GI - Appendicitis
Atim Uya, MD
Henry Chaiaza, MD
I. Introduction and Indications
Acute appendicitis is the most common surgical emergency in children with higher incidence between 5-15 years.1
The classic presentation is periumbilical pain radiating to the right lower quadrant with associated anorexia, leukocytosis, low-grade fever, seen in 70% of children.2
Younger children tend to not have a classic presentation and hence are at higher risk of perforation.3,4
Children are particularly at risk for the adverse effects of ionizing radiation.5 Ultrasonography lacks the risks of radiation, is widely available and has been shown to be faster compared to obtaining a CT scan.
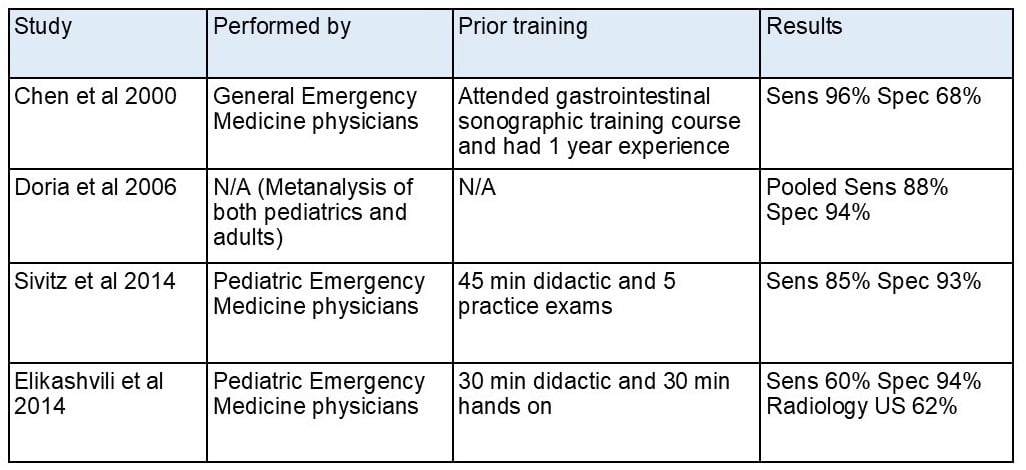
Sensitivity is generally good but there is wide variability, based on user level of experience and when each study was performed. See Table 1 below.6-9
Indications: Patients presenting with right lower quadrant abdominal pain or abdominal pain in younger children where there is suspicion for appendicitis.
II. Anatomy
Relevant anatomy
The appendix is a tubular structure that is connected to the cecum.
Both the cecum and appendix are typically located in the right lower quadrant (McBurney’s point) however; the cecum and appendix can be found in other parts of the abdomen (ie, left lower quadrant in malrotation).
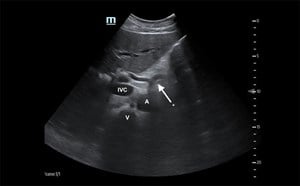
When scanning in the right lower quadrant, the two landmarks that are used to help identify the appendix are the psoas muscle and the iliac vessels (Figure 1).
