E-FAST (Extended Focused Assessment with Sonography in Trauma)
Ultrasound in Trauma - The Extended FAST Exam
Andrea Rowland-Fisher, MD
Robert F. Reardon, MD, FACEP
I. Introduction and Indications
- Trauma patients often have injuries that are not apparent on the initial physical exam. These injuries can be even more difficult to detect in patients with distracting injuries or altered mental status.
- The purpose of bedside ultrasound in trauma is two-fold; (1) to rapidly identify free fluid (usually blood) in the peritoneal, pericardial, or pleural spaces and (2) to identify the presence of a pneumothorax.
- It is most important in the most unstable patients, when management decisions cannot wait for a CT scan or even a chest radiograph.
- The FAST exam has been long established.
- Physicians in Germany and Japan began using routine bedside ultrasound for trauma patients in the 1970's.1
- In the United States emergency physicians started using this tool in the 1980’s2,3 and it has now become the initial imaging test of choice for trauma care in the United States and is part of the Advanced Trauma Life Support (ATLS) protocol developed by the American College of Surgeons.
- “FAST” is an acronym for Focused Assessment with Sonography in Trauma and has become synonymous with beside ultrasound in trauma.4,5
- The FAST exam, per ATLS protocol, is performed immediately after the primary survey of the ATLS protocol.
- Ultrasound is the ideal initial imaging modality because it can be performed simultaneously with evaluation and resuscitation, providing vital information without the time delay caused by radiographs or computed tomography (CT).
- The concept behind the FAST exam is that many life-threatening injuries cause bleeding. Although ultrasound is not 100% sensitive for identifying all bleeding, it is nearly perfect for recognizing intraperitoneal bleeding in hypotensive patients who need an emergent laparotomy and for diagnosing cardiac injuries from penetrating trauma.6-9
- Research studies have shown that bedside ultrasound is equivalent to, or better than, chest radiography for identifying a hemothorax or pneumothorax in trauma patients.10-13 For this reason, most trauma centers now use the extended FAST exam (EFAST), evaluating for pneumo- and hemothorax in addition to intraperitoneal injuries.10,11,14
- Physicians should understand the potential applications of trauma ultrasound as well as the common pitfalls and their own technical limitations. It is important to recognize the imperfect nature of such exams, but sonographers who master this challenge, will find it an invaluable tool in the care of trauma patients.14-16
II. Specific Indications
Penetrating Cardiac Trauma
- Bedside ultrasound performed by emergency physicians significantly decreases mortality in patients with penetrating cardiac injuries.9
- Many patients with stab wounds to the heart do not suffer significant blood loss because the wound in the pericardium seals, creating a pericardial effusion.
- Prior to the development of tamponade, which can be delayed by several minutes to hours, patients will be relatively asymptomatic.
- The “classic” signs of Beck’s triad are not commonly present.
- The key to managing penetrating chest trauma is to identify a developing pericardial effusion as early as possible, before tamponade and cardiac arrest occurs.
- All patients with penetrating chest injury should be “screened” for a potential pericardial effusion. If an effusion is present, cardiac injury is assumed until proven otherwise and the patient should go directly to the operating room for a pericardial window or sternotomy.
Blunt Cardiac Trauma
- Significant blunt cardiac injury is relatively uncommon.
- Most patients who suffer severe cardiac injury such as rupture of the free ventricular wall die quickly.
- One research report described patients with blunt cardiac rupture who were rapidly diagnosed and aggressively managed because of early bedside ultrasound.17
- The authors stressed the importance of prompt cardiac ultrasound in all patients with significant blunt chest trauma.
- Cardiac rupture causes a pericardial effusion and although blunt cardiac rupture is rare, the cardiac portion of the FAST exam should still be performed on all patients with significant blunt chest trauma, especially those who are hypotensive.17
Blunt Abdominal Trauma
- Intraperitoneal bleeding after blunt trauma is common.
- It is usually the result of a spleen or liver injury and difficult to diagnose on physical exam.
- The FAST exam is an ideal initial screening modality for early recognition of intraperitoneal blood since it is rapid, safe and can be repeated if the patient’s status changes.
- The utility of the FAST exam in blunt abdominal trauma has been questioned given is poor sensitivity particularly in those that are hemodynamically stable and for its lack of ability to detect specific organ injuries and retroperitoneal injuries. This criticism has been heightened as the use of whole-body CT has grown in favor for those with severe trauma.
- One study showed that even though there is a high rate of false negative FAST exams (49%), there is no increase in mortality or ICU length of stay. Furthermore, those with a false negative FAST were less likely to require a laparotomy.18
- In those that are hemodynamically unstable, the FAST exam has been shown to be of benefit, and furthermore, Neal et al showed that obtaining a CT in this group of patients resulted in a higher mortality.19
Penetrating Abdominal Trauma
- The sensitivity of the FAST exam in penetrating trauma has been shown to be anywhere from 28%-100%. While it lacks sensitivity, the specificity is high ranging between 94-100%.
- If the FAST is negative, further investigation is needed either through exploratory laparotomy, local wound exploration, DPL, serial abdominal exams or CT scan.20
- The sensitivity of the FAST exam for determining the need for laparotomy is only about 50%.21
- Bowel injuries are very common in penetrating trauma and the FAST exam does not detect most of these injuries.
- Some clinicians think that this low sensitivity makes the FAST exam less useful in penetrating trauma, but others advocate it as a valuable tool to help assess for significant hemoperitoneum and to help prioritize management when multiple penetrating injuries are present.15,22-25
Chest Trauma
Hemothorax
- Bleeding into the pleural space, called a hemothorax, is common in both blunt and penetrating trauma.
- About 200 mL of pleural fluid is required before it can be detected with a plain CXR.26
- As little as 20 mL of fluid can be seen with ultrasound.27
- Ultrasound was found to be equivalent to CXR in detecting hemothoraces in trauma and also could be performed more rapidly, taking about 1 minute versus 15 minutes for chest radiography.12,13
- Chest radiographs are still necessary in trauma patients to evaluate the mediastinum, lung parenchyma and several other anatomic features.
- Ultrasound can be used during the initial minutes of the trauma evaluation to determine if urgent chest tube placement is necessary. A chest radiograph can then be obtained after chest tube placement. This approach saves valuable time when managing an unstable multiple-trauma patient.13,15,28
Pneumothorax
- Pneumothoraces are common in trauma and more than half are missed on a supine chest radiograph.29
- Bedside ultrasound has been shown to be more sensitive than CXR for detecting this lung injury.10,11,29-32
When is Trauma Ultrasound Most Useful?
- Ultrasound is most useful in unstable critically ill patients, to help clinicians determine the etiology of shock and direct immediate management decisions.
- While CT has better accuracy for diagnosing both blunt and penetrating torso injuries, the FAST exam is most useful in situations where CT is not practical due to time constraints.
- CT of the abdomen is better than ultrasound for showing parenchymal injury and the source of intraperitoneal bleeding.
- CT is useful to differentiate solid organ injury from bowel injury or other causes of hemoperitoneum and it is far superior demonstrating retroperitoneal bleeding.
- Modern CT scanners can also use abdominal/pelvic images to reconstruct bone windows and rule-out fractures of the spine and pelvis.
III. Clinical scenarios where the FAST is most useful
- Hemodynamically unstable patients, when the cause of hypotension is unclear.
- Patients who need an emergent bedside procedure.
- Patients at a community hospital who require transfer to a trauma center. Consider pericardiocentesis if a pericardial effusion is found, consider early blood transfusion for significant hemoperitoneum, and consider a chest tube if a hemothorax or pneumothorax is discovered, especially if aeromedical transport is planned.
- Intoxicated patients who can be observed and re-examined.
- Patients with penetrating trauma with multiple wounds or unclear trajectory, especially with wounds in upper abdomen or lower chest.
- Patients with a concerning mechanism of injury but no indication for CT. Consider a period of observation and serial FAST exams.
