
Early Pregnancy
Matt Rutz, MD, Creagh Boulger, MD, FACEP
I. Introduction and Indications
Pregnancy related complaints are the 4th leading discharge diagnosis for women of childbearing age.1 Many of these women present with pain and bleeding. Frequently the presence of a pregnancy and its location has yet to be confirmed on initial presentation. The differential for these patients is broad and includes but is not limited to viable pregnancy, miscarriage, molar pregnancy, fetal demise, and ectopic. Physical exam and history are often not helpful in delineating the diagnosis. As a result of this diagnostic dilemma, bedside ultrasound has become a useful diagnostic tool in early pregnancy. Bedside ultrasound should be used in conjunction with the serum quantitative B-hCG and the history and physical exam to rule in intrauterine pregnancy.
- Role of this exam is to rule in intrauterine pregnancy
- Specificity of 92-100% for confirming intrauterine pregnancy (IUP) when gestational sac and yolk sac or fetal pole seen.2
- Ultrasound for early pregnancy should be performed when the patient has a pregnancy test to confirm location of pregnancy.
- Ultrasound for early pregnancy should be performed when the patient with a known pregnancy presents with increased pain and or bleeding to assess for viability.
II. Anatomy
Uterus
- Pear shaped, thick walled muscular organ that is posterior to the bladder and anterior to sigmoid colon.
- Positions include:
- Anteverted – Most common position. The uterine fundus pointed toward the anterior abdominal wall.
- Retroverted – Uterine fundus pointed toward the spine. Can make transabdominal imaging more challenging.
Fallopian Tubes and Ovaries
- Fallopian tubes extend laterally from the body of the uterus toward the broad ligament.3
- Ovaries are attached to the uterus by the ovarian ligaments and to the lateral sidewall by the suspensory ligaments of the ovary.
- These are not rigid ligaments so ovarian position can be different
- Illustration 1. Sagittal view of pelvis. Image reproduced from Gray’s Anatomy. (Source: https://en.wikipedia.org/wiki/Vaginal_fornix#/media/File:Gray1166.png)
- Illustration 2. Transverse view of pelvis. Image reproduced from Gray’s Anatomy. (Source: https://ipfs.io/ipfs/QmXoypizjW3WknFiJnKLwHCnL72vedxjQkDDP1mXWo6uco/wiki/Ovarian_fossa.html)
III. Scanning Technique, normal findings and common variants
Sonographic Technique – Transabdominal
- Patient should be supine.
- Use of a 3.5-5 MHz curvilinear probe or phased array probe.
- In thin patients a high frequency linear probe can be used and is helpful for identifying early pregnancies.4
- It is best to have a full bladder for the transabdominal approach.
- Start just above the pubic symphysis in the transverse (probe indicator to the patient’s right).
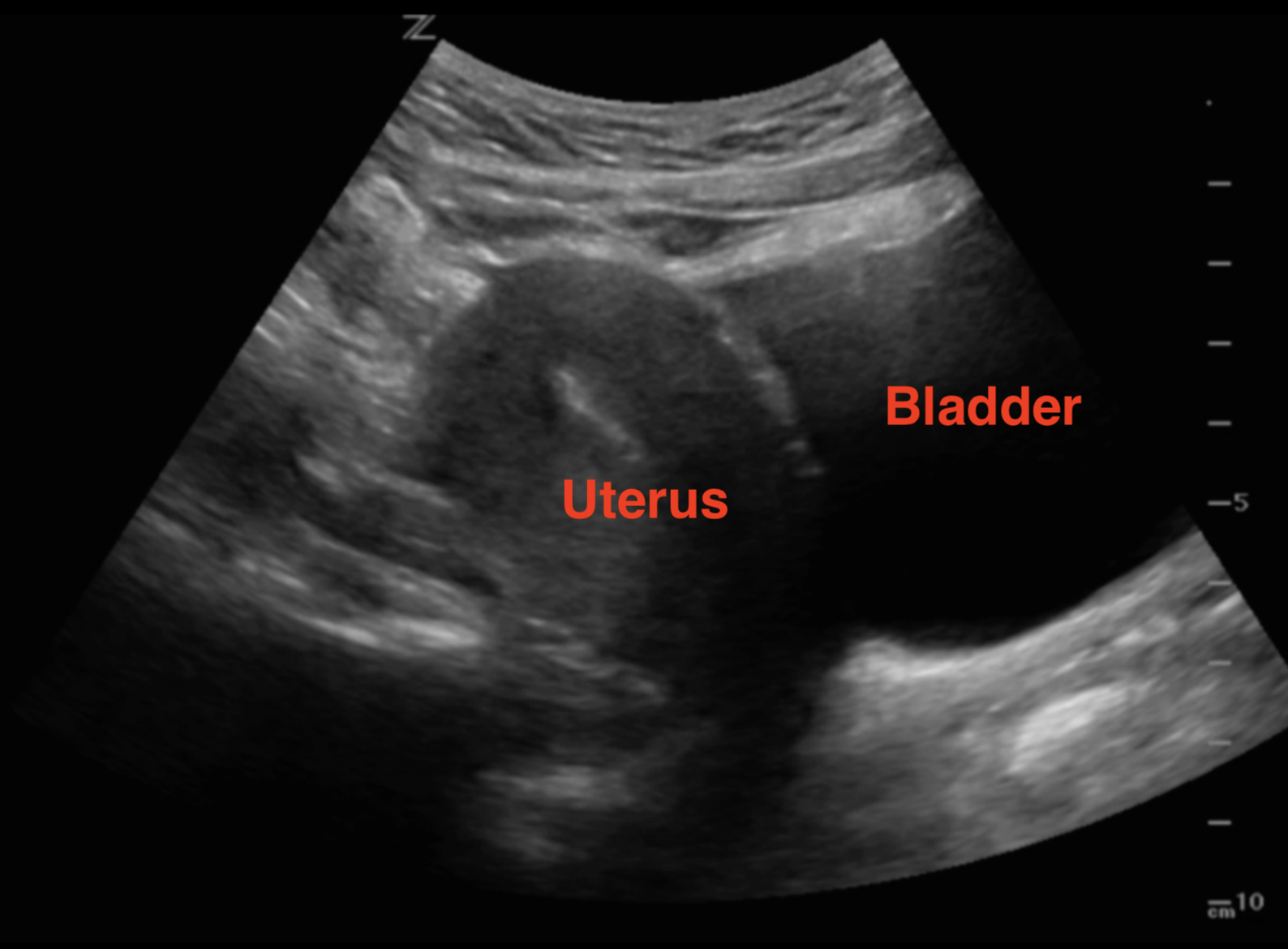
- In the transverse plane use the bladder as an acoustic window to identify the uterus. Fan all the way through by angling the beam towards then head and fan towards the feet. The endometrial stripe should be a hyperechoic line in the middle of the uterus.