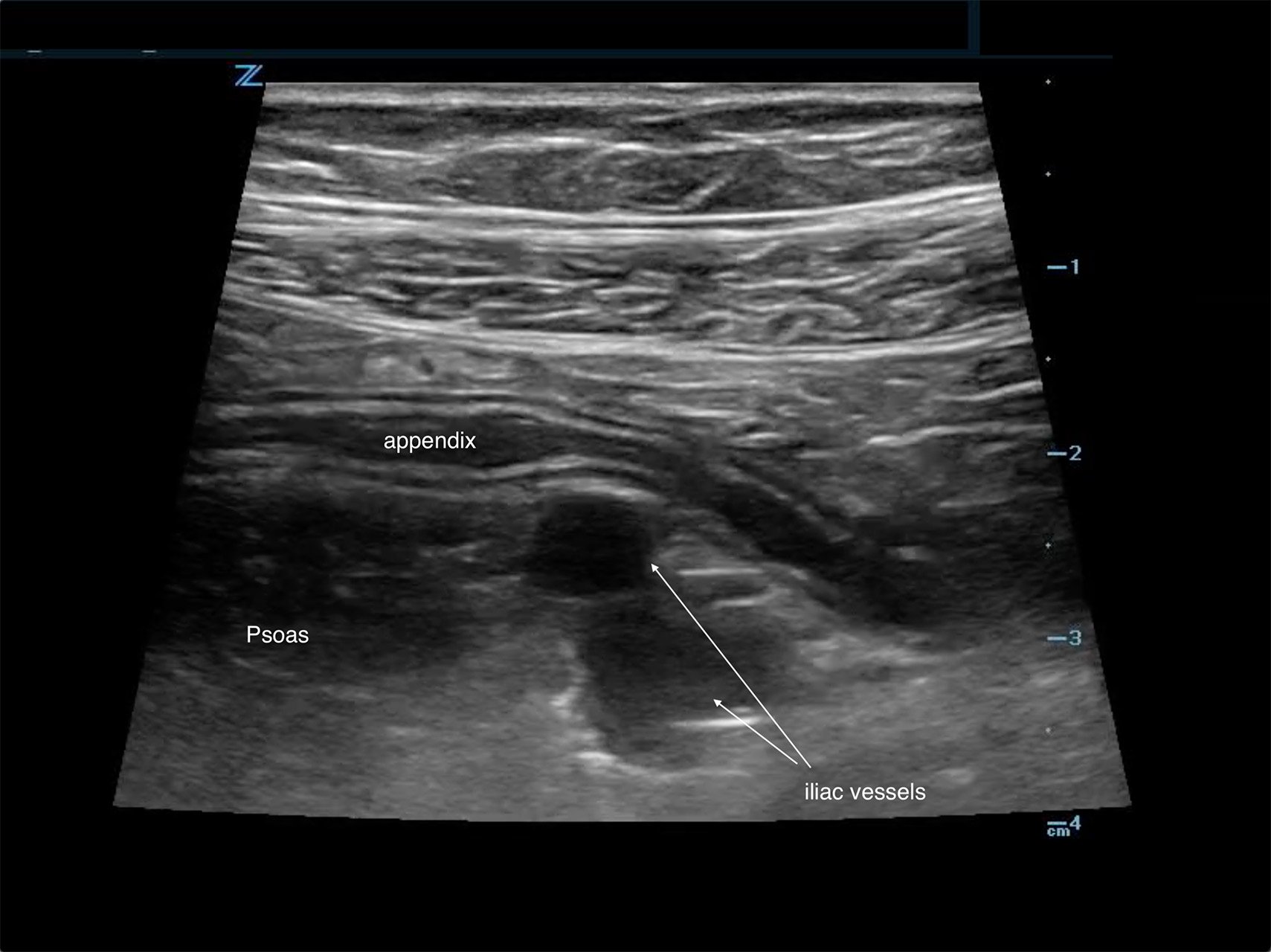
Figure 1. Typical location of the appendix anterior to both the psoas and iliac vessels
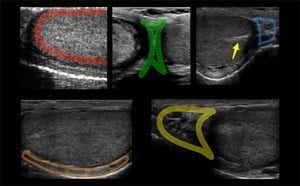
The location of the appendix relative to the cecum can vary as demonstrated in Figure 2.