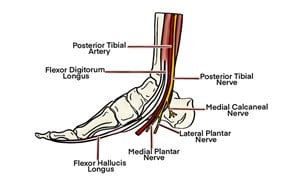
IV. Anatomy
- The FAST exam evaluates potential spaces where free fluid could accumulate. These potential spaces are located in the pericardium, right upper quadrant/hemidiaphragm, left upper quadrant/hemidiaphragm, and pelvis.
- The “extended” portion of the EFAST exam evaluates for a pneumothorax by observing the lung pleura for sliding. Sliding occurs when the parietal pleura that lines the thoracic cavity glides along the visceral pleura that covers the lung with inspiration and expiration.
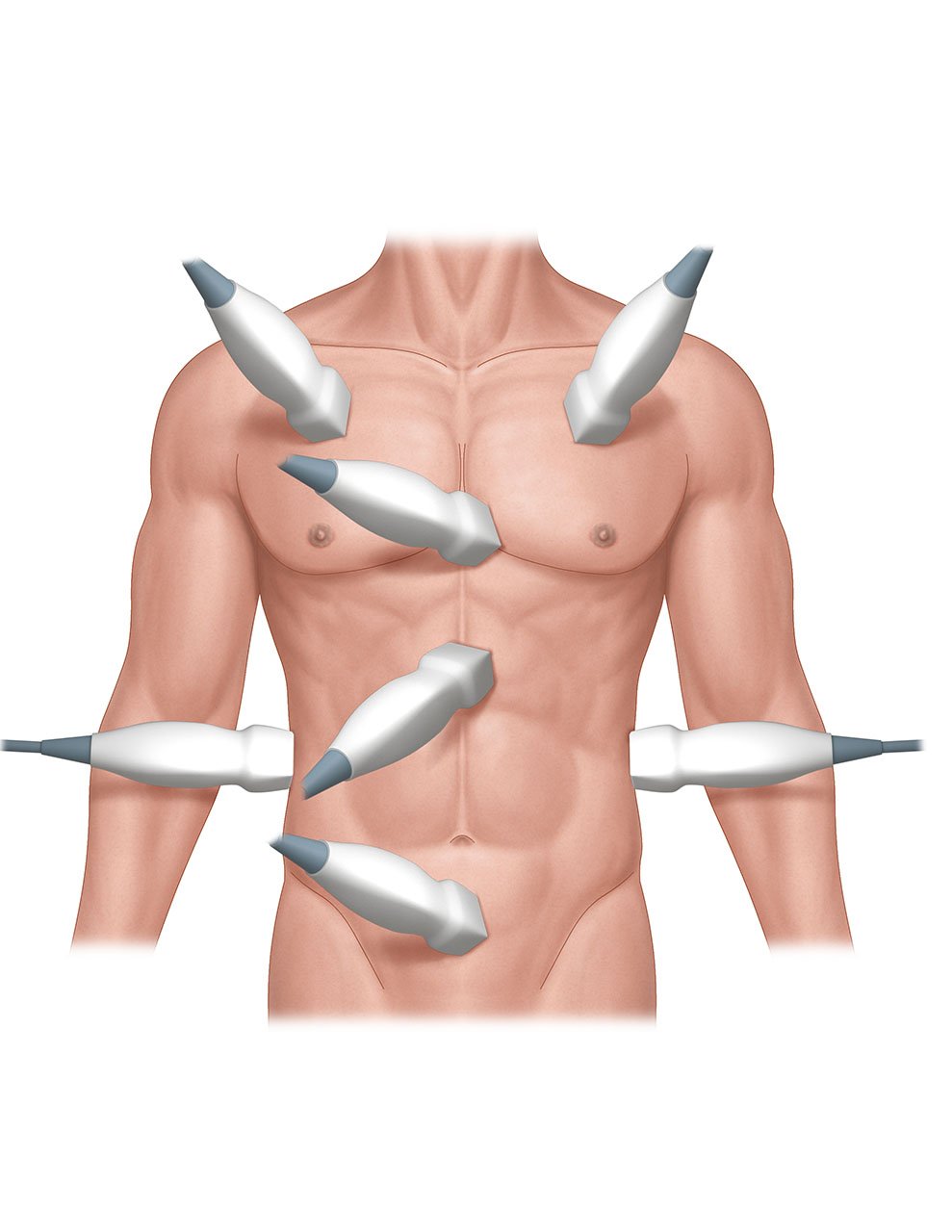
- Illustration 1. Overview of regions scanned in EFAST exam
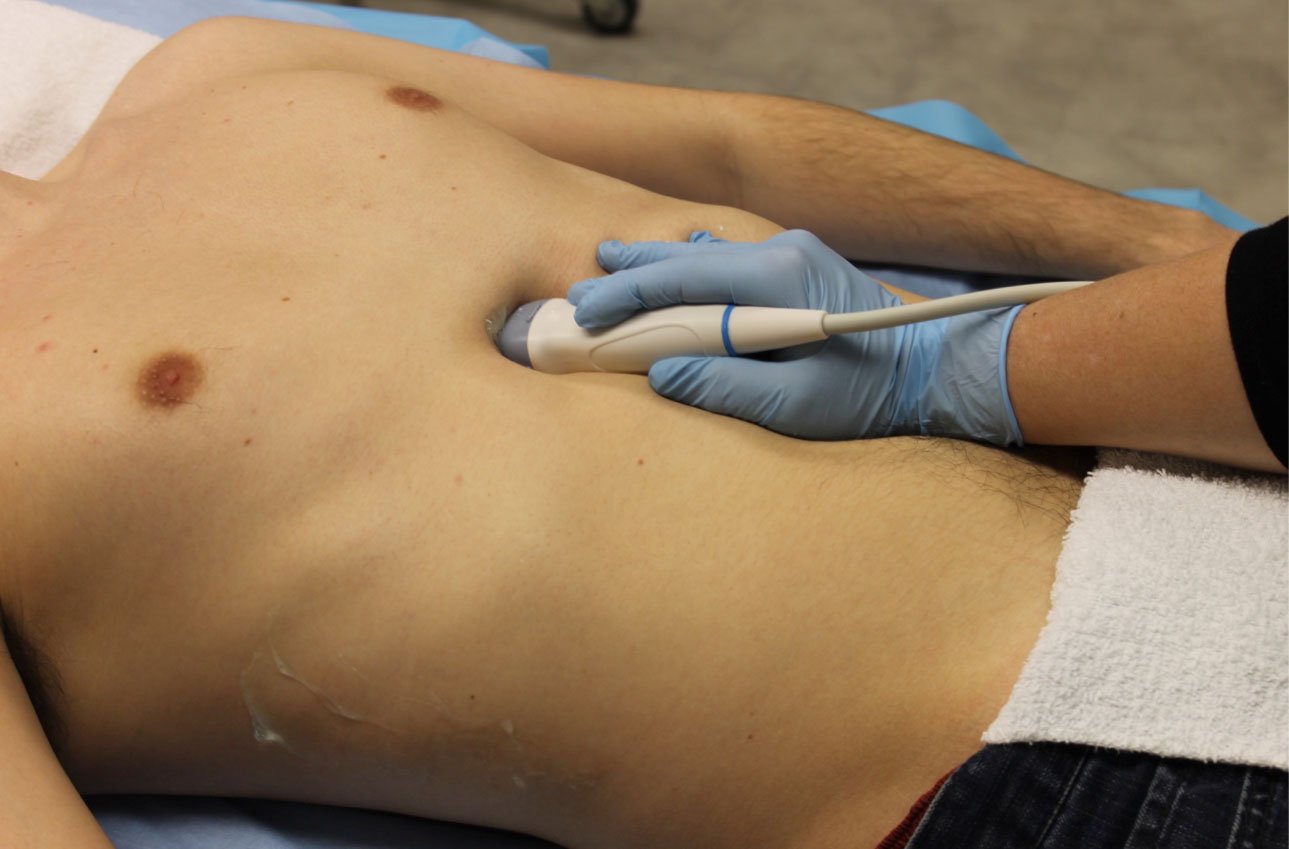
V. Scanning Technique and Normal Findings
- The FAST exam can be effectively performed with limited scanning planes since the objective is to find free fluid and not do a comprehensive survey of the involved organs. This approach makes the FAST exam easier to learn and less time consuming.
