
From MIPS to MVP and Beyond...
Background:
The Centers for Medicare & Medicaid Services (CMS) invited interested stakeholders to develop and submit Merit-based Incentive Payment System (MIPS) Value Pathways (MVP) candidates for evaluation and potential proposal in future rulemaking.
With MVPs, CMS is aiming to reduce the burden and complexity associated with selecting from a large inventory of quality measures, improvement activities, and cost measures.
As noted in the CY 2021 Physician Fee Schedule Final Rule, the MVP framework strives to link measures and improvement activities that address a common clinical theme across the four MIPS performance categories. More details regarding the intent of the MVP framework and the latest 2021 Final Rule Fact Sheet can be accessed on the MVP website.
MVP candidates needed to include measures and activities from across the Quality, Cost, and Improvement Activities performance categories. Furthermore, the foundational layer of each MVP candidate was also required to include the entire set of Promoting Interoperability measures and the Hospital-Wide 30-Day All-Cause Unplanned Readmission (HWR) Measure.
Quality Category:
CMS encouraged submissions to include measures and improvement activities that are currently available in MIPS. The MIPS quality measures are mapped to 46 specialties and sub-specialties that provided guidance for stakeholders developing MVP candidates based on specialties.
Stakeholders could also submit MVP candidates based on a health condition (e.g. diabetes). In instances where a quality measure closely related to the MVP candidate topic was not available, a broadly applicable or cross-cutting measure that drives quality care in alignment with the MVP topic could suffice.
The MIPS quality measures are also categorized by measure type, and are categorized as such, in the MIPS quality measures list (see above link). CMS encourages the inclusion of measures that fall into the Outcome, Patient Reported Outcome, and Patient Engagement/Experience measure types to the extent feasible. As there may be limited availability of Patient Reported Outcome Measures for all specialties, we encourage the use of other measures that consider the patient in MVPs, such as patient surveys, patient satisfaction, patient experience, or patient safety measures.
Qualified Clinical Data Registry (QDCR) measures may also be considered for inclusion in an MVP so long as the measure has met all requirements, including being fully tested and approved through the Self-Nomination process.
Measures that are currently outside the MIPS program need to follow the pre-rulemaking process (e.g., Call for Measures and rulemaking) before they may be included in an MVP.
Improvement Activities:
Improvement activities are broader in application and cover a wide range of clinician types and health conditions. Improvement activities that best drive the quality of care addressed in the MVP topic could be prioritized. Improvement activities should complement and/or supplement the quality action of the measures in the MVP candidate submission, rather than duplicate it.
Cost Measures:
The current inventory of cost measures covers different types of care. Procedural episode-based cost measures apply to specialties (such as orthopedic surgeons) that perform procedures of a defined purpose or type, and acute episode-based cost measures cover clinicians (such as hospitalists) who provide care for specific acute inpatient conditions. There are also two broader types of measures (population-based cost measures) that assess overall costs of care for a patient’s admission to an inpatient hospital (MSPB Clinician measure) and for primary care services that a patient receives (TPCC measure). In addition, the MIPS cost measures are calculated for clinicians and clinician groups based on administrative claims data.
What Did ACEP Do?
Last month, ACEP submitted a proposal to the Centers for Medicare & Medicaid Services (CMS) for an emergency medicine-focused Merit-based Incentive Payment System (MIPS) Value Pathway (MVP). This submission represents another step in ACEP’s long-term effort to help transition emergency physicians to value-based care models.
So, what is an MVP? When I first heard the acronym, I thought CMS was in some way making an artful analogy to a sports super star! Well, in actuality, it is a new framework for participating in MIPS—the major quality performance program for physicians in Medicare. Under the current MIPS program, clinicians must report or attest to measures in four performance categories—Quality, Cost, Improvement Activities, and Promoting Interoperability (formerly known as Meaningful Use). Performance in these four categories (which are weighted) roll up into an overall score that translates to an upward, downward, or neutral payment adjustment that clinicians receive two years after the performance period (for example, performance in 2021 will impact Medicare payments in 2023).
Most emergency physicians need to participate in MIPS to avoid a penalty and perhaps receive a bonus. While the bar for avoiding a penalty is continually being raised, one consistent element of the program’s design has been that clinicians have always had a lot of choices of what measures to report. For example, for the Quality performance category, clinicians generally must report on six measures out of more than 200 possible options—and they can switch which measures they report on each year. Given the lack of consistency in reporting, some key stakeholders, including MedPAC (an independent commission tasked with providing Medicare-related policy recommendations to CMS and Congress) believe that clinicians may even have too many choices and that MIPS needs to adjusted (or as MedPAC suggests, totally transformed) to make it more meaningful to clinicians and to really improve quality of care.