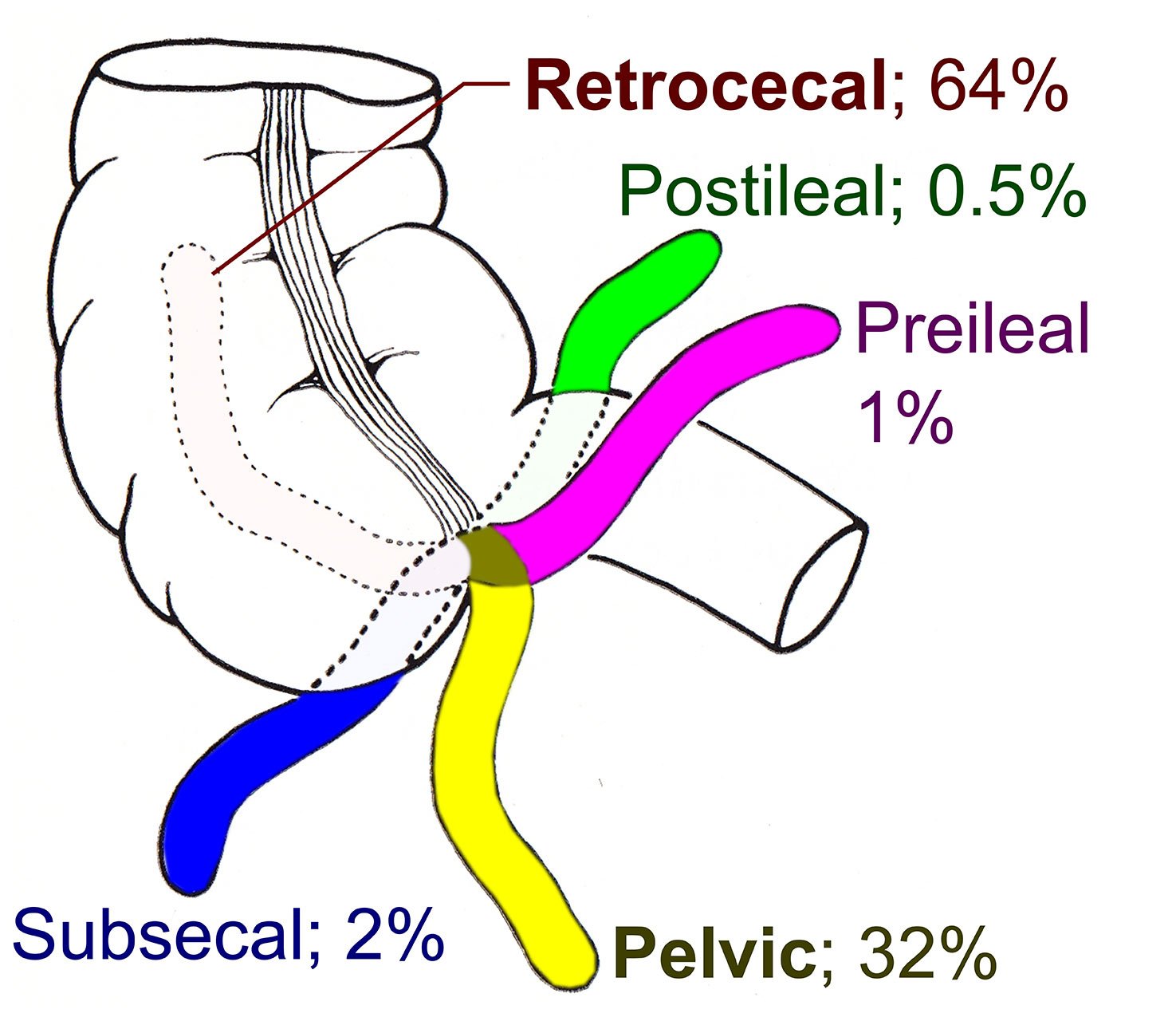
Figure 2. Variant anatomical positions of the appendix
III. Scanning technique, normal findings and common variants
Scanning technique
- Probe selection
Typically, the high frequency linear array transducer (7-12 MHz) is used to scan and evaluate the appendix.
In patients with a larger body habitus the lower frequency probes (curvilinear or phased-array) allow for deeper penetration albeit sacrificing some of the image resolution.
- Scanning approach
Prior to starting your ultrasound exam be sure to adequately treat the patient’s pain. Poor pain tolerance can reduce your ability to obtain good quality images.
The scanning approach depends on how cooperative patient is. If the patient is able to point to the area of maximal tenderness, use this as your starting point for the scan.
“Maximal Area of Tenderness” approach
-
- Place probe over area of maximal tenderness (you can allow the patient to place probe over the area as well)
- Apply graded compression (gradual and increasing steady pressure) to displace bowel gas. Not utilizing this technique may lead to an uncooperative patient due to pain.
- Localize the landmarks in the right lower quadrant. Identify the psoas muscle and the iliac vessels.
- Localize the appendix, which is typically anterior to the psoas and iliac vessels (Figure 1).