- The exam is performed in the supine position with either a phased array or curvilinear transducer. The ultrasound machine should be set on a FAST or abdominal setting with the screen indicator on the left side.
- Normal findings show regular anatomy and no intraperitoneal or intrathoracic fluid.
- Lung sliding signs should be present in the normal lung.
VI. Abnormal Findings
- The purpose of the FAST exam is to:
- Find free fluid (usually blood) in the pericardial, pleural, or intraperitoneal spaces
- Detect a pneumothorax by lack of lung sliding signs
- Free fluid is jet black on the screen and tends to collect in the most dependent areas and surround the organs.
- Interpretation of the FAST exam involves learning where free fluid commonly collects adjacent to these organs.
- The volume of intraperitoneal blood that can be detected using the FAST exam depends on the skill of the operator and which views are obtained.
- To optimize sensitivity to detect the smallest amount of free fluid possible, it is important to obtain good images of multiple intraperitoneal sites.33
- A good quality FAST can probably reliably detect about 200 mL of free intraperitoneal fluid, however, the mean volume needed for a FAST to be positive was 619 mL.1,34
- If good images of the pelvis are obtained, requiring more technical skill, even smaller volumes may be detected.33,35
- Placing a patient in the Trendelenburg position improves the sensitivity for detecting free fluid in the Morison's pouch view.36
- As noted previously, and most importantly, the FAST exam is nearly perfect for detecting intraperitoneal bleeding that causes shock and requires an emergent laparotomy.6,7
Cardiac Views
- There are two different cardiac views that can be performed with the FAST exam. It is important to learn both views, because one of the views may be easily obtained and the other impossible in any given patient.
- Please note that this chapter demonstrates one of the three most common orientations for cardiac visualization by emergency providers. In this chapter, one of the orientations favored by emergency physicians is utilized and can be seen with the indicator to the top left of the image. Further information on this topic can be found in the cardiac chapter.
Subxiphoid Four-Chamber View
- Place the probe in the subxiphoid region with the transducer indicator toward the patients’ right side or right shoulder. Angle the probe toward the left shoulder.
- Figure 1. Position of the ultrasound probe for the subxiphoid view
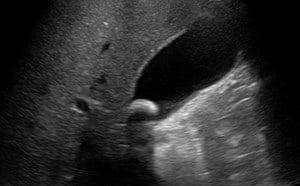
- This view shows the right ventricle immediately adjacent to the left lobe of the liver. (Figure 2, Video 1) A pericardial effusion will be easily recognized between the liver and the heart. (Video 2)
- Increasing the depth of the image, applying more pressure, and having the patient take a deep breath will improve chances of obtaining a good image.
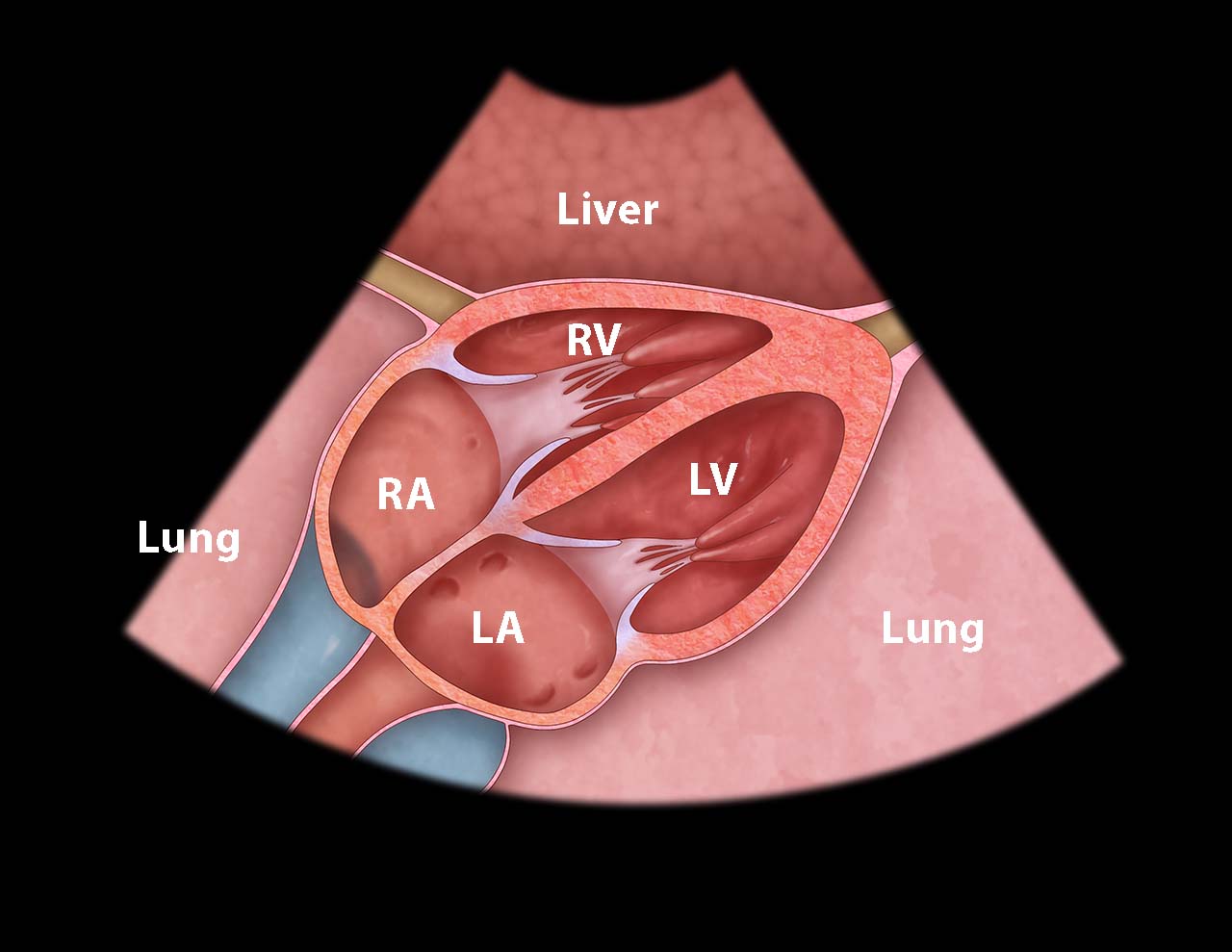
- Illustration 2. Cardiac anatomy from subxiphoid view
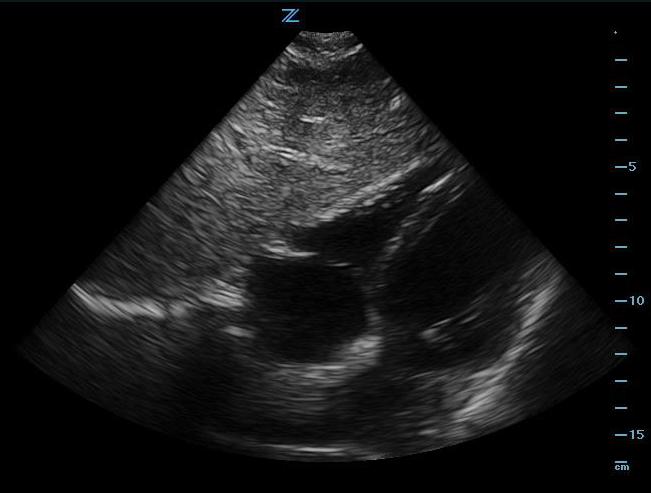
- Figure 2. Subxiphoid view
- Video 1. Subxiphoid view
- Video 2. Pericardial effusion (black stripe between liver and right ventricle)
Parasternal Long-Axis View
- Place the probe just to the left of the sternum in the 4th or 5th intercostal space, directly over the center of the heart, with the transducer indicator toward the 4 o’clock position. (Fig. 3)
- This view shows the anterior and the posterior pericardium. (Video 3) Sliding the probe toward the cardiac apex (toward the 4 o’clock position) provides a good look at the apex.