MVPs represent CMS’ solution to this issue. They are streamlined reporting options in which measures across the Quality, Cost, and Improvement Activities categories of MIPS are grouped together around an episode of care, condition, or specialty (the Promoting Interoperability category requirements would remain the same). By grouping together measures in a meaningful way, CMS hopes that MVPs can not only help drive more quality improvement, but also give clinicians more experience focusing on ways to contain costs—an essential skill to have to be able to successfully participate in an APM. Thus, CMS’ ultimate goal is to have all clinicians participate in MVPs and eventually in APMs.
CMS doesn’t expect this significant transition from MIPS to MVPs to APms to happen overnight. In fact, CMS’ initial timeline for implementing the first set of MVPs has been delayed from 2021 to 2022 due to the COVID-19 pandemic. CMS expects to have a few MVPs operational in 2022 and then add more each year thereafter. With respect to the process for developing new MVPs, CMS is relying on outside stakeholders (like ACEP) to submit MVP concepts. Once submitted, CMS will go back and forth with the submitter on the proposal and may make changes to specific measures or other features of the MVP. After these initial conversations, CMS will take ownership of the MVP and decide whether to propose it in the annual Physician Fee Schedule (PFS) and Quality Payment Program (QPP) proposed regulation. If CMS does decide to propose the MVP concept, like any other proposal in this annual reg, the public will have a chance to comment on it and then CMS will ultimately decide whether to finalize the MVP in the final regulation.
Review Process:
On an annual basis, CMS intends to host a public-facing MVP development webinar to remind stakeholders of MVP development criteria as well as the timeline and process to submit a candidate MVP. While CMS believes that engagement with stakeholders regarding MVP candidates may occur on a rolling basis throughout the year, at CMS’s discretion the agency will determine if an MVP is ready for inclusion in the upcoming performance period.
As MVP candidates are received, they will be reviewed, vetted, and evaluated by CMS and their contractors. CMS intends on utilizing the MVP development criteria to determine if the candidate MVP is feasible. In addition to the MVP development criteria, CMS will also vet the quality and cost measures from a technical perspective to validate that the coding in the quality measures and cost measure(s) include the clinician type being measured and whether all potential specialty-specific quality measures or cost measures were considered, with the most appropriate included.
CMS may reach out to stakeholders on an as-needed basis, should questions arise during the review process. To continue collaborative efforts, once an internal evaluation is completed, CMS will reach out to select stakeholders whose candidate MVP may be feasible for the upcoming performance period to schedule a meeting to have an iterative dialog regarding our feedback and next steps that may include recommended modifications to the MVP candidate. Submitting an MVP candidate does not guarantee it will be accepted for the rulemaking process. To ensure a fair and transparent rulemaking process, CMS will not be able to directly communicate (to those who submit MVP candidates) whether an MVP candidate has been approved, disapproved, or is being considered for a future year, prior to the publication of the proposed rule.
MVP Development Process for 2022
From MIPS to MVP and Beyond…
The Centers for Medicare & Medicaid Services (CMS) invited interested stakeholders to develop and submit Merit-based Incentive Payment System (MIPS) Value Pathways (MVP) candidates for evaluation and potential proposal in future rulemaking.
With MVPs, CMS is aiming to reduce the burden and complexity associated with selecting from a large inventory of quality measures, improvement activities, and cost measures.
As noted in the CY 2021 Physician Fee Schedule Final Rule, the MVP framework strives to link measures and improvement activities that address a common clinical theme across the four MIPS performance categories. More details regarding the intent of the MVP framework and the latest 2021 Final Rule Fact Sheet can be accessed on the MVP website.
MVP candidates needed to include measures and activities from across the Quality, Cost, and Improvement Activities performance categories. Furthermore, the foundational layer of each MVP candidate was also required to include the entire set of Promoting Interoperability measures and the Hospital-Wide 30-Day All-Cause Unplanned Readmission (HWR) Measure.
Quality Category:
CMS encouraged submissions to include measures and improvement activities that are currently available in MIPS. The MIPS quality measures are mapped to 46 specialties and sub-specialties that provided guidance for stakeholders developing MVP candidates based on specialties.
Stakeholders could also submit MVP candidates based on a health condition (e.g. diabetes). In instances where a quality measure closely related to the MVP candidate topic was not available, a broadly applicable or cross-cutting measure that drives quality care in alignment with the MVP topic could suffice.