If the patient is unable to point to the area of maximal tenderness you can utilize other scanning protocols such as the one presented by Sivitz et al. (Figure 3)8
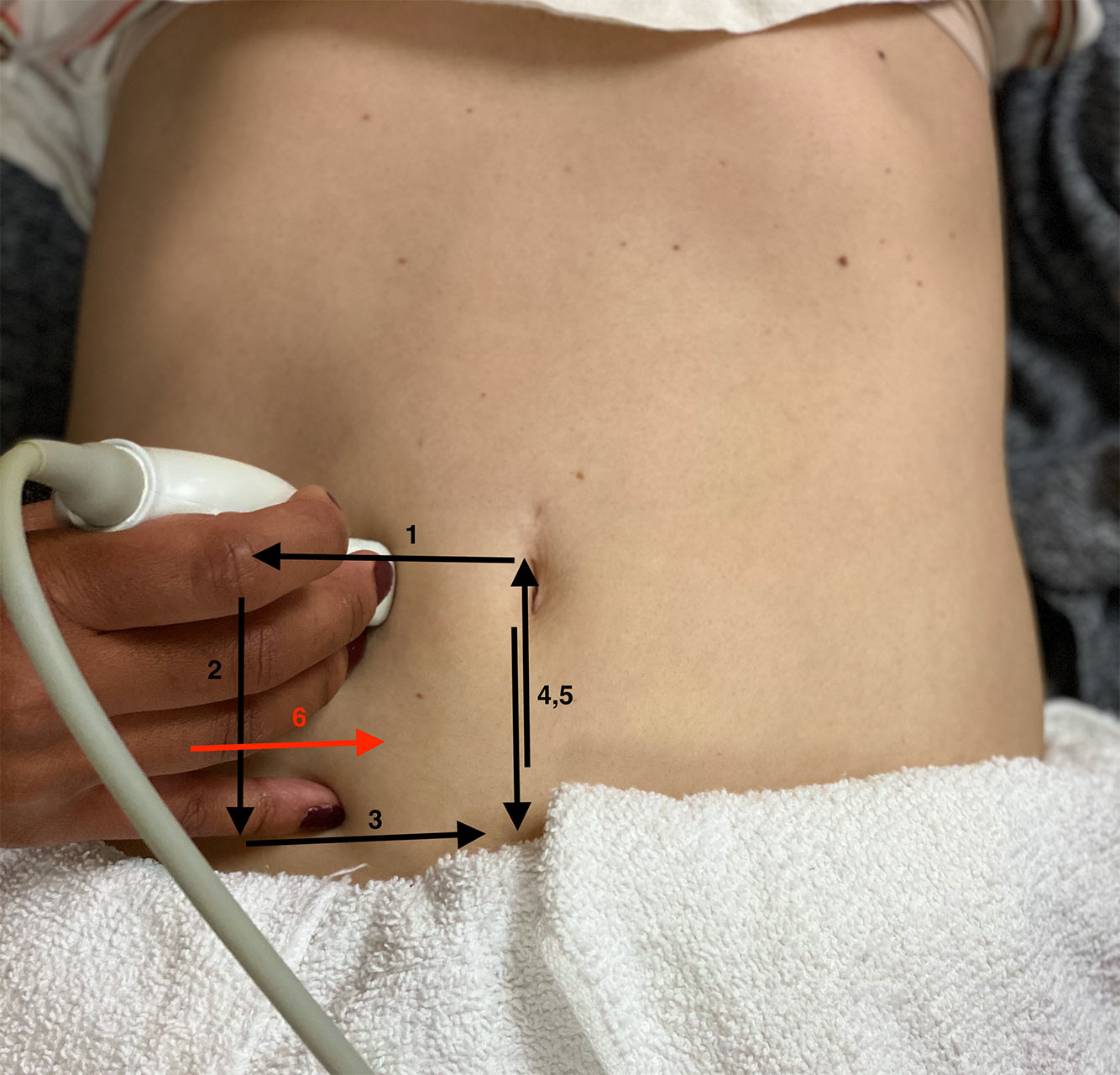
Start by placing your linear probe in a transverse position at the level of the umbilicus. Apply graded compression.
- Move your probe laterally to identify the ascending colon
- Move down to the end of the cecum.
- Move medially and identify the psoas and iliac vessels.
- Move down the border of the cecum.
- Move up the border of the cecum.
- Turn your probe into a sagittal position and identify the end of the cecum in the long axis and move medially across the psoas
Video 1. How to Perform the Scan
Normal findings
The typical normal appendix in children has a characteristic inner hypoechoic band (Figure 4).10,11
This feature allows the appendix to be differentiated from small bowel.