- This view requires less depth and is easier to obtain in uncooperative patients. To improve this view, have the patient exhale or positions the patient in left lateral decubitus position if they are able.

- Illustration 3. Cardiac anatomy from parasternal long axis view

- Figure 3. Position of the ultrasound probe for the parasternal long axis-view
- Video 3. Parasternal long axis-view
Abdominal and Lower Thoracic Views
- When a patient is in the supine position the most dependent area in the upper peritoneum between the liver and right kidney, also known as Morison's pouch, and the most dependent area in the lower peritoneum is posterior to the bladder in the male and the pouch of Douglas (posterior to the uterus) in the female.
- Right Coronal and Intercostal Oblique Views:
- The easiest abdominal view to obtain is the view of Morison’s pouch. (Ill. 4)
- Place the probe in the mid-axillary line at about the 8th to 11th intercostal space with the transducer indicator pointed cephalad. (Fig. 4)
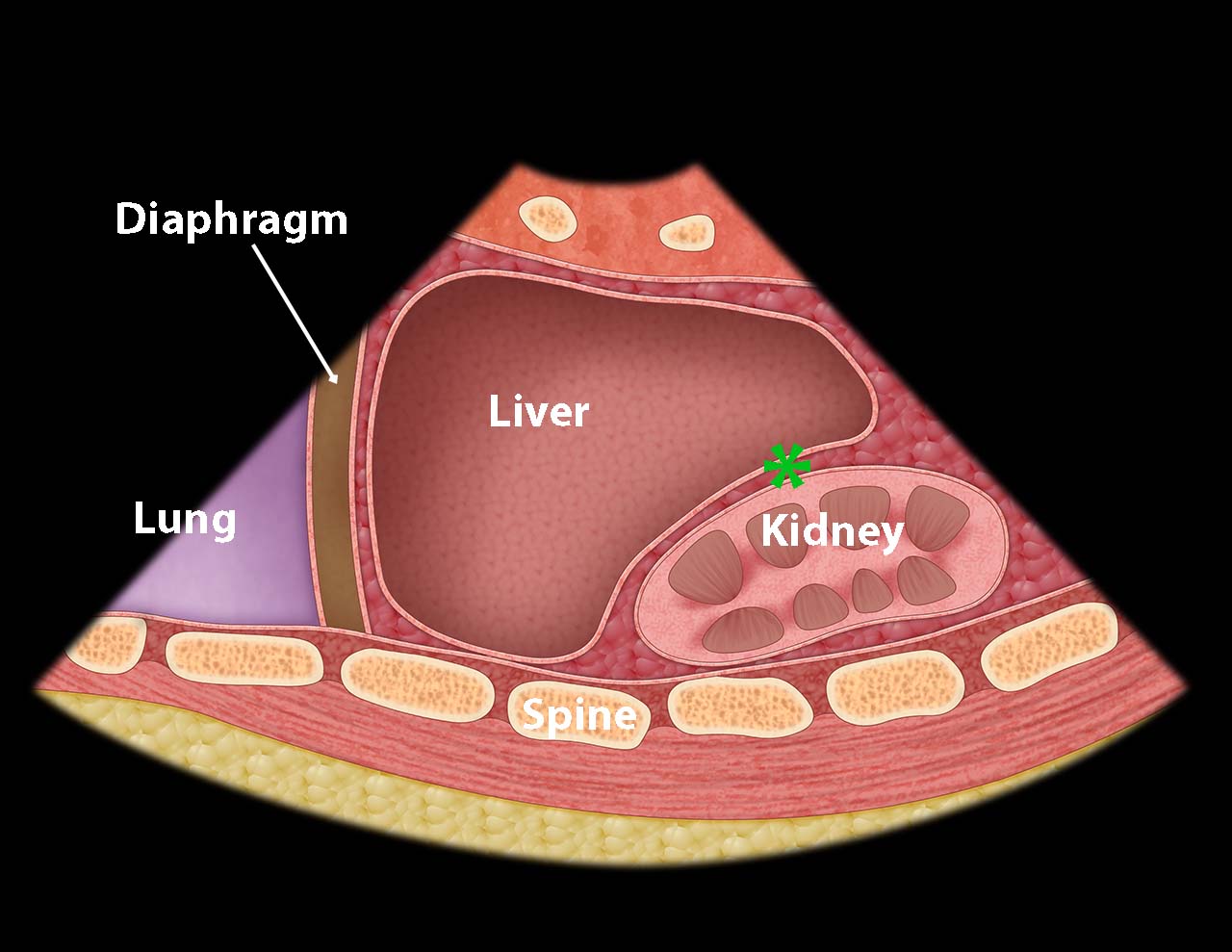
- Illustration 4. Morison’s pouch (asterisk)

- Figure 4. Probe position for right upper quadrant/Morison’s pouch
- This gives a coronal view of the interface between the liver and kidney. (Fig. 5) It is important to follow the lower edge of the liver caudally until a good view of the liver tip is obtained as fluid will often collect there first. (Video 4)
- Video 4. Morison’s pouch view
- Free fluid is usually seen in Morison’s pouch or along the lower edge of the liver and around the lower tip of the liver. (Figure 5, Videos 5-8)

- Figure 5. Small amount of free fluid Morison’s pouch view
- Video 5. Small amount of free fluid Morison’s pouch view
- Video 6. Small amount of free fluid Morison’s pouch view at the tip of the liver
- Video 7. Moderate amount of free fluid Morison’s pouch view
- Video 8. Large amount of free fluid Morison’s pouch view
- Rib shadows may be prominent when the marker-dot is pointed directly cephalad. Shadows can be minimized by rotating the probe slightly counter-clockwise, so the marker-dot is pointed toward the posterior axilla giving an intercostal oblique This will orient the footprint of the probe parallel to the ribs.