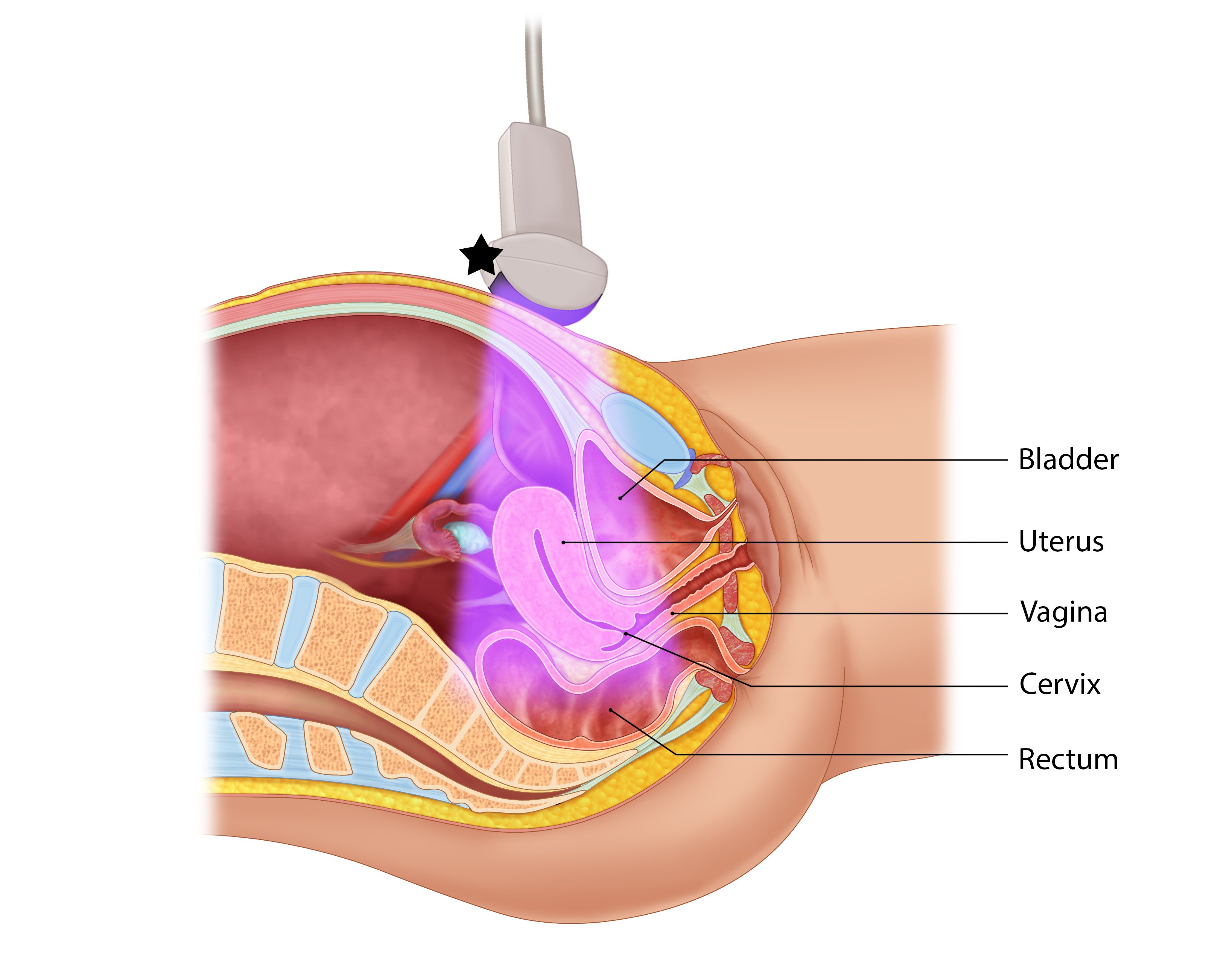
- Illustration 3. Illustration of transverse approach and relevant anatomy. Probe indicator toward patient’s right (star)
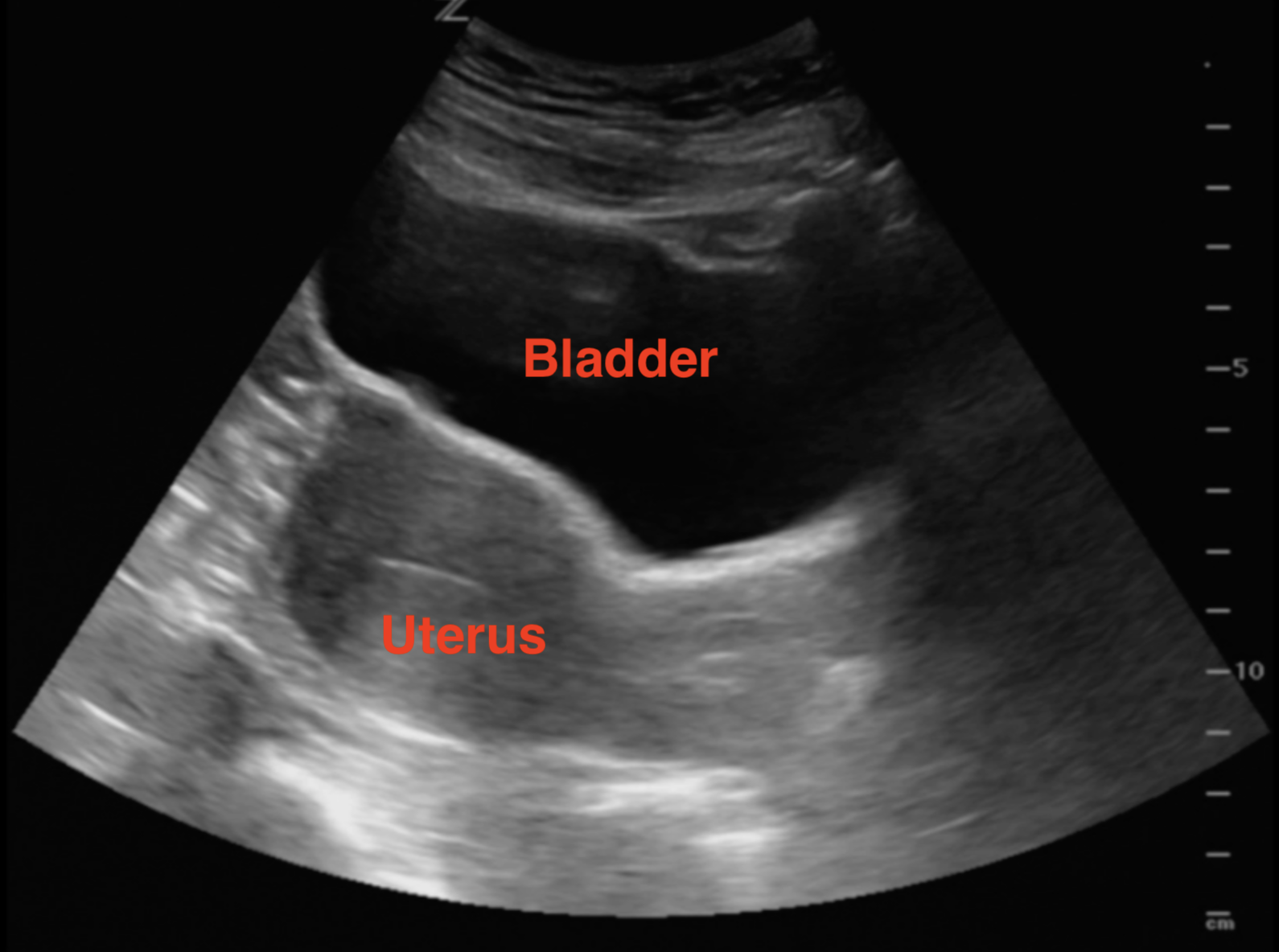
- Illustration 4. Transverse view of pelvis
- Video 1. Transverse view with bladder anteriorly (on top) and uterus posteriorly
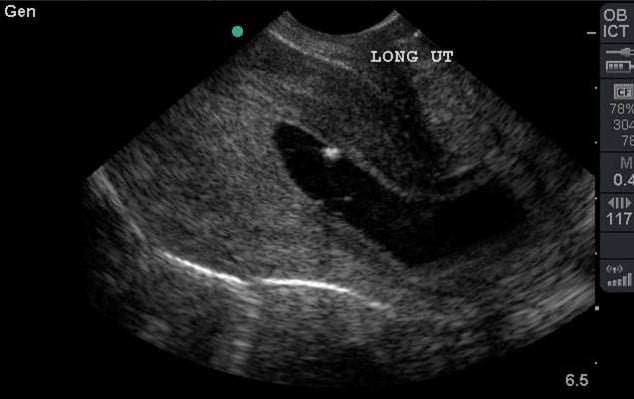
- Rotate the probe towards the patient’s head to and fan left to right in the sagittal plane (Illustrations 5 & 6, Video 2)
