponds to the bladder depth and width, respectively.
- In the sagittal plane, measure the maximum horizontal length of the bladder image from inner wall to inner wall. This corresponds to the bladder height.
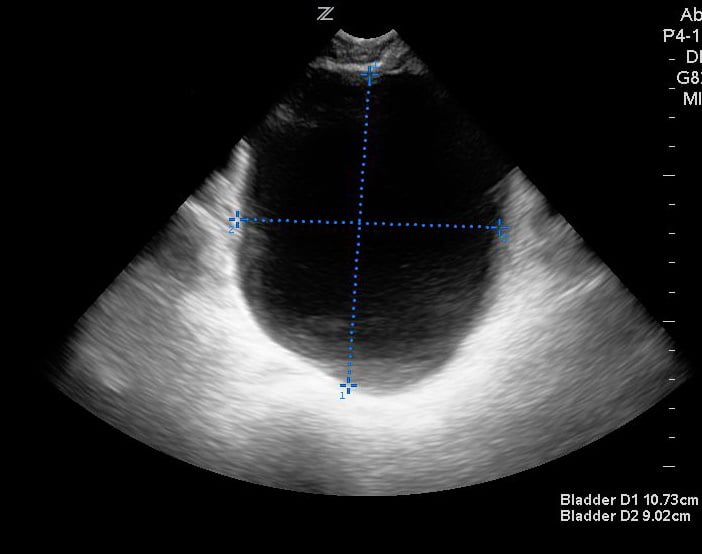
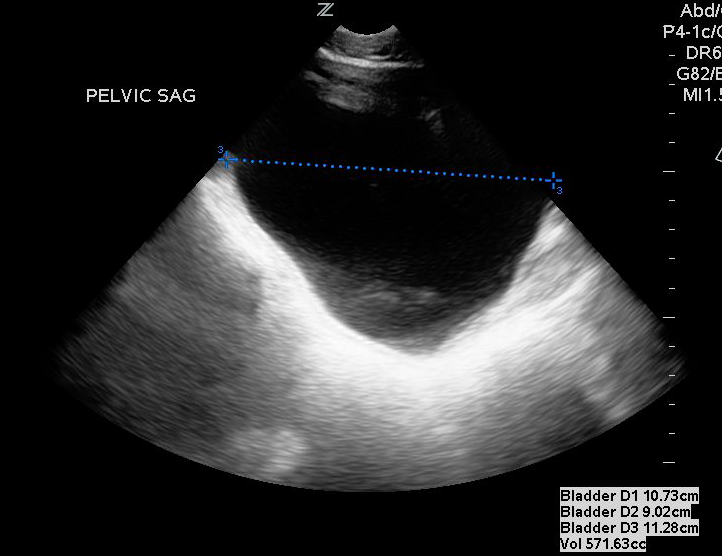
- Figures 3 and 4. Measurement of bladder volume in the transverse (Figure 3) and sagittal (Figure 4) views
Normal Findings for Bladder
- The normal bladder has a thick, smooth, muscular wall measuring 3-5 mm. When filled, the wall thickness decreases to 2-3 mm and the shape conforms to the contour of the pelvic structures.
- Normal post void bladder volume in adults is <50 in younger patients and < 100 mL in those over 65 years old.
IV. Pathology
Kidney and Ureter
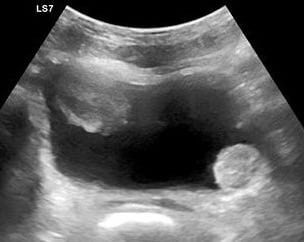
- The primary sonographic abnormality you will identify in the patient with suspected renal colic is hydronephrosis. The degree of hydronephrosis relates to the degree and extent of obstruction: (Illustration 2, Videos 11-17)
- After complete obstruction to flow, there is an acute rise in intrarenal pressure. The renal pelvis and calyces dilate first. On US you will see echo-free areas distending the normal bright (echogenic) central area of the kidney.
- As obstruction continues, the renal parenchyma becomes compressed and you see thinning of the pyramids.