- Slide the probe cephalad to obtain a view of the diaphragm and look for pleural fluid. (Illustration 5, Fig. 10, Video 9)
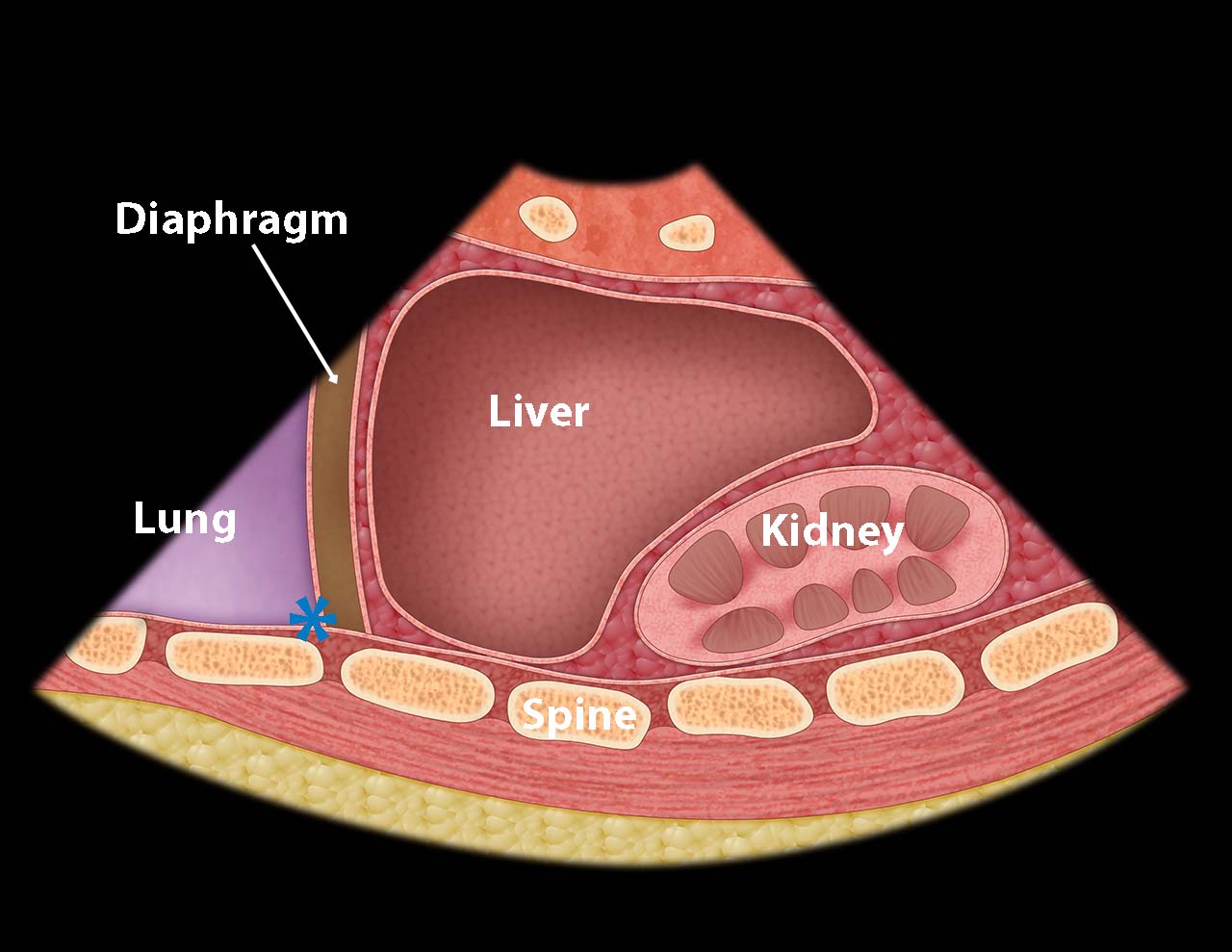
- Illustration 5. Base of right thoracic cavity where free fluid collects (asterisk)

- Figure 10. Probe position for right-sided pleural fluid evaluation
- Video 9. Normal view right pleura and lung from right upper quadrant
- Pleural fluid will appear as a jet black triangle just superior to the diaphragm. (Video 10) Also, this view may reveal free intraperitoneal fluid superior to the liver (Fig. 11)
- Pleural fluid will appear as a jet black triangle just superior to the diaphragm. (Video 10) Also, this view may reveal free intraperitoneal fluid superior to the liver (Fig. 11)
-
Video 10. Pleural fluid 
- Figure 11. Positive FAST scan with fluid in the abdomen superior to the liver
- Figure 12. Positive FAST scan with free fluid in the abdomen as well as pleural effusion
- Left Coronal and Intercostal Oblique Views:
- This is often the most difficult abdominal view to obtain. Place the probe in the posterior-axillary line at about the 6th to 9th intercostal space with the transducer indicator pointed cephalad, producing a coronal view. From this position the interface between the spleen and left kidney can be found.
- Free fluid is rarely seen between the spleen and the kidney but rather surrounding all other parts of the spleen or between spleen and diaphragm.
- To get rid of rib shadows, and to get a better view of the spleen, slide the probe cephalad and rotate it very slightly clockwise with the indicator pointing toward the posterior axilla, producing an intercostal oblique view, so that the spleen (not the kidney) is seen (Figure 13 shows the probe position). This view will allow good images of the lower tip and superior surface of the spleen, where intraperitoneal free fluid is most likely to collect. The diaphragm will also be seen in this view, just superior to the spleen.
- A pleural effusion will appear as a jet black stripe or triangle just superior to the diaphragm. (Video 10)
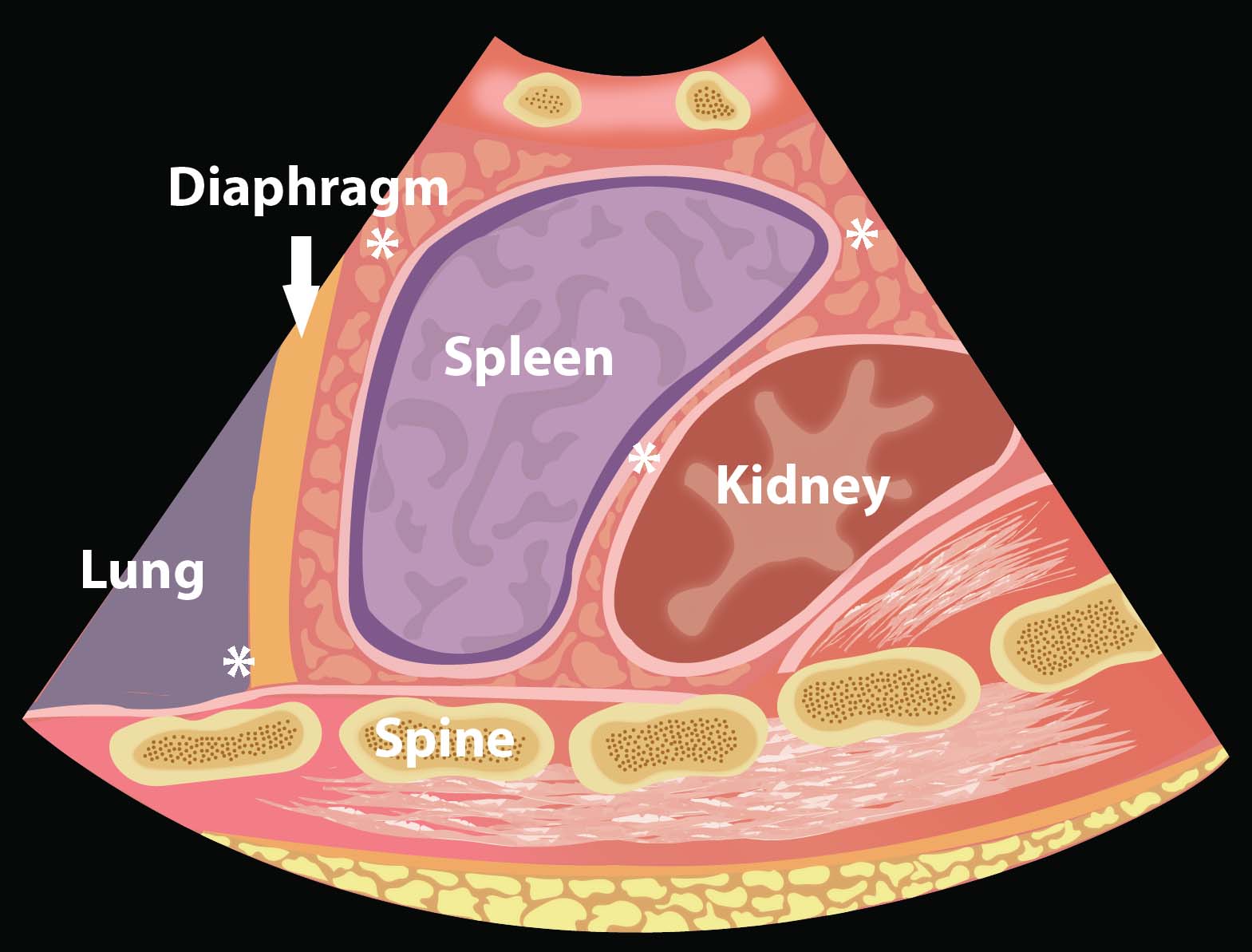
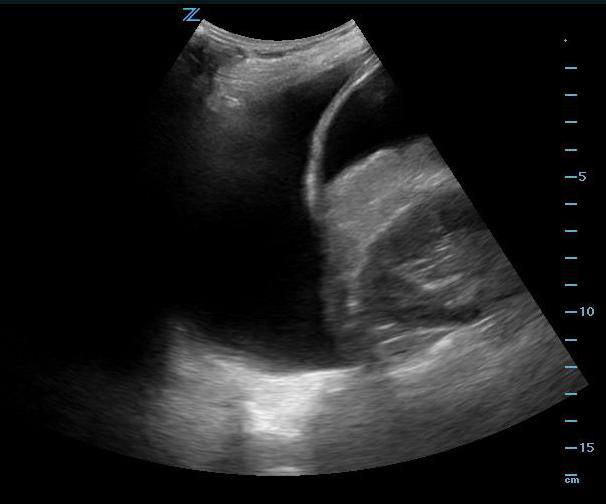
- Illustration 6. Left upper quadrant EFAST view demonstrating locations where intrathoracic free fluid (*) and intraabdominal free fluid collects (around spleen)

- Figure 13. Probe position for LUQ FAST view
- Video 11. Normal perisplenic view
- Video 12. Small amount of free fluid surrounding the spleen
- Video 13. Small amount of free fluid surrounding the spleen
- Video 14. Moderate amount of free fluid surrounding the spleen with pleural fluid visualized as well
- Video 15. Large amount of free fluid surrounding the spleen
- Anteriorly the stomach can cause air artifact and make visualization challenging so moving the probe posteriorly may be helpful. (Video 16) A full stomach can also give the appearance of fluid in the area. (Video 17)
-
Video 16. Air in stomach causing artifact in LUQ view
- Video 17. Full stomach seen in LUQ view
- Pelvic Views
- Pelvic views are not as easy to obtain as right upper quadrant views, but since the pelvis is the most dependent part of the peritoneal space, it is the most likely place to see abdominal free fluid.