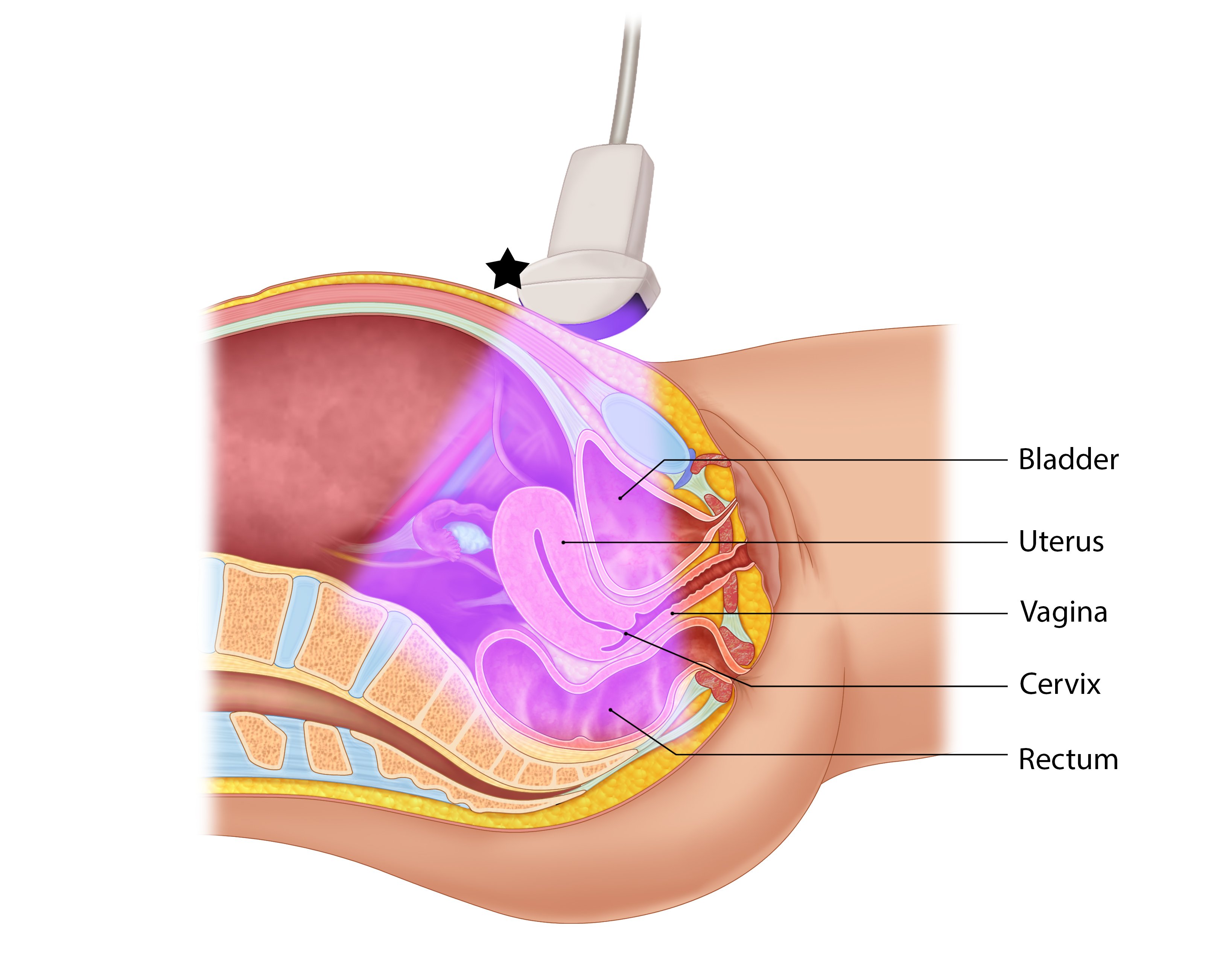
- Illustration 5. Illustration of sagittal approach and relevant anatomy. Probe indicator toward patient’s head (star)
- Illustration 6. Pelvis sagittal view with relevant anatomy
- Video 2. Sagittal view with bladder anterior inferior and uterus superior
- Finally, scan through the ovaries by moving laterally in either transverse or sagittal plane from the uterus. Usually ovaries are not visualized unless there is pathology.