The hypoechoic band is the result of the mucosal layer with abundant lymphoid tissue.

Figure 4. Hyperechoic inner band of normal appendix.
The following video shows a normal appendix lying just anterior to the psoas and iliac vessels
Video 2a, b. Position of appendix anterior to the psoas muscle and iliac vessels.
IV. Pathology
Diagnostic criteria: Appendix measuring more than 6 mm in transverse diameter under compression (98% Sens)1
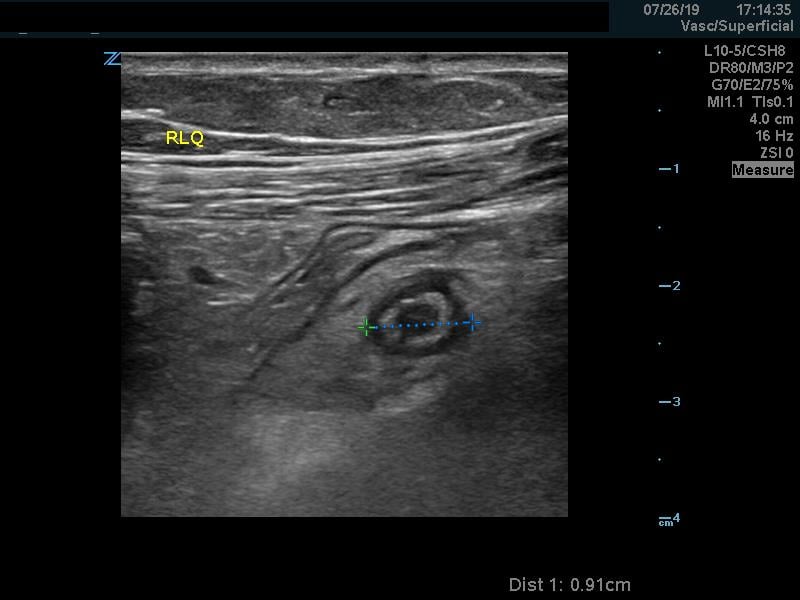
Figure 5. Dilated, non-compressible appendix.
Video 3. Dilated, non-compressible appendix (compression applied).
Other secondary sonographic findings (with varying sensitivities and specificities):