The MIPS quality measures are also categorized by measure type, and are categorized as such, in the MIPS quality measures list (see above link). CMS encourages the inclusion of measures that fall into the Outcome, Patient Reported Outcome, and Patient Engagement/Experience measure types to the extent feasible. As there may be limited availability of Patient Reported Outcome Measures for all specialties, we encourage the use of other measures that consider the patient in MVPs, such as patient surveys, patient satisfaction, patient experience, or patient safety measures.
Qualified Clinical Data Registry (QDCR) measures may also be considered for inclusion in an MVP so long as the measure has met all requirements, including being fully tested and approved through the Self-Nomination process.
Measures that are currently outside the MIPS program need to follow the pre-rulemaking process (e.g., Call for Measures and rulemaking) before they may be included in an MVP.
Improvement Activities:
Improvement activities are broader in application and cover a wide range of clinician types and health conditions. Improvement activities that best drive the quality of care addressed in the MVP topic could be prioritized. Improvement activities should complement and/or supplement the quality action of the measures in the MVP candidate submission, rather than duplicate it.
Cost Measures:
The current inventory of cost measures covers different types of care. Procedural episode-based cost measures apply to specialties (such as orthopedic surgeons) that perform procedures of a defined purpose or type, and acute episode-based cost measures cover clinicians (such as hospitalists) who provide care for specific acute inpatient conditions. There are also two broader types of measures (population-based cost measures) that assess overall costs of care for a patient’s admission to an inpatient hospital (MSPB Clinician measure) and for primary care services that a patient receives (TPCC measure). In addition, the MIPS cost measures are calculated for clinicians and clinician groups based on administrative claims data.
What Did ACEP Do?
Last month, ACEP submitted a proposal to the Centers for Medicare & Medicaid Services (CMS) for an emergency medicine-focused Merit-based Incentive Payment System (MIPS) Value Pathway (MVP). This submission represents another step in ACEP’s long-term effort to help transition emergency physicians to value-based care models.
So, what is an MVP? When I first heard the acronym, I thought CMS was in some way making an artful analogy to a sports super star! Well, in actuality, it is a new framework for participating in MIPS—the major quality performance program for physicians in Medicare. Under the current MIPS program, clinicians must report or attest to measures in four performance categories—Quality, Cost, Improvement Activities, and Promoting Interoperability (formerly known as Meaningful Use). Performance in these four categories (which are weighted) roll up into an overall score that translates to an upward, downward, or neutral payment adjustment that clinicians receive two years after the performance period (for example, performance in 2021 will impact Medicare payments in 2023).
Most emergency physicians need to participate in MIPS to avoid a penalty and perhaps receive a bonus. While the bar for avoiding a penalty is continually being raised, one consistent element of the program’s design has been that clinicians have always had a lot of choices of what measures to report. For example, for the Quality performance category, clinicians generally must report on six measures out of more than 200 possible options—and they can switch which measures they report on each year. Given the lack of consistency in reporting, some key stakeholders, including MedPAC (an independent commission tasked with providing Medicare-related policy recommendations to CMS and Congress) believe that clinicians may even have too many choices and that MIPS needs to adjusted (or as MedPAC suggests, totally transformed) to make it more meaningful to clinicians and to really improve quality of care.
MVPs represent CMS’ solution to this issue. They are streamlined reporting options in which measures across the Quality, Cost, and Improvement Activities categories of MIPS are grouped together around an episode of care, condition, or specialty (the Promoting Interoperability category requirements would remain the same). By grouping together measures in a meaningful way, CMS hopes that MVPs can not only help drive more quality improvement, but also give clinicians more experience focusing on ways to contain costs—an essential skill to have to be able to successfully participate in an APM. Thus, CMS’ ultimate goal is to have all clinicians participate in MVPs and eventually in APMs.
CMS doesn’t expect this significant transition from MIPS to MVPs to APms to happen overnight. In fact, CMS’ initial timeline for implementing the first set of MVPs has been delayed from 2021 to 2022 due to the COVID-19 pandemic. CMS expects to have a few MVPs operational in 2022 and then add more each year thereafter. With respect to the process for developing new MVPs, CMS is relying on outside stakeholders (like ACEP) to submit MVP concepts. Once submitted, CMS will go back and forth with the submitter on the proposal and may make changes to specific measures or other features of the MVP. After these initial conversations, CMS will take ownership of the MVP and decide whether to propose it in the annual Physician Fee Schedule (PFS) and Quality Payment Program (QPP) proposed regulation. If CMS does decide to propose the MVP concept, like any other proposal in this annual reg, the public will have a chance to comment on it and then CMS will ultimately decide whether to finalize the MVP in the final regulation.