- Focus initially on the entire pelvis looking for pathology such as masses or free fluid. Next focus on fetus for location, fetal heart rate, and dating as necessary.
- If no IUP is identified (Video 1 and 2), look at the hepatorenal recess in the right upper quadrant (RUQ), liver tip, and posterior cul de sac of the pelvis to ensure there is no free fluid. If free fluid is detected, consider ectopic pregnancy (Video 3 and 4). Literature has shown that free fluid in the RUQ in the setting of presumed ectopic is an indication for the operating room.5
Video 3. Positive free fluid in RUQ
Video 4. Sagittal view with large amount of pelvic free fluid with an empty uterus.
Sonographic Technique – Transvaginal
- Patient should be supine in lithotomy position.
- Use a 5-9 MHz endocavitary or transvaginal probe with a water based/non-irritating lubricant and probe cover.
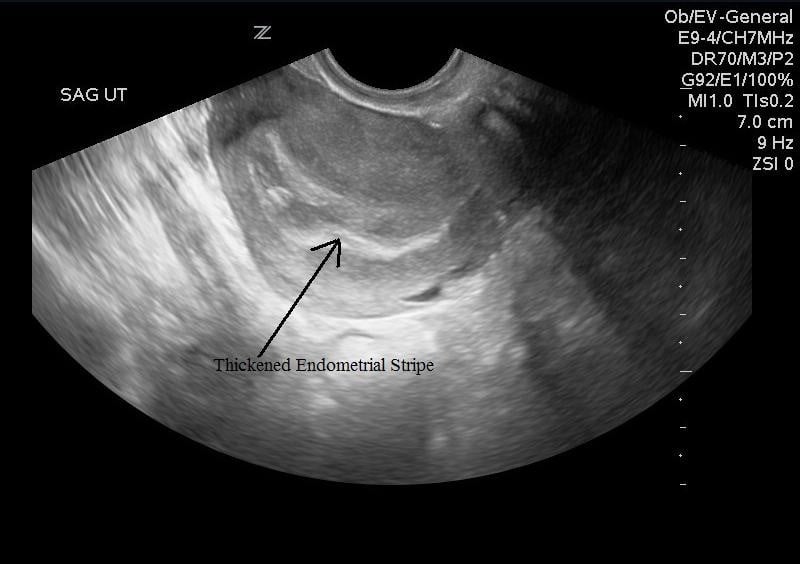
- Insert or have the patient insert the probe into the vagina with probe indicator towards to ceiling. This is the sagittal/longitudinal plane. (Illustrations 7 and 8)
- Fan right to left to view the entire uterus.
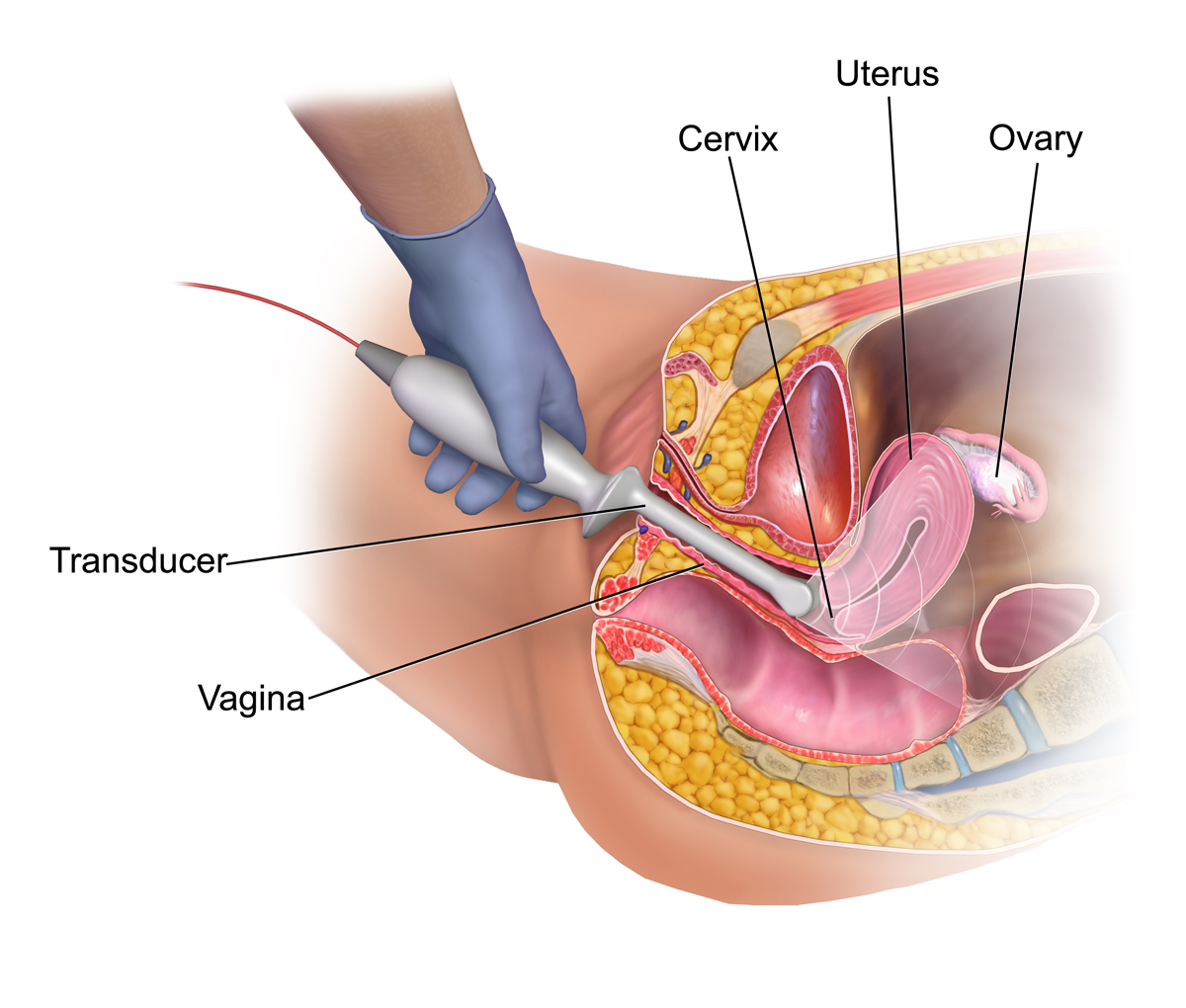
- Illustration 7. Graphic of sagittal or longitudinal transvaginal approach with relevant anatomy. Probe indicator towards the ceiling. Source: WikiCommons (https://commons.wikimedia.org/wiki/File:Vaginal_Ultrasound.png)

- Illustration 8. Image of transvaginal sagittal/longitudinal view. Notice hyperechoic (bright) endometrial stripe.