Presence of an appendicolith. Note that this may be seen in normal size appendix. When present, it is associated with an earlier and higher risk of perforation.12
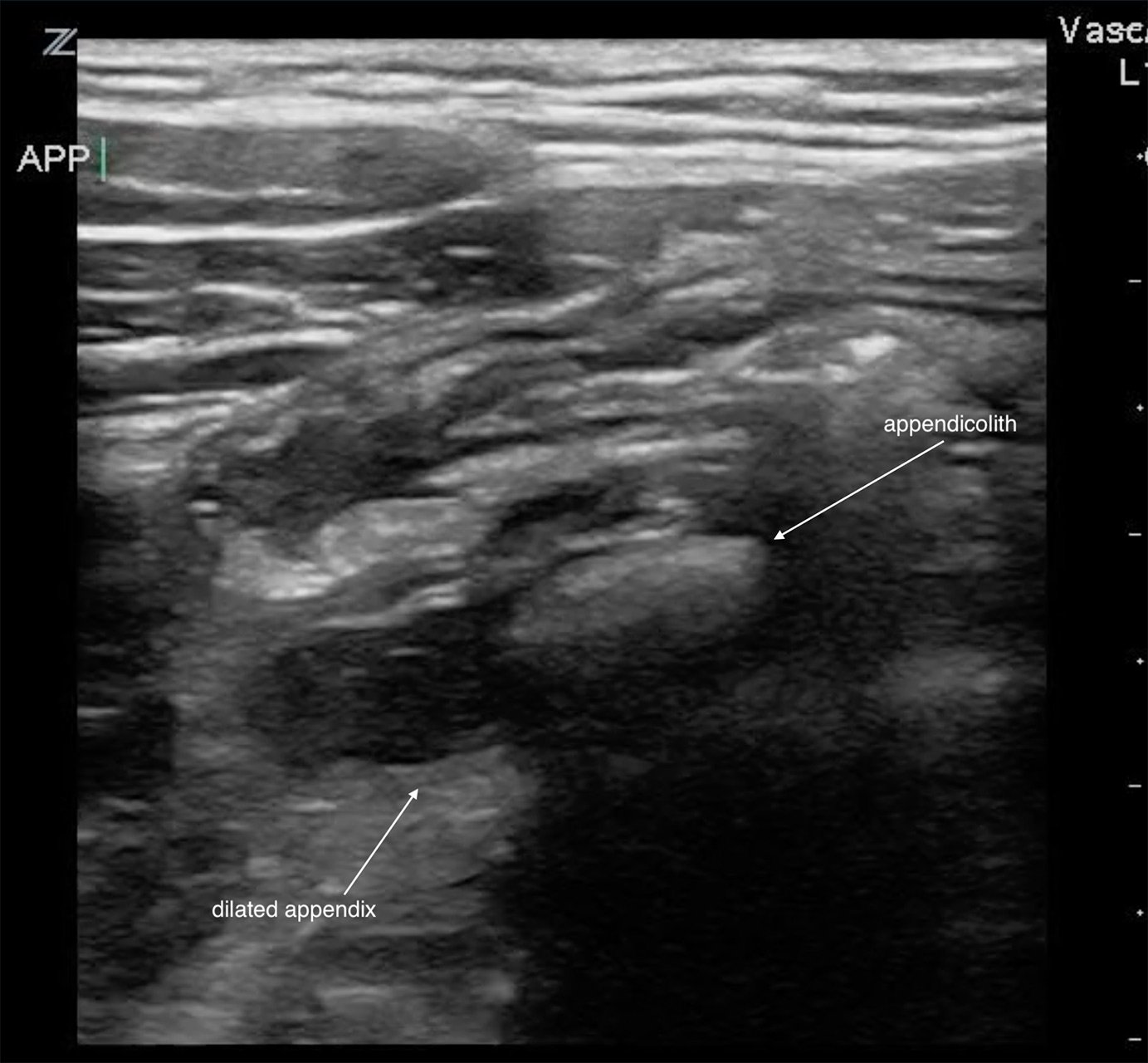
Figure 6. Appendicolith in acute appendicitis.
Video 4. Appendicolith in acute appendicitis.
Hyperemia within the appendiceal wall on color doppler image. Also referred to as a “ring of fire.” (Sens 52%, Spec 96%) Normal bowel wall signal has little to no color flow on Doppler.13
Periappendiceal fat inflammation. On ultrasound, surrounding fat will become hyperechoic.
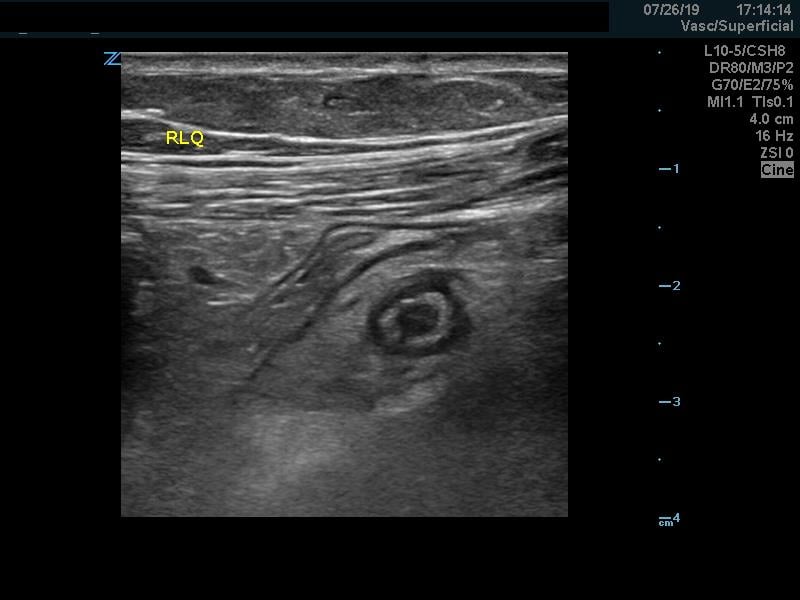
Figure 7. Periappendiceal fat inflammation.