- Place the probe in the midline just cephalad to the pubic bone with the transducer indicator pointed cephalad. Make sure the probe position is correct by actually placing the probe on the pubic bone and noting a bone shadow on the image. (Fig. 14) From this position sliding the probe slightly cephalad will produce a longitudinal pelvic view.

- Figure 14. Probe position for longitudinal view of the bladder
- The bladder will be found just cephalad to the pubic bone and can usually be found even if it is nearly empty. A full bladder will be triangular in shape. The lower angle of the bladder marks the border between the intraperitoneal space (left side of the image) and the true pelvic structures (right side of the image).
- In a male, free fluid will be seen along the inferior peritoneal cavity just posterior to the wall of the bladder.
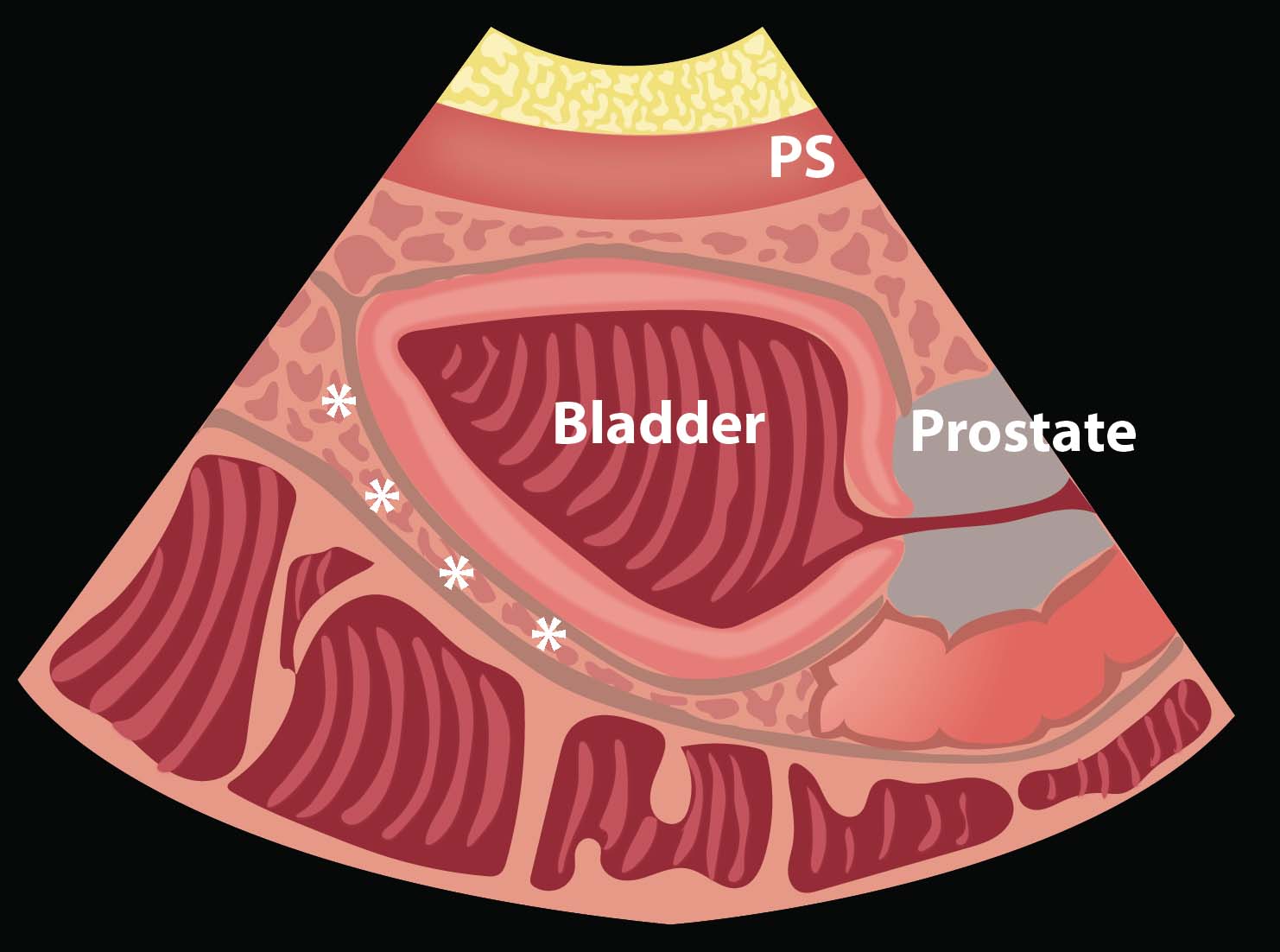
- Illustration 7. Potential spaces where free fluid may collect in the male pelvis (*)
- Video 18. Significant amount of free fluid posterior to the bladder
- In a female, the body of the uterus sits in the intraperitoneal space just posterior to the bladder (Video 19), so free fluid will be seen just posterior to the uterus, also known as the pouch of Douglas. A trace amount of free fluid can be normal in the pouch of Douglas depending on the woman’s menstrual cycle. Free fluid often is seen here first. (Video 20) Free fluid may also be seen completely surrounding the edges of the uterus. (Video 21) If there is clot in the pelvis, this will look grey compared with unclotted blood which will be black. (Video 22)
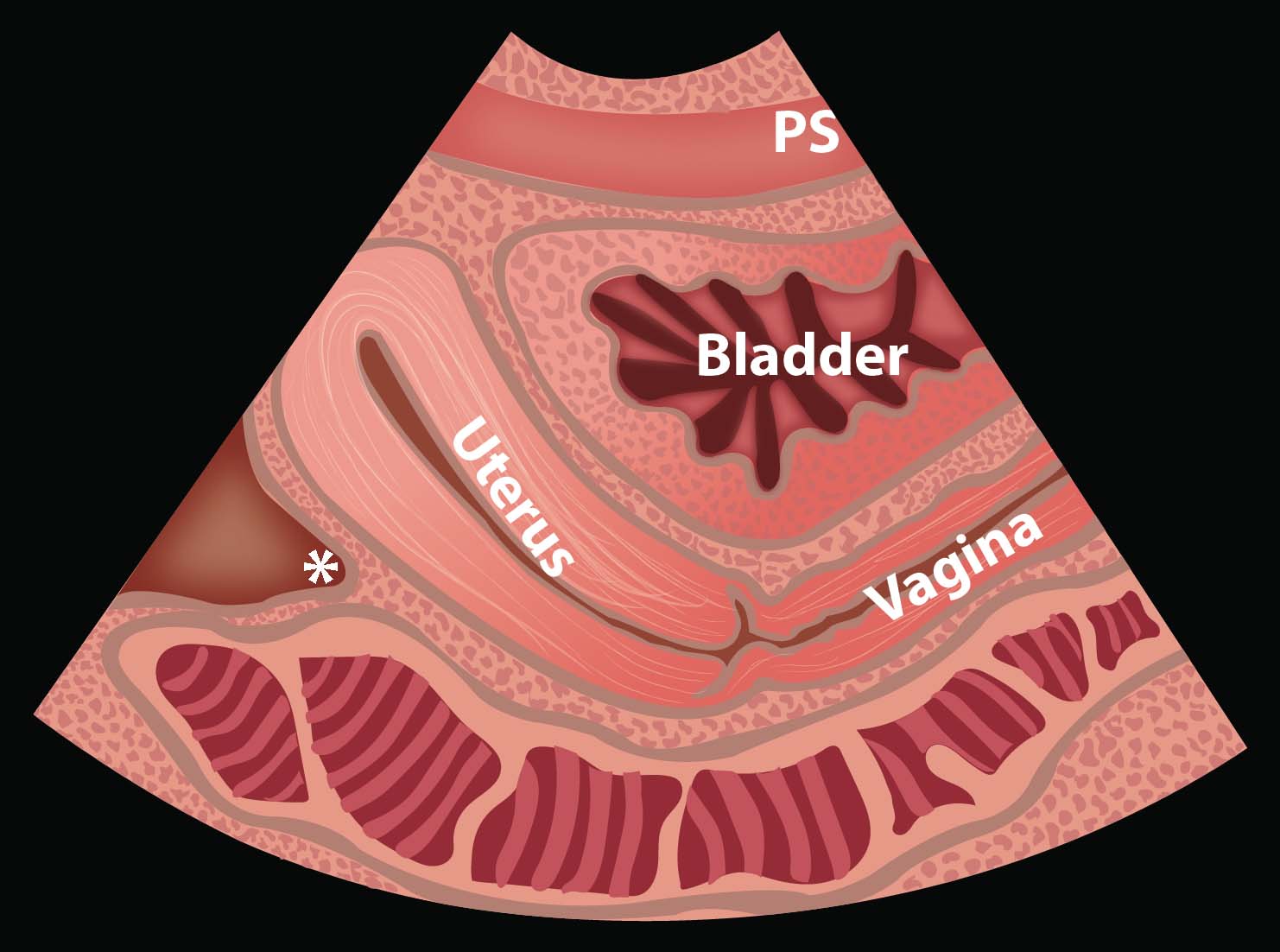
- Illustration 8. Pouch of Douglas in the female pelvis (*)
- Video 19. Normal longitudinal view of bladder and uterus
- Video 20. Moderate fluid in pouch of Douglas
- Video 21. Large amount of free fluid (black) surrounding the uterus
- Video 22. Large amount of free fluid (black) and clotted blood (grey) surrounding the uterus (Video courtesy of Gavin Budhram, MD)
- If the bladder is empty, it is very difficult to recognize pelvic free fluid in a male. In a female, the pouch of Douglas may still be identifiable, even when the bladder is empty.