- Then rotate probe 90 degrees with the transducer indicator to the patient’s right to view the transverse/coronal plane.
- Fan the probe anteriorly and posteriorly to view the entire uterus (Video 5).
Video 5. Transverse/Coronal sweep through the uterus with transvaginal ultrasound. Very hyperechoic (bright) endometrium in the center
- Fan the probe anteriorly and posteriorly to view the entire uterus (Video 5).
- Angle probe into the bilateral adnexa and fan through.
- The fallopian tubes can be tracked to the ovaries which will appear as small cysts in a hypoechoic base from the follicles.
- Evaluation of the ovaries for pathology and vascularity is beyond the scope of point-of-care ultrasound
Normal Findings – Intrauterine Pregnancy (IUP)
- Definitive evidence of an IUP is a gestational sac containing a yolk sac (YS) in two planes within the endometrium which usually occurs around 5-6 weeks gestational age.3,6 (Video 6 and 7)
- There is controversy with this definition; however, any earlier definition (eg, double decidual sign, empty gestational sac) is not accurate enough to ensure an IUP.7
Video 6. Sagittal sweep showing a yolk sac within gestational sac as well as intrauterine pregnancy
Video 7. Transverse/coronal transvaginal view of yolk sac within uterus
- There is controversy with this definition; however, any earlier definition (eg, double decidual sign, empty gestational sac) is not accurate enough to ensure an IUP.7
- Prior to the develop of a YS, a gestation sac (GS) becomes visible in weeks 4-5.
- Be careful not to rely on a GS as an IUP, 10-20% of ectopic pregnancies have pseudo-gestational sacs.8 (Video 8)
Video 8. Sagittal transvaginal view of gestational sac within the uterus. This is not considered an IUP as it could be a pseudo-gestational sac.
- Be careful not to rely on a GS as an IUP, 10-20% of ectopic pregnancies have pseudo-gestational sacs.8 (Video 8)
- A Fetal Pole develops weeks 6-7 and a heart rate is visible in the same time frame (Illustration 9, Video 9)
- Fetal heart rate is best by placing an M-Mode spike across the flickering fetal heart and measuring the repeating pattern. (Illustration 9)
- Do not use pulse wave Doppler as it focuses too much energy (heat) on the fetus and goes against the ALARA (as low as reasonably achievable) principle.
Video 9. Transabdominal fetus with fetal heart rate 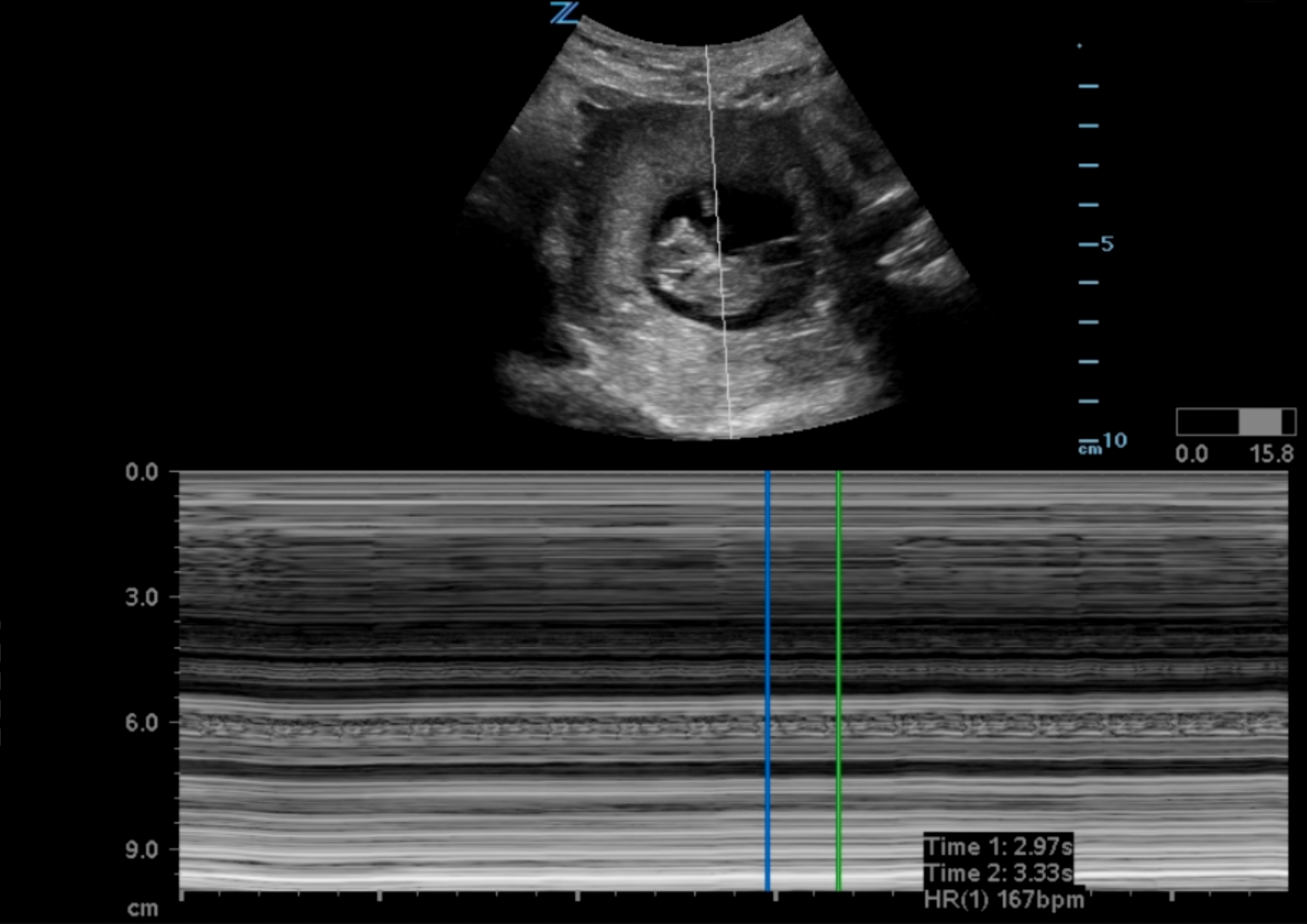
- Illustration 9. M-Mode Tracing Fetal Heart Tones
- Do not use pulse wave Doppler as it focuses too much energy (heat) on the fetus and goes against the ALARA (as low as reasonably achievable) principle.