Video 5. Area of hyperechogenicity surrounding the appendix. (Sens 91 spec 76-98%)13 This sign can also be seen in inflammatory bowel disease.
Periappendiceal free fluid.
Treatment
Surgical though using antibiotics as treatment is being explored.14
V. Pearls and Pitfalls
Assuming that non visualization of the appendix means that the appendix is normal. Point-of-care ultrasound should be used to rule in the diagnosis rather than to rule-out especially more inexperienced user.
Confusing other structures for the appendix, eg, the terminal ileum, mesenteric lymph nodes.
Video 6. Recognizing terminal ileum, which has bowel content, is non-blind ending and demonstrates peristalsis.
Perforation may leave the appendix non-distended and may make visualization difficult.
Tip appendicitis: always make sure you visualize the entire appendix including the blind end.
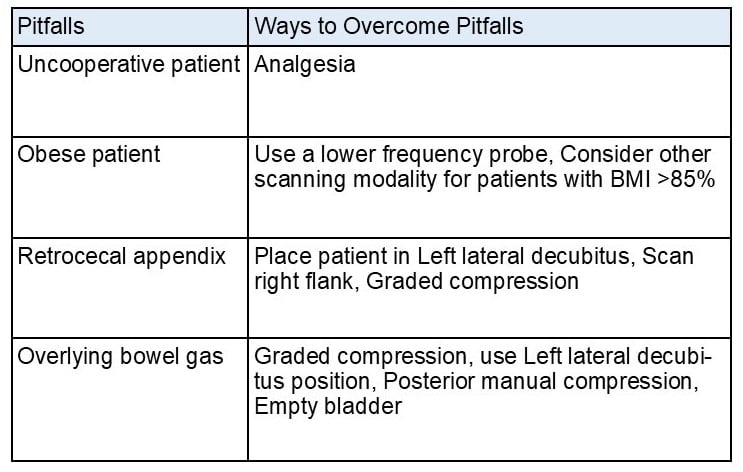
Other pitfalls and ways to overcome them are shown in Table 2.
References
- Cogley JR, O’Connor SC, Houshyar R, et al. Emergent pediatric US: what every radiologist should know. Radiographics. 2012;32(3):651-65.
- Lau WY, Fan St, Yip WC, et al. Acute appendicitis in children. Austl NZ J Surg. 1987;57(12):927-31.
- Sivit CJ, Siegel MJ, Applegate KE, et al. When appendicitis is suspected in children. Radiographics. 2001;21(1):247-262.
- Williams RF, Blakely ML, Fischer PE, et al. Diagnosing ruptured appendicitis preoperatively in pediatric patients. J Am Coll Surg. 2009;208(5):819-25; discussion 826-28.
- Shah NB, Platt SL. ALARA: is there a cause for alarm? Reducing radiation risks from computed tomography scanning in children. Curr Opin Pediatr. 2008; 20(3):243-7.
- Chen SC, Wang HP, Hsu HY, et al. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 2000;18(4):449-52.
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241(1):83-94.
- Sivitz AB, Cohen SG, Tejani C. Evaluation of acute appendicitis by pediatric emergency physician sonography. Ann Emerg Med. 2014;64(4):358-64.
- Elikashvili I, Tay ET, Tsung JW. The effect of point‐of‐care ultrasonography on emergency department length of stay and computed tomography utilization in children with suspected appendicitis. Acad Emerg Med. 2014;21(2):163-70.
- Park NH, et al. Characteristic sonographic appearance of normal appendix in children: inner hypoechoic band without folding. J Korean Radiol Soc. 2004;51(6):663-7.
- Kim BS, et al. Usefulness of the inner hypoechoic band of the vermiform appendix as ultrasonographic criteria for the diagnosis of acute appendicitis in children. J Korean Radiol Soc. 2007;57(5):483-8.
- Alaedeen DI, Cook M, Chwals WJ. Appendiceal fecalith is associated with early perforation in pediatric patients. J Pediatr Surg. 2008; 43(5):889–92.
- Janitz E, Naffaa L, Rubin M, et al. Ultrasound evaluation for appendicitis focus on the pediatric population: A review of the literature. J Am Osteopath Coll Radiol. 2016;5(1):5-14.
- Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156.