- To obtain transverse views, simply rotate the probe 90 degrees, pointing the probe marker to the patients' right side. (Fig. 15) In transverse pelvic views, free fluid may be seen posterior to the bladder or uterus, or adjacent to the corners of the full bladder. (Fig. 23)

- Figure 15. Probe position for transverse pelvic view
- Video 23. Small amount of free fluid posterior to the bladder in a male
- Anterior Thoracic Views:
- When using ultrasound to evaluate for a pneumothorax, the probe is usually placed on the anterior chest in the 2nd-4th intercostal space and midclavicular line. This is a starting point and a likely place to find a pneumothorax when the patient is in the supine position. Subsequent imaging can be done on any part of the chest wall if there is concern for a very small or loculated pneumothorax.

- Figure 16. Probe position for anterior thoracic view
- A high frequency vascular/small parts probe (known as a linear probe) can be used for this exam, but a standard curvilinear abdominal or phased array probe will also work well. The most important part about this exam is decreasing the depth setting so that the ultrasound image shows a maximum depth of about 4-6 cm.
- The probe is placed in a longitudinal position with the transducer indicator pointed cephalad. In this orientation, rib shadows can be used to find the pleural plane.
- Between the ribs, the pleural interface will be apparent at the posterior border of the ribs. It is important to anchor the probe and hold it very still while looking for the sliding motion of the visceral pleura against the parietal pleura. (Video 24)
- If the “sliding sign” is not present, a pneumothorax is suspected. (Video 25) Comparing one side of the chest to the other may be helpful.
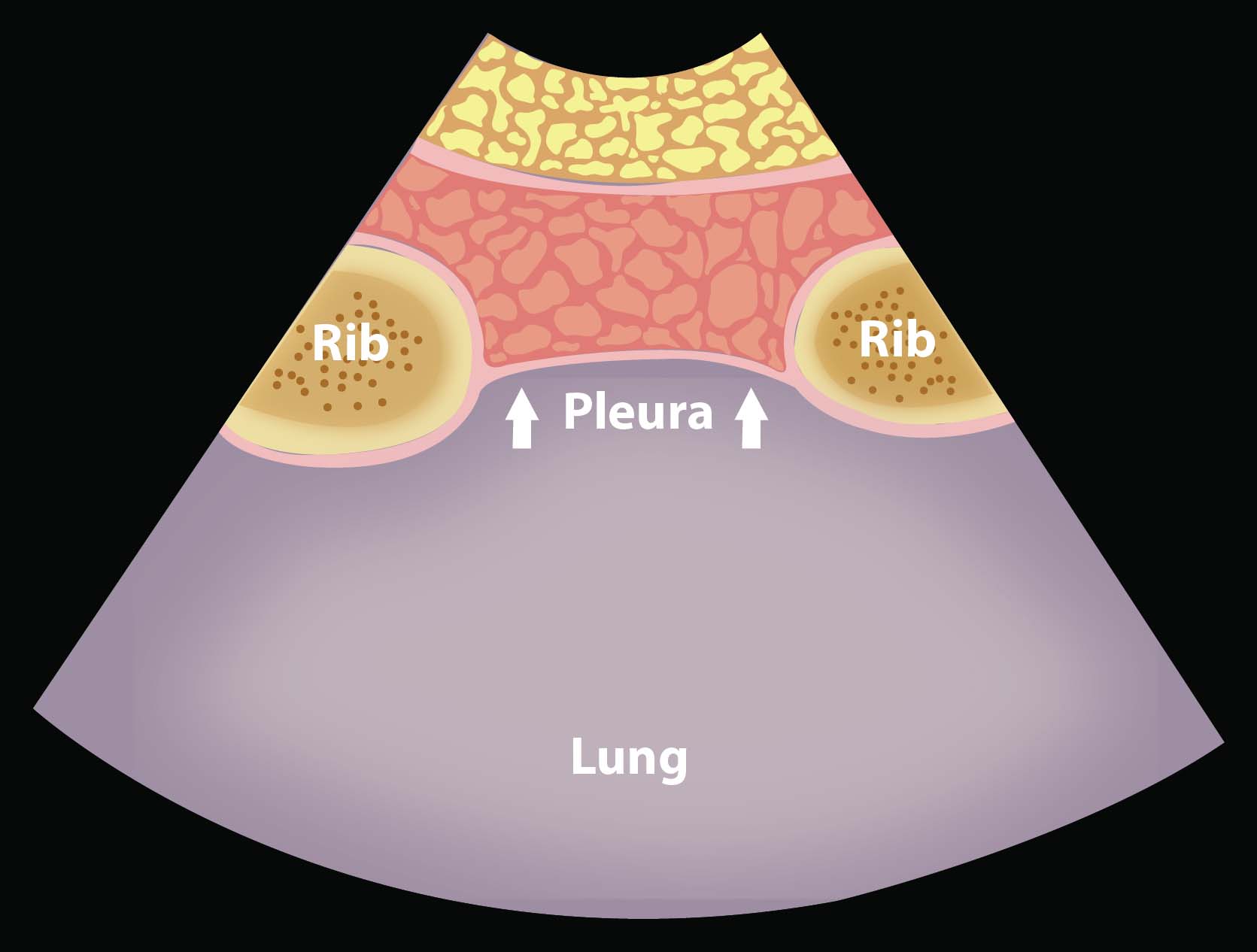
- Illustration 9. Normal anatomy at the anterior thoracic view
- Video 24. Normal “lung sliding”
- Video 25. Absence of lung sliding representative of a pneumothorax
- When using ultrasound to evaluate for a pneumothorax, the probe is usually placed on the anterior chest in the 2nd-4th intercostal space and midclavicular line. This is a starting point and a likely place to find a pneumothorax when the patient is in the supine position. Subsequent imaging can be done on any part of the chest wall if there is concern for a very small or loculated pneumothorax.