- Twin gestation is becoming more and more common with fertility treatments.
- Monochorionic pregnancy – Single chorionic sac (Video 10)
- Dichorionic pregnancy – Two chorionic sacs separated by a thick wall (Video 11)
- Dating can be achieved by obtaining crown rump length when fetal pole becomes visible and then biparietal diameter when fetal skull becomes evident at the end of the first trimester.1 (Illustration 10, 11)
Video 10. Transabdominal transverse view of monochorionic triplets
Video 11. Transabdominal transverse view of dichorionic twins. Notice the large septum between the two chorionic sacs. 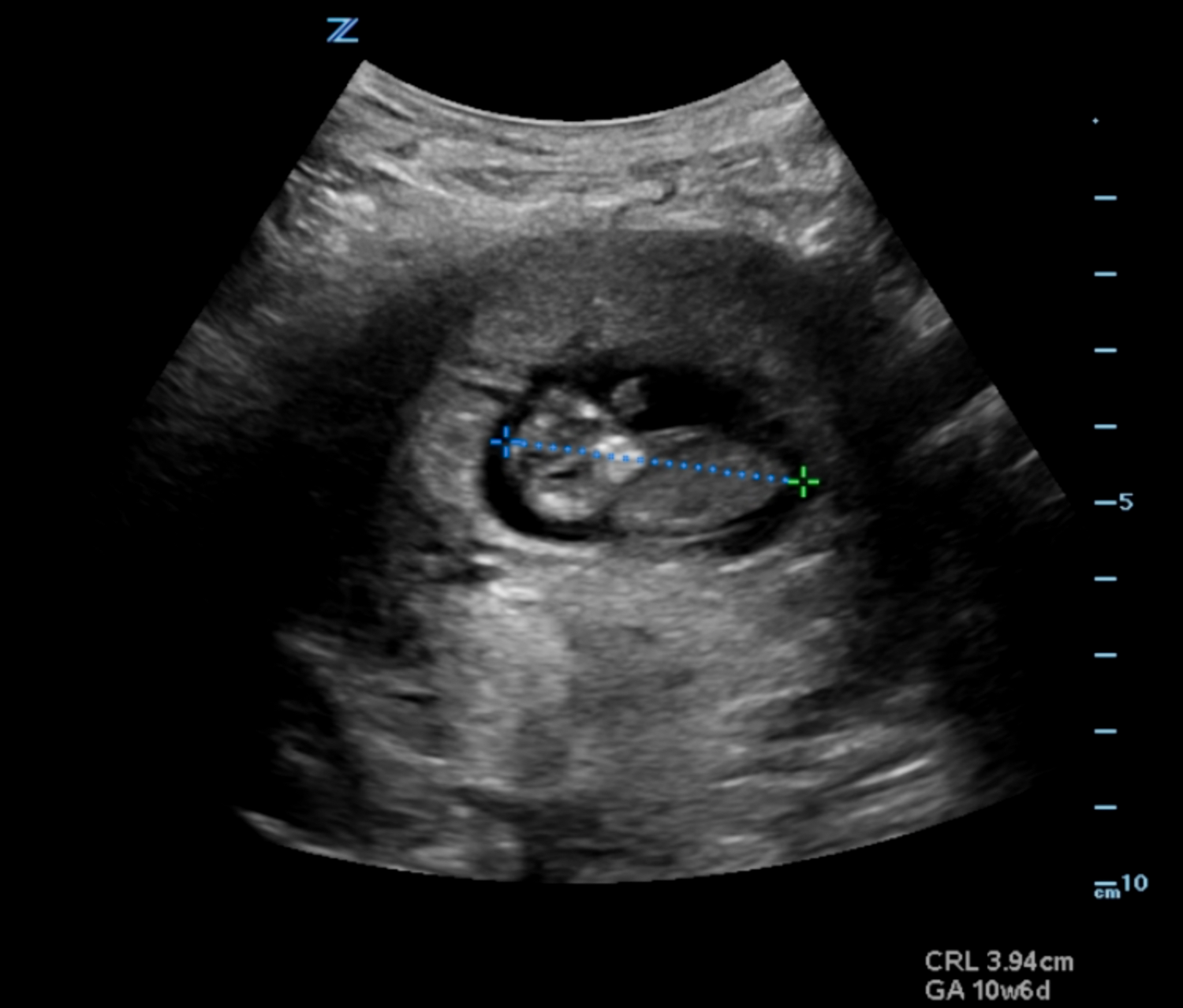
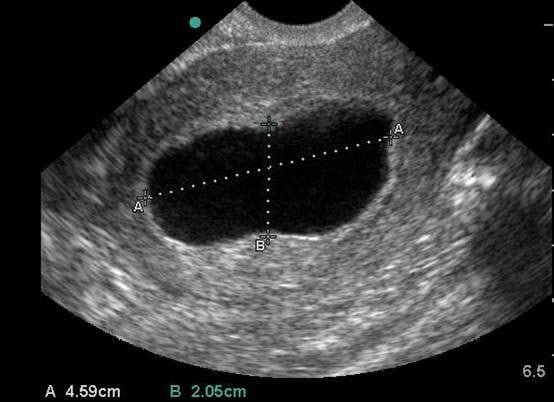
- Illustration 10. Transabdominal transverse view of 10-week fetus with crown rump length measurement.
