Updates on the 2024 Medicare Physician Final Rule for ED Related Codes

David A. McKenzie, CAE
Section Staff Liaison
Medicare Physician Fee Schedule Final Rule for 2024 Released
Medicare released the final rule for the 2024 Physician Fee Schedule (PFS) on November 2, 2023. A summary of the 2414-page final rule prepared by Michael A. Granovsky, MD, CPC, FACEP, President of LogixHealth, a national ED coding and billing company and David A. McKenzie, ACEP Director of Reimbursement follows.
Physician Fee Schedule Conversion Factor:
The Centers for Medicare and Medicaid Services (CMS) released the 2024 Medicare Physician Fee Schedule Final rule on November 2nd. This is the document that informs what Medicare payments will be for the following year. As expected, the conversion factor, a dollar amount which when multiplied by the relative value units assigned to a code to determine the payment amount, is expected to drop by 3.39 percent. The estimated impact on emergency medicine will be minus two percent to offset increases in new payments to maintain statute driven budget neutrality across the entire fee schedule.
However, ACEP is lobbying Congress to step in with new funding to prevent or lessen these cuts. HR 2474 the Strengthening Medicare for Patients and Providers Act would provide an annual update the conversion factor equal to the increase in the Medicare Economic Index (MEI), but the cost of this legislation may be too high for broad support under our current national fiscal situation.
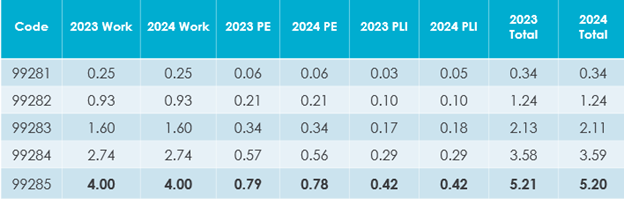
ED E/M RVUs Remain Stable
CMS did not make changes to the Work RVUs for the ED E/M codes, but there were a few small changes to the Practice Expense and Professional Liability Insurance RVUs at the hundredth decimal place.
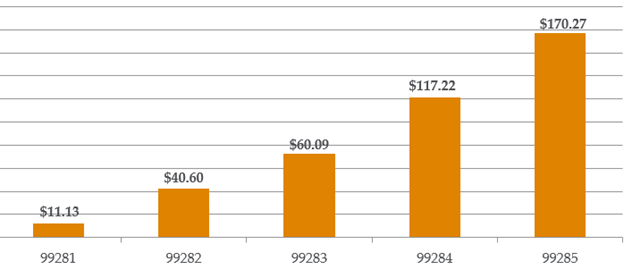
If we apply the revised 2024 final conversion factor of $32.7442 The ED E/M codes payments should look like this:
Split or Shared Services: CMS has finalized its policy on “split” or “shared” E/M visits by a physician, when the visit is performed in part by both a physician and an Advanced Practice Provider (APP), who are in the same group and the physician meets certain criteria termed the “substantive portion” of the visit. CMS has accepted new language in the 2024 CPT code set, so the rules are aligned for both CPT and CMS in 2024. CMS is continuing to limit the split or shared concept to E/M codes only, not procedures.
In 2024, the definition of substantive portion means more than half the total time spent by both the physician and the APP for the encounter, or a substantive part of the medical decision-making. CPT uses the example of the physician made or approved the number and complexity of problems addressed at the encounter (COPA) and takes responsibility for the inherent risk of complications and/or morbidity or mortality of patient management; thereby performing two of the three categories of MDM and the substantive portion of the visit.
CMS is proposing to allow split/shared visit billing for critical care because it believes the practice of medicine has evolved towards a more team-based approach to care, with greater integration of physicians and NPPs into the clinical practice, particularly when care is furnished by clinicians in the same group in the facility setting. Since critical care is a time-based service, CMS requires practitioners to document in the medical record the total time that critical care services were provided and identify the provider who performed the majority of the patient care time. The provider that provides more than 50 percent of the total time should be the one to report the critical care code.
Look for updated FAQ sets in the coming weeks on both the RBRVS Equation and Split or Shared Services on the ACEP website under Reimbursement FAQs for full details on these and other topics.
Telehealth: While no new codes were permanently added to the Medicare Telehealth Services list, finalizes a new process for adding, removing or otherwise changing codes on the list, and creates differential payment based on the place of service.
In this rule, CMS decides to maintain all five ED E/M codes (99281-99285). Thes codes are listed as provisional in Table 11 of the 2024 PFS Final Rule meaning that they may be reported via telehealth at least through the end of 2024.
Additionally, some observation codes on the list of approved telehealth services at least through the end of CY 2024:
- Initial Hospital Inpatient or Observation Care - 99221-99223
- Hospital Inpatient or Observation Care Services, Same Day Admission and Discharge - 99234-99236
- Discharge from Hospital Inpatient or Observation Care - 99238-99239
Additional Resources
Resources for these and other topics can be found on the reimbursement section of the ACEP website. ACEP Director of Reimbursement David McKenzie, CAE, is also available to field your questions.