VII. Pearls and Pitfalls
- If the initial FAST exam is negative and clinical suspicion remains high, consider a repeat FAST exam after a short time period.
- Trendelenburg position may be required to visualize free fluid during perihepatic and peri-splenic examination.
- Consider reverse Trendelenburg position while evaluating for hemothorax or pelvic free fluid.
- It is important to visualize as much perihepatic and peri-splenic area as possible, not just one quick view. Multiple windows may be required to fully evaluate for free fluid.
- If visualization of the peri-splenic view is inadequate, moving the probe caudad and posterior may improve the window.
- Subcutaneous emphysema may obscure visualization of underlying structures.
- Pericardial anechoic or hypoechoic stripes that are circumferential usually represent pericardial fluid, whereas a focal anterior hypoechoic region may be normal pericardial fat. Pericardial fat with appear to move with the heart as it adheres to the heart as opposed to moving independently
- Video 26. Pericardial fat
- A focal posterior effusion seen on the parasternal long axis view, may be a left pleural effusion rather than a pericardial effusion. The hypoechoic stripe of a pericardial effusion usually wraps around the apex of the heart and stays superficial to the descending thoracic aorta seen just deep to the heart on this view. A pleural effusion stays to the right of the descending thoracic aorta on the screen and often deep to the level of the aorta.
- Video 27. Pleural effusion seen on the parasternal long view
- Perinephric fat, especially in obese patients, may be misinterpreted as intraperitoneal free fluid. Consider comparison views between each kidney.
- Free fluid isn’t always blood; consider ascites, fluid related to a ruptured ovarian cyst, ruptured bladder or peritoneal dialysis.
- Not all abdominal injuries produce free fluid. Bowel injury and solid organ injury without significant bleeding will not be detected by ultrasound.
- Clotted blood can generate various degrees of echogenicity and may be mistaken for normal surrounding soft tissue.
- The pelvic view should be completed prior to placement of a Foley catheter.
- Chest ultrasound can only detect a pneumothorax which is directly under the probe, so consider looking in several sites on the anterior chest is suspicion is high.
- Lack of pleural sliding may indicate a pneumothorax, mainstem intubation, blebs or just poor ventilation/apnea.
- Comparing one side of the chest to the other is helpful but may be confusing if bilateral pneumothoraces are present.
- Lung sliding will be better visualized if the ultrasound beam is angled medially to be perpendicular to the true thoracic cavity (and not the skin) in cases of significant obesity.
- Dimming the lights in the exam room may provide the examiner with an improved display of ultrasound findings.
VIII. References
- Tiling T, Bouillon B, Schmid A. Ultrasound in blunt abdomino-thoracic Trauma. in: Border J, Allgoewer M, Hansen S (eds.), Blunt Multiple Trauma: Comprehensive Pathophysiology and Care. Marcel Dekker: New York,1990;415-433.
- Plummer D. Principles of emergency ultrasound and echocardiography. Ann Emerg Med.1989;18:1291-7.
- Jehle D, Davis E, Evans T, et al. Emergency department sonography by emergency physicians. Am J Emerg Med.1989;7:605-11.
- Scalea TM, Rodriguez A, Chiu WC, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466-72.
- Rozycki GS, Shackford SR. Ultrasound, what every trauma surgeon should know. J Trauma. 1996;40:1-4.
- Rozycki GS, Ballard RB, Feliciano DV, et al. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998;228:557-67.
- Wherrett LJ, Boulanger BR, McLellan BA, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma. 1996;41:815-20.
- Rozycki GS, Feliciano DV, Ochsner MG, et al. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma. 1999;46:543-52.
- Plummer D, Brunette D, Asinger R, et al. Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992;21:709-12.
- Dulchavsky SA, Schwarz KL, Kirkpatrick AW, et al. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma. 2001;50:201-5.
- Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma. 2004;57:288-95.
- Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997;29:312-6.
- Sisley AC, Rozycki GS, Ballard RB, et al. Rapid detection of traumatic effusion using surgeon-performed ultrasonography. J Trauma. 1998;44: 291-7.
- Reardon R, Moscati R. Beyond the FAST Exam: Additional Applications of Sonography in Trauma. in: Jehle D, Heller M (eds.) Ultrasonography in Trauma: The FAST Exam, American College of Emergency Physicians: Dallas, TX. 2003;107-126.
- Moscati R, Reardon R. Clinical Application of the FAST Exam. in: Jehle D, Heller M (eds.) Ultrasonography in Trauma: The FAST. American College of Emergency Physicians: Dallas, TX. 2003;39-60.
- Mandavia D, Kendall J. Pitfalls in Trauma Ultrasonography. in: Jehle D, Heller M (eds.), Ultrasonography in Trauma: The FAST Exam. American College of Emergency Physicians: Dallas, TX. 2003;87-105.
- Schiavone WA, Ghumrawi BK, Catalano DR, et al. The use of echocardiography in the emergency management of nonpenetrating traumatic cardiac rupture. Ann Emerg Med. 1991;20:1248-50.
- Laselle BT, Byyny RL, Haukoos JS, et al. False Negative FAST examination: associations with injury characteristics and patient outcomes. Ann Emerg Med. 2012;60(3):326-34.
- Neal MD, Peitzman AB, Forsythe RM, et al. Over reliance on computed tomography in patients with severe abdominal injury: is the delay worth the risk? J Trauma. 2011;70:278-84.
- Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: current perspectives. Open Access Emerg Med. 2017;9:57-62.
- Soffer D, McKenney MG, Cohn S, et al. A prospective evaluation of ultrasonography for the diagnosis of penetrating torso injury. J Trauma. 2004;56:953-9.
- Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879-85.
- Rozycki GS, Ochsner MG, Schmidt JA, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995;39:492-500.
- Boulanger BR, Kearney PA, Tsuei B, et al. The routine use of sonography in penetrating torso injury is beneficial. J Trauma. 2001;51:320-5.
- Tayal VS, Beatty MA, Marx JA, et al. FAST (focused assessment with sonography in trauma) accurate for cardiac and intraperitoneal injury in penetrating anterior chest trauma. J Ultrasound Med. 2004;23:467-72.
- Juhl J. Diseases of the pleura, mediastinum, and diaphragm., in: Juhl J, Crummy A (eds.), Essentials of Radiologic Imaging. JB Lippincott: Philadelphia, PA. 1993;1026.
- Rothlin MA, Naf R, Amgwerd M, et al. Ultrasound in blunt abdominal and thoracic trauma. J Trauma. 1993;34:488-95.
- Ma OJ, Mateer. Trauma, in: Ma OJ, Mateer J (eds.), Emergency Ultrasound, McGraw-Hill: New York. 2003;67-88.
- Ball CG, Kirkpatrick AW, Laupland KB, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. Am J Surg. 2005;189:550-6.
- Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. 1995;108:1345-8.
- Lichtenstein D, Goldstein I, Mourgeon E, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. 2004;100:9-15.
- Lichtenstein D, Meziere G, Lascols N, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231-8.
- Ma OJ, Kefer MP, Mateer JR, et al. Evaluation of hemoperitoneum using a single- vs multiple-view ultrasonographic examination. Acad Emerg Med. 1995;2:581-6.
- Carter JW, Falco MH, Chopko MS, et al. Do we really rely on fast for decision-making in the management of blunt abdominal trauma? Injury. 2014;46(5):817-21.
- Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003;21:476-8.
- Abrams BJ, Sukumvanich P, Seibel R, et al. Ultrasound for the detection of intraperitoneal fluid: the role of Trendelenburg positioning. Am J Emerg Med. 1999;17:117-20.