- Always scan both kidneys for comparison and correlation to the patient’s clinical presentation
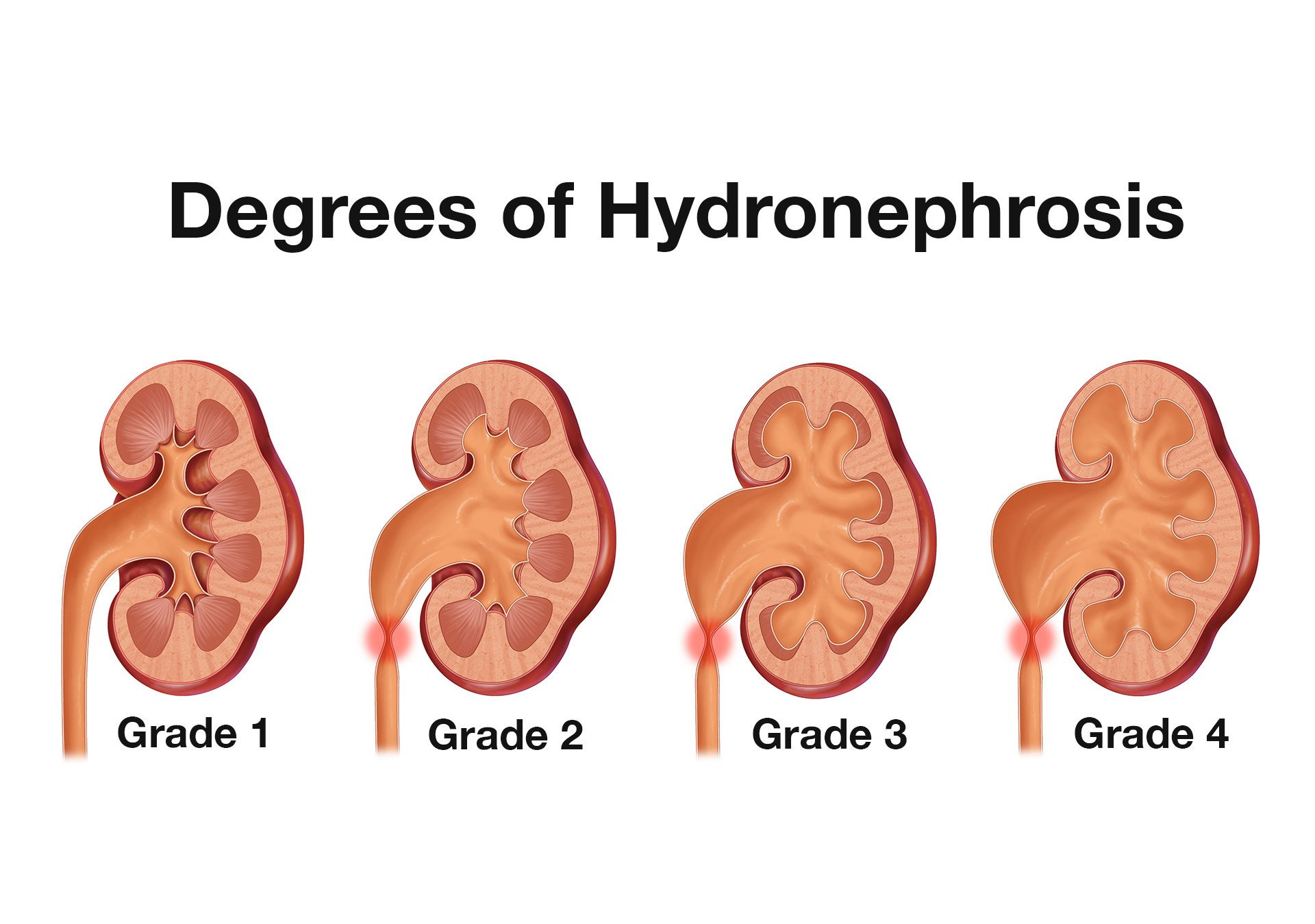
- Illustration 2. Overview of degrees of hydronephrosis
Videos 11-13. Mild hydronephrosis
- Videos 14-15. Moderate hydronephrosis
Video 16. Moderate to severe hydronephrosis
Video 17. Severe hydronephrosis
- Depending on their location, you may also identify kidney stones:
- Stones within the kidney - look for bright objects that cast a shadow within the kidney.
Video 18. Renal stone (arrow) and mild hydronephrosis 

- Figures 5 and 6. Renal stones (arrows) with shadowing
- Stones at the ureteropelvic junction - look for a bright object that casts a shadow at the hilum as the renal pelvis narrows to form the ureter.
- Stones more distal in the ureter are often hard to identify.1 If you can, follow the dilated ureter down toward the bladder. A bright object that casts a shadow within the ureter or at the junction of the bladder is consistent with ureteral stone.
- Figure 7. Stone in the mid-ureter in setting of hydroureter (Courtesy of Dasia Esener, MD)
- Stones at the ureterovesicular junction (UVJ) can be challenging to see but are sometimes evident as a protrusion of the ureter on inspection of the bladder.
Video 19. Stone at UVJ seen at bottom of the transverse bladder view to the right of midline (Courtesy of Dasia Esener, MD)
Video 20. Stone at UVJ (arrow) seen on sagittal bladder view (Courtesy of Eric Abrams, MD)
- Stones within the kidney - look for bright objects that cast a shadow within the kidney.
- Other abnormal findings that you may identify when scanning the kidney and ureter include:
- Simple or complex renal cysts- peripheral, smooth, hypoechoic and with or without internal echoes
Video 21. Renal cyst
Video 22. Kidney with several simple cysts
Video 23. Kidney with several simple cysts - Innumerable cysts seen in polycystic kidney disease with destruction of the renal cortex often seen and the kidney appears very distorted
Videos 24 and 25. Polycystic kidney disease
- Bilateral hydronephrosis indicating either mass lesion compressing both ureters or bladder outlet obstruction
- Renal mass - may have any echotexture (hyperechoic, anechoic etc.) and appear anywhere within the kidney
Video 26. Renal sarcoma (Courtesy of Dasia Esener, MD)
Videos 27 and 28. Renal cell carcinoma blurring the upper border between the kidney and liver (Courtesy of Eric Abrams, MD) - Chronic kidney disease - kidneys appear small and hyperechoic.