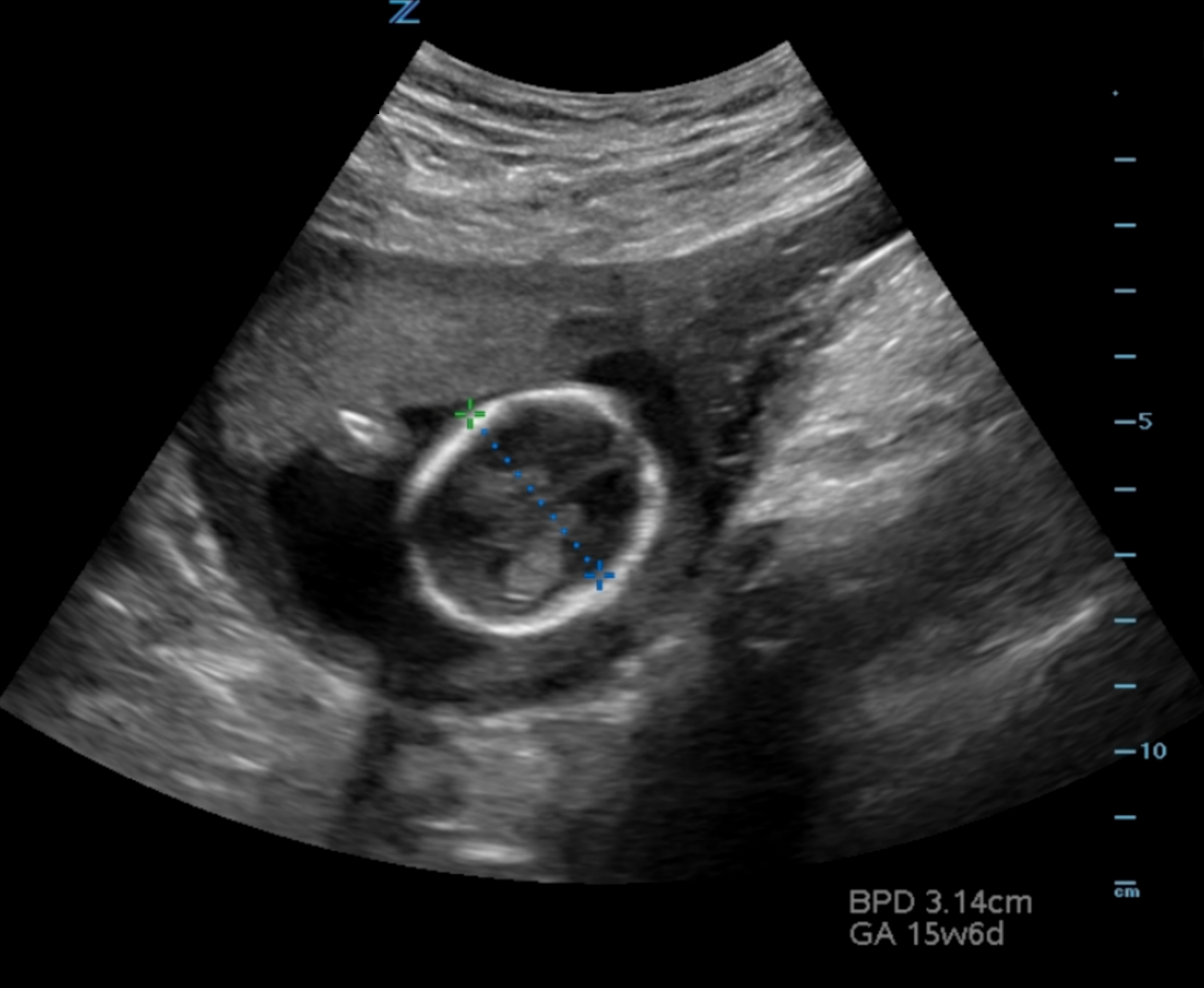
- Illustration 11. Transabdominal transverse view of 15-week fetus with biparietal diameter measurement from leading outer skull (most near field) to inner skull (far field) at the level of the ventricles.
IV. Pathology
- Ectopic
- Pregnancy implants outside of endometrium.9
- 95 % occur in the fallopian tubes (Video 12)
Video 12. Live adnexal ectopic pregnancy - Cervix (Illustration 12)
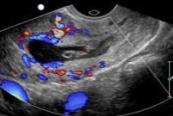
- Illustration 12. Transvaginal ultrasound showing peritrophoblastic blood flow on color Doppler suggesting implantation of the gestational sac into the cervix.
- Peritoneum
- Interstitial portion of fallopian tube – suggested by gestational sac with <5mm of surrounding myometrium (Illustration 13)
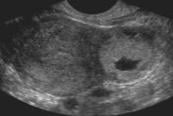
- Illustration 13. Transvaginal ultrasound in a transverse plane showing an interstitial pregnancy.
- Ovarian
- Frequently delayed diagnosis10,11
- Bedside ultrasound can decrease time to diagnosis2,12
- Can develop yolk sac, embryo, fetal heart tones
- Pseudogestational Sac- Empty sac in the uterus, often tear drop shaped. Result of endometrium reacting to secreted hormones but no yolk sac or fetal pole will develop there.13-15
- 95 % occur in the fallopian tubes (Video 12)
- Pregnancy implants outside of endometrium.9
- Miscarriage/Spontaneous Abortion
- Failed pregnancy before 20 weeks
- 10 % all recognized pregnancies16,17
- Guidelines for failed pregnancy18
- Gestational Sac and Yolk Sac x 11 days without FHR
- Gestational Sac > 25 mm without a fetal pole (Illustration 14)
- Fetal pole > 7 mm without a heartbeat (Video 13)
- Illustration 14. Large empty gestational sac
Video 13. Intrauterine fetal demise at 9 weeks - Findings suggestive of failed pregnancy
- Irregular gestational sac (Illustration 15, Video 14)

- Illustration 15. Involuting gestational sac
Video 14. Irregular gestational sac - Discordant measurements of Gestational Age
- Irregular gestational sac (Illustration 15, Video 14)
- Potential Diagnoses
- Threatened Miscarriage- patient with pain and/or bleeding who has a closed os and IUP on ultrasound
- Inevitable/Incomplete Miscarriage- open os with non viable fetus or products of conception in the uterus (Illustration 16)
- Illustration 16. Inevitable spontaneous abortion
- Missed/Completed Miscarriage- os is typically open with no products of conception in the uterus (Illustration 17)
- Illustration 17. Completed spontaneous abortion
- If not diagnosed and products of conception remain non viable, can progress to septic abortion, which is rare.
