General Nerve Block Contraindications and Precautions
- Allergy to local anesthetic agents
- Active infection at injection site
- Risk of compartment syndrome or need to monitor neurologic function
- Uncooperative patient
- Pre-existing neurologic deficit that could prevent the patient from communicating paresthesias or pain during the nerve block
- Obesity obscuring nerve visualization
- Coagulopathy (relative)
General Procedure Setup
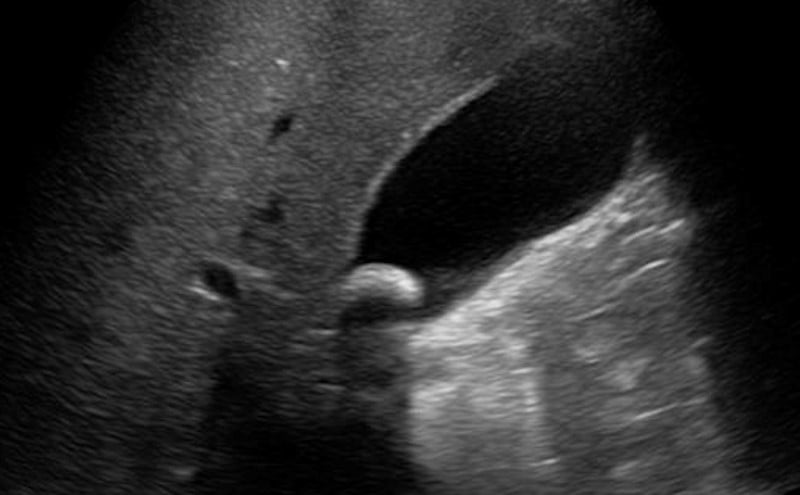
- Minimize ambient light to improve image quality. Placing a spotlight on the block site and darkening the rest of the room can have a dramatic effect on image quality.
- Place machine in direct field of vision of practitioner. Avoid placement that requires twisting or head turning.
- For large volume blocks place the patient on a cardiac monitor, establish IV access and have emergency airway equipment available.
- Provide analgesics and light sedation as needed.
- Obtain consent and document a pre-block neurologic exam.
Injection Precautions
- Remove all air from the needle prior to beginning.
- Ensure the needle is clearly visualized prior to advancing.
- Never inject if the patient complains of intense pain or pressure as this could signify intraneural injection.
- Anesthetic should inject easily with one finger on the plunger. High pressure can be due to intraneural placement.
- Avoid intravascular injection. Always aspirate for blood prior to injecting anesthetic. If injection fails to produce a resulting bolus on the ultrasound image, stop injecting and reposition. If intravascular injection of local anesthetic occurs, then the physician must recognize the potentially life-threatening complication of local anesthetic systemic toxicity (LAST). LAST can lead to cardiovascular collapse. If this occurs, the provider should follow ACLS protocols and administer intralipid emulsion therapy.
In-plane (long-axis) approach
Video 1. In-plane approach
The needle enters the skin at the short side of the transducer and the probe is slid toward the needle until seen
- Course of the needle is parallel to and transects the ultrasound beam
- Bevel faces the transducer
The transducer is readjusted frequently
- Across the axis of the needle to maintain visualization
- Rotated to ensure the ultrasound beam remains parallel to the needle
Advantages
- Needle shaft and tip are well visualized
- Great depth and trajectory information
- Generally easier to master
Disadvantages
- May require the operator to use the needle in their non-dominant hand
- Visualizing a thin needle with a thin ultrasound beam can be challenging
Important Application Information
Providers should choose the appropriate needle gauge, length and type
Larger gauge needles are easier to locate with ultrasound and should be considered for beginners
Several needles are available to perform nerve blocks:
Cutting point needles
- the most common found in the ED
- easily pass through tissue and theoretically could more easily penetrate a nerve if accidentally contacted
Spinal needle (quincke tip)
- non-cutting, long bevel needle
- more difficult to penetrate through tissue
- readily available in a variety of lengths and gauges in most EDs
- used with success in several ED based US-guided nerve block studies
Short-beveled or blunt-point needles
- generally used by anesthesiologists and can be special ordered
- more difficult to pass through tissue and therefore provide feedback to the operator as they pass through tissue planes
- theoretically less likely to cause damage if brought into contact with a nerve. However, no studies have confirmed decreased neural injury with short or blunt point needles
Needle Orientation: In-Plane vs Out-of-Plane Approach
Figure 1. Needle Orientations
2 needle orientations for ultrasound guided procedures, the in-plane and out-of-plane approach
In-plane (long-axis) approach
Video 1. In-plane approach
The needle enters the skin at the short side of the transducer and the probe is slid toward the needle until seen
- Course of the needle is parallel to and transects the ultrasound beam
- Bevel faces the transducer
The transducer is readjusted frequently