Review Process:
On an annual basis, CMS intends to host a public-facing MVP development webinar to remind stakeholders of MVP development criteria as well as the timeline and process to submit a candidate MVP. While CMS believes that engagement with stakeholders regarding MVP candidates may occur on a rolling basis throughout the year, at CMS’s discretion the agency will determine if an MVP is ready for inclusion in the upcoming performance period.
As MVP candidates are received, they will be reviewed, vetted, and evaluated by CMS and their contractors. CMS intends on utilizing the MVP development criteria to determine if the candidate MVP is feasible. In addition to the MVP development criteria, CMS will also vet the quality and cost measures from a technical perspective to validate that the coding in the quality measures and cost measure(s) include the clinician type being measured and whether all potential specialty-specific quality measures or cost measures were considered, with the most appropriate included.
CMS may reach out to stakeholders on an as-needed basis, should questions arise during the review process. To continue collaborative efforts, once an internal evaluation is completed, CMS will reach out to select stakeholders whose candidate MVP may be feasible for the upcoming performance period to schedule a meeting to have an iterative dialog regarding our feedback and next steps that may include recommended modifications to the MVP candidate. Submitting an MVP candidate does not guarantee it will be accepted for the rulemaking process. To ensure a fair and transparent rulemaking process, CMS will not be able to directly communicate (to those who submit MVP candidates) whether an MVP candidate has been approved, disapproved, or is being considered for a future year, prior to the publication of the proposed rule.
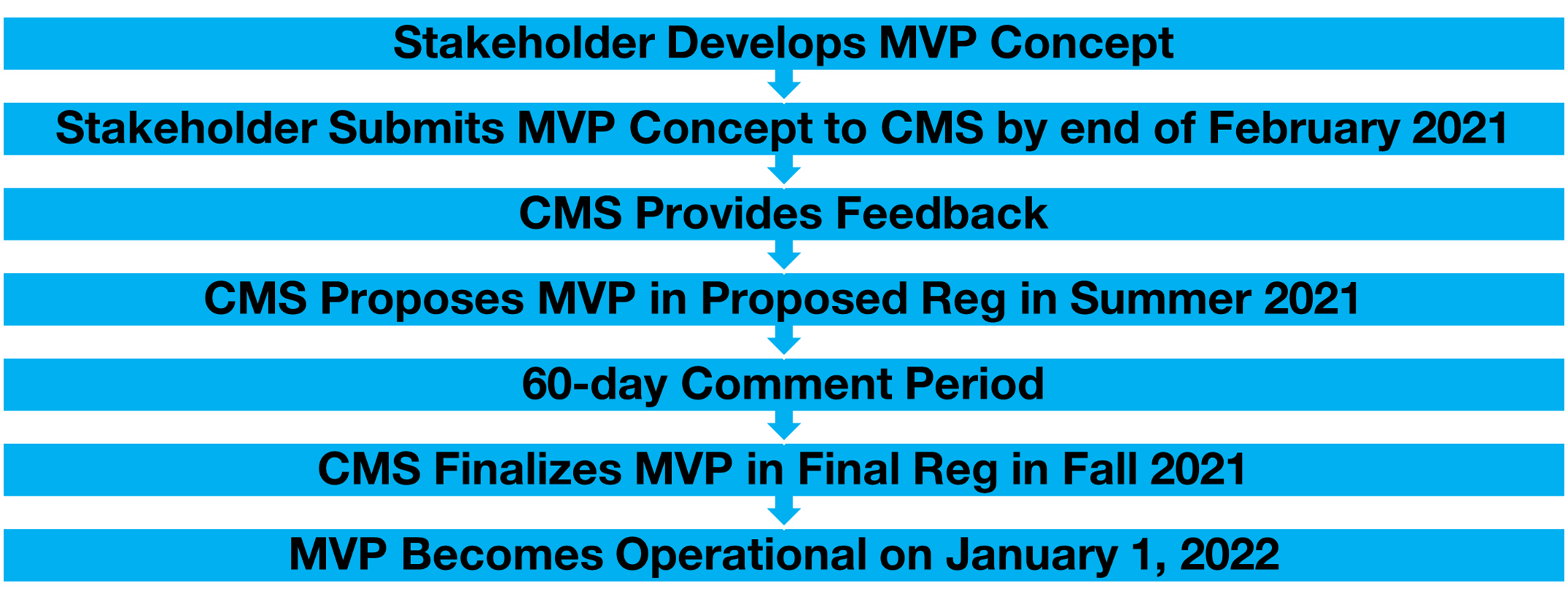
Thus, as you can see, there are many steps that an MVP concept must go through before it actually becomes a full-fledged MVP—and there is no guarantee that every MVP concept will make it through each step along the journey. Even with this uncertainty, ACEP feels that it is critical to submit a proposal in time for CMS to consider it for the 2022 PFS and QPP proposed reg. As one of the leading voices in emergency medicine, ACEP is in a prime position to propose an MVP that is the most meaningful to you as emergency physicians—and one that truly reflects the unique nature of emergency medicine. What we want to avoid is a situation where an emergency medicine MVP in-name-only is implemented. Going forward with an MVP that is not meaningful to emergency physicians (such as one that measures care processes that emergency physicians do not exert much control over) would waste a great opportunity to engage you in more value-based care efforts and help you all focus on improving on areas that have the greatest impact on the quality and cost of the care you provide.