- Subchorionic Hemorrhage
- Frequent cause of first and second trimester bleeding19
- Anechoic/Hypoechoic crescent around gestational sac (Illustration 18)

- Illustration 18. Subchorionic hemorrhage
Increased risk of miscarriage20,21
- Heterotopic Pregnancy
- Intra and extrauterine pregnancy existing simultaneously (Video 15)
Video 15. Heterotopic pregnancy - Rare- 1/30,000 spontaneous pregnancies but much higher risk in 1/100 assisted reproduction pregnancies22,23
- Increased risk in delay of diagnosis of ectopic and thus increased risk of complications
- Intra and extrauterine pregnancy existing simultaneously (Video 15)
- Molar Pregnancy (also known as Gestational Trophoblastic Disease)
- 1/1000-2000 pregnancies24
- Exaggerated symptoms of pregnancy (hyperemesis, increased breast pain, increased fatigue)
- Excessive levels of serum B-hCG
- Partial Mole- fairly normal appearance of IUP initially and challenging to diagnose
- Complete Mole- “cluster of grapes” appearance (Illustration 19)

- Illustration 19. Molar pregnancy
- High rate of recurrence on subsequent pregnancy25
- Increased risk of choriocarcinoma
V. Pearls and Pitfalls
- For transabdominal scanning have a full bladder
- For transvaginal pregnancy have an empty bladder
- Ensure 5mm of myometrium surrounding the gestational sac so as not to miss an interstitial ectopic
- Central teardrop shaped gestational sacs are concerning for pseudogestational sac
- Must have yolk sac or fetal pole to confirm IUP
- In patients with assisted reproduction, must consider heterotopic pregnancy
- Serum B-hCG is unreliable. Ectopics can exist at all levels and in multiple gestation pregnancies, B-hCG may be unusually high or low for gestational age.
- Fetal heart tones should only be obtained with M-Mode unless significant concern for fetal demise. Avoid color and pulse wave doppler in viable fetus, especially in first trimester.
- Keep-sake imaging and ultrasounds for non-medical reasons are discouraged as there is a theoretical risk to the fetus that may increase from increased exposure.
VI. References
- Niska R, Bhuiya F, Xu J. National hospital ambulatory medical care survey: 2007 emergency department summary. Natl Health Stat Report. 2010:1-31. https://www.cdc.gov/nchs/data/nhsr/nhsr026.pdf
- McRae A, Edmonds M, Murray H. Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: A systematic review. CJEM. 2009;11(4):355-64.
- Ma J, Mateer J, Blaivas M. Emergency Ultrasound 2nd Edition. McGraw Hill; 2008.
- Tabbut M, Harper D, Gramer D, et al. High-frequency linear transducer improves detection of an intrauterine pregnancy in first-trimester ultrasonography. Am J Emerg Med. 2016;34(2):288-91.
- Moore C, Todd WM, O’Brien E, et al. Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007;14(8):755-8.
- Noble VE, Nelson B, Sutingco AN. Manual of Emergency and Critical Care Ultrasound. 2007.
- Richardson A, Gallos I, Dobson S, et al. Accuracy of first-trimester ultrasound in diagnosis of tubal ectopic pregnancy in the absence of an obvious extrauterine embryo: Systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2016;47(1):28-37.
- Yeh HC, Goodman JD, Carr L, et al. Intradecidual sign: a US criterion of early intrauterine pregnancy. Radiology. 1986;161:463-7.
- Kirk E. Ultrasound in the diagnosis of ectopic pregnancy. Clin Obstet Gynecol. 2012;55(2):395-401.
- Gracia CR, Barnhart KT. Diagnosing ectopic pregnancy: Decision analysis comparing six strategies. Obstet Gynecol. 2001;97(3):464-70.
- Mateer JR, Valley VT, Aiman EJ, et al. Outcome analysis of a protocol including bedside endovaginal sonography in patients at risk for ectopic pregnancy. Ann Emerg Med. 1996;27(3):283-9.
- Adhikari S, Blaivas M, Lyon M. Diagnosis and management of ectopic pregnancy using bedside transvaginal ultrasonography in the ED: a 2-year experience. Am J Emerg Med. 2007;25(6):591-6.
- Bhatt S, Ghazale H, Dogra VS. Sonographic evaluation of ectopic pregnancy. Radiol Clin North Am. 2007;45(3):549-60.
- Lin EP, Bhatt S, Dogra VS. Diagnostic clues to ectopic pregnancy. RadioGraphics. 2008;28(6):1661-71.
- Gurel S, Sarikaya B, Gurel K, et al. Role of sonography in the diagnosis of ectopic pregnancy. J Clin Ultrasound. 2007;35(9):509-17.
- Wilcox AJ, Weinberg CR, O’Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med. 1988;319(4):189-94.
- Wang X, Chen C, Wang L, et al. Conception, early pregnancy loss, and time to clinical pregnancy: A population-based prospective study. Fertil Steril. 2003;79(3):577-84.
- Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369(15):1443-51.
- Pearlstone M, Baxi L. Subchorionic hematoma: a review. Obstet Gynecol Surv. 1993;48(2):65-8.
- Tuuli M, Norman S, Odibo A, et al. Subchorionic hematoma (SCH) and adverse perinatal outcomes: Systematic review and meta-analysis. Am J Obstet Gynecol. 2011;204(1 SUPPL.):S149.
- Abu-Yousef MM, Bleicher JJ, Williamson RA, et al. Subchorionic hemorrhage: sonographic diagnosis and clinical significance. AJR Am J Roentgenol. 1987;149(4):737-40.
- Levine D. Ectopic pregnancy. Radiology. 2007;245(2):385-97.
- Human reproduction. Hum Reprod. 2008;23(9):1963.
- Savage PM, Sita-Lumsden A, Dickson S, et al. The relationship of maternal age to molar pregnancy incidence, risks for chemotherapy and subsequent pregnancy outcome. J Obstet Gynaecol (Lahore). 2013;33(4):406-11.
- Berkowitz RS, Goldstein DP. Clinical Practice: Molar pregnancy. N Engl J Med. 2009;360(16):1639-45.