- Pyelonephritis - sonographic appearance is most commonly normal, but you may find hypoechoic cortex and loss of demarcation between the outer cortex and middle pyramids and columns.
- Transplant kidney - a normal echotexture kidney when healthy, typically in a pelvic location.
- Ureteral stents: have a characteristic appearance but can be difficult to visualize due to size and position but can often be seen in the bladder where they coil
Video 29. Stent seen coiling in bladder (Courtesy of Dasia Esener, MD)
- Simple or complex renal cysts- peripheral, smooth, hypoechoic and with or without internal echoes
Bladder
- Bladder outlet obstruction is confirmed by US showing a post-void bladder volume of ≥ 100 mL.
- Bladder US can be used to identify a Foley catheter balloon in the bladder
Videos 30 and 31. Foley catheter in bladder - Bladder US may identify other pathology:
- Bladder mass hyperechoic or mixed, irregular shaped mass within the bladder
- Video 32 and Figure 8. Bladder mass
- Intraluminal bladder hematoma – mobile hyperechoic collection within bladder in a patient with trauma or hematuria
Video 33. Bladder with clots - Bladder stone – bright object within the bladder that casts a posterior shadow
Video 34. Stones in bladder
- Bladder mass hyperechoic or mixed, irregular shaped mass within the bladder
V. Pearls and Pitfalls
- The primary disadvantages of POC renal US are:
- It may miss mild or early hydronephrosis
- It often does not allow determination of stone size or location within the ureter
- It does not identify other intraabdominal pathology such as appendicitis, diverticulitis, etc.
- The overhydrated patient, pregnant patient, or one with a full bladder may have mild hydronephrosis. In this case, both kidneys will show evidence of hydronephrosis.
- The underhydrated patient may not have hydronephrosis on initial renal scanning, despite the presence of obstruction and renal colic.
- In some cases, an adjacent structure such as a fluid-filled gallbladder may be mistaken as renal cyst or other renal pathology.
- US findings that can be mistaken for hydronephrosis:
- Renal cysts can sometimes be mistaken for hydronephrosis. Cysts are typically single and arise in the periphery of the kidney but can be multiple as in polycystic kidney disease.
- An extrarenal pelvis can mimic early hydronephrosis but is a normal developmental variant (12).
- Color doppler may be placed on the kidney to differentiate blood vessels in the renal pelvis giving this appearance of mild hydronephrosis.
Video 35. Color doppler reveals blood vessels entering the renal pelvis - Last, but not least, be sure to scan the aorta for AAA in the patient who clinically appears to have acute renal colic, but in whom the renal scanning is normal.
VI. References
- Nicolau C, Claudon M, Derchi LE, et al. Imaging patients with renal colic-consider ultrasound first. Insights Imaging. 2015;6(4):441-7.
- Wong C, Teitge B, Ross M, et al. The accuracy and prognostic value of point-of-care ultrasound for nephrolithiasis in the emergency department: A systematic review and meta-analysis. Acad Emerg Med. 2018; 25(6):684-98.
- Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014;371(12):1100-10.
- Daniels B, Gross CP, Molinaro A, et al. STONE PLUS: Evaluation of emergency department patients with suspected renal colic, using a clinical prediction tool combined with point-of-care limited ultrasonography. Ann Emerg Med. 2016;67(4):439-48.
- Edmonds ML, Yan JW, Sedran RJ, et al. The role of renal ultrasonography in the diagnosis of renal colic in emergency department patients. 2010;12:201-6.
- Goertz JK, Lotterman S. Can the degree of hydronephrosis on ultrasound predict kidney stone size? Am J Emerg Med. 2010;28(7):813-6.
- Moak JH, Lyons MS, Lindsell CJ. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. Am J Emerg Med. 2012;30(1):218-21.
- Chan H. Noninvasive bladder volume measurement. J Neuroscience Nurs. 1993;25(5):309-12.
- D'Silva KA, Dahm P, Wong, CL. Does this man with lower urinary tract symptoms have bladder outlet obstruction? The Rational Clinical Examination: a systematic review. 2014;312(5):535-42.
- Hakenberg OW, Ryall RL, Langlois SL, et al. The estimation of bladder volume by sonocytography. J Urol. 1983;130(2):249-51.
- Hvarness, H, Skjoldbye B, Jakobsen H. Urinary bladder volume measurements: comparison of three ultrasound calculation methods. Scand J Urol Nephrol. 2002;36(3):177-81.
- Koratala A, Bhattacharya. Extrarenal pelvis mimicking hydronephrosis: a case for caution. Clin Case Rep. 2017;5(10):1720-1.