ACEP certainly had no time to dilly-dally if we wanted to meet the deadline for submitting MVP proposals for 2022. CMS finalized all the guidance for MVP submissions in December of last year (and hosted some webinars that clarified the guidance earlier this year)—and proposals are due at the end of this week. Despite the compressed timeline, I am proud to say that ACEP underwent a robust process to develop an MVP proposal. First, ACEP’s President, Dr. Mark Rosenberg, convened an MVP Task Force (led by Dr. Cameron Gettel) that included experts from across the country on MIPS, quality measurement, and value-based care. To inform the Task Force’s work on an MVP, it sent out a survey to all the relevant ACEP committees, sections, and to outside stakeholders such as patient representatives to get their input on what quality measures and activities were truly meaningful to you as emergency physicians and the patients you serve. There were approximately 120 responses to the survey, giving the Task Force the clear direction it needed to construct a solid MVP proposal.
While obviously subject to change throughout the long development process described above, ACEP’s initial MVP proposal focuses on undifferentiated high-risk conditions. Quality category measures within the proposed MVP address chest pain, abdominal pain, headache, and back pain—all common conditions that are seen on a daily basis. Importantly, emergency department (ED) disposition decisions for these conditions have considerable influence on healthcare quality and cost, as we have found that there is significant variation in admission rates for all the conditions and variation in opioid prescribing and imaging utilization rates with respect to atraumatic back pain and headache. The proposal also includes associated and assorted number of measures and activities within the Improvement Activities category that are frequently reported, clinically appropriate, and relevant to emergency physicians.
The Cost and Promoting Interoperability performance categories are not so straightforward when it comes to emergency medicine. With respect to Cost, there are no episode-based cost measures that are currently attributable to emergency physicians. In addition, the standard MIPS cost measures, the Medicare Spending Per Beneficiary (MSPB) measure, and the Total Per Capita Cost (TPCC) measure do not appropriately capture the cost of emergency care. Since including cost measures in an MVP proposal is a requirement, we do propose to include both the MSPB and TPCC within the Cost performance category but leave to door open to including other cost measures in the MVP as future measures become available. On that note, a few weeks ago, ACEP submitted comments to CMS’ contractor, Acumen, about the future development of emergency medicine-specific episode-based cost measures and we are hopeful that new measures will become available in the next few years.
Moving on to the Promoting Interoperability Category, it is important to note that most of you as emergency physicians are exempt from this category since you are deemed “hospital-based” and do not have as much control over the use of your health information technology systems as office-based clinicians do. While we do include the Promoting Interoperability standard measure set in the MVP proposal (which is required), we don’t expect emergency physicians who select to report through the MVP to actually have to meet the Promoting Interoperability category requirements.
Finally, as initially designed, the MVP will still include some choices for emergency physicians. We are proposing that emergency physicians report on 4 out of a total of 10 available quality measures and 2 out of a total of 8 improvement activities.
Overall, we believe that this proposal accomplishes the major goal of an MVP—to focus on areas where there is a clear opportunity for care improvement. Further, it may achieve another major goal of helping emergency physicians participate in APMs. The common conditions that the MVP focuses on overlap with those that are included in ACEP’s APM, the AUCM. We are still waiting on CMS to adopt the AUCM, and hopefully, if the MVP is adopted in the meantime, CMS will see enough value in targeting these conditions that it will eventually transition the MVP to an APM like the AUCM.
We are excited about this opportunity to engage with CMS on our MVP proposal and look forward to seeing where the proposal goes from here. I will keep you updated as the proposal makes it way along the long journey towards implementation and hope that you all will find that the final emergency medicine-focused MVP, if implemented, actually does achieve the ambitious goals that we have laid out for it.
Until next week, this is Pawan saying, enjoy reading the newsletter from quality.
Pawan Goyal, MD, MHA, PMP, MS, FHIMSS, CPHIMS
Associate Executive Director, Quality
American College of Emergency Physicians