- Across the axis of the needle to maintain visualization
- Rotated to ensure the ultrasound beam remains parallel to the needle
Advantages
- Needle shaft and tip are well visualized
- Great depth and trajectory information
- Generally easier to master
Disadvantages
- May require the operator to use the needle in their non-dominant hand
- Visualizing a thin needle with a thin ultrasound beam can be challenging
Out-of-plane (short-axis) approach
Video 2. Out-of-plane approach
The needle enters the skin at the long side of the transducer and the probe is slid towards the needle until seen
- Course is perpendicular to the ultrasound beam
- Bevel faces the transducer
The needle tip and shaft can look the same on ultrasound
The procedure involves allowing the needle to catch up to the ultrasound beam but never pass it:
- Identify the needle tip after piercing the skin
- Slide the probe away from the needle until the tip is no longer visualized
- Advance the needle only until it is seen again
- Slide the probe away from the needle again until it is no longer seen and then advance the needle as above
This process is repeated down to the target
This catch-up motion prevents the needle tip from being lost or passing beyond the beam to damage deeper structures
Out-of-plane (short-axis) Approach
Video 1. Out-of-plane approach
The needle enters the skin at the long side of the transducer and the probe is slid towards the needle until seen
- Course is perpendicular to the ultrasound beam
- Bevel faces the transducer
The needle tip and shaft can look the same on ultrasound
The procedure involves allowing the needle to catch up to the ultrasound beam but never pass it:
- Identify the needle tip after piercing the skin
- Slide the probe away from the needle until the tip is no longer visualized
- Advance the needle only until it is seen again
- Slide the probe away from the needle again until it is no longer seen and then advance the needle as above
- This process is repeated down to the target
- This catch-up motion prevents the needle tip from being lost or passing beyond the beam to damage deeper structures
Advantages
- Easier visualization of surrounding structures (e.g. artery and nerve)
- Needle path can be short
- Operators who perform vascular access in short axis may find this approach more comfortable
Disadvantages
- Tip of the needle and shaft of the needle can look the same
- Needle tracking can be difficult for novices
Visualizing the Needle
During the block, keeping the tip in view is of critical importance. Doing so will result in the highest quality block and avoid the most devastating complications.
A few factors play into how well the tip displays:
- Approach
- The tip is generally easier to visualize with the in-plane approach.
- Needle orientation
- Choosing a shallow angle will also help, as it presents more of the needle to the ultrasound beam for reflection.
- The needle tip should always be oriented such that the bevel is facing toward the probe; this way the broadest, most echogenic portion of the tip is available for reflection.
- Needle gauge
- The larger needles are easier to visualize.
Never advance the needle if you are unsure of the tip position.
- If you lose the tip, slowly rock the probe on its face to scan through the needle. You may need to rotate the probe to align it with the axis of the needle.
- If you are still unsure, withdraw the needle slightly and watch for tissue movement.
- If the tip is not clear, inject 0.5 cc of local anesthetic. This will deform the tissue surrounding the tip, and the anechoic fluid bolus should highlight the tip.
- If these attempts fail to localize the tip, withdraw the needle and choose a different angle or puncture site.
Ensure to inject all air from needles as air in the tissue will prevent visualization of deeper structures.
Anisotropy
Video 1. Anisotropy
Nerves can exhibit strong anisotropy
- Anisotropy refers to the changes in echogenicity of a structure as the angle of insonation is changed.
- Care must be taken to adjust the angle of insonation to ensure optimal nerve visualization.
- Tendons, ligaments and muscle also exhibit anisotropy.