Ultrasound-Guided Superficial Cervical Plexus Block
Laura Pumarejo, MD, Ultrasound Fellow, Kaiser Permanente San Diego
Gabriel Rose, DO, Co-Director of Emergency Ultrasound, Kaiser Permanente San Diego
Case
A 73-year-old female presents to the emergency department (ED) with right-sided clavicular pain. She was recently diagnosed with a right clavicle fracture (Figure 1) and was discharged home with a sling and oral analgesia. The patient returned to the ED due to persistent severe pain despite taking her oral medication. On physical examination, the patient appeared uncomfortable, and a deformity was noted with tenderness to palpation along the distal aspect of the right clavicle. The patient had a very limited active range of motion of the right upper extremity, with a maximum shoulder abduction of 10-15 degrees, limited due to pain. The ED physician performed a superficial cervical plexus nerve block (SCPNB) with ultrasound guidance, and the patient had a complete resolution of pain within 15 minutes. Range of motion also improved, with near 180-degree shoulder abduction achieved.

Figure 1. Patient’s X-ray demonstrating right clavicle fracture
Background and Anatomy
The SCPNB may be used in the setting of clavicle fractures or to facilitate painful procedures along the submandibular area and lateral neck, such as abscess drainage, laceration repair, and internal jugular vein (IJV) central line placement.
The superficial cervical plexus (SCP) is located just deep to the sternocleidomastoid muscle (SCM) and superficial to the prevertebral fascia, which envelops the levator scapulae (LSM) and scalene muscles. The SCP exits out and around the lateral border of the sternocleidomastoid muscle (SCM) at approximately the level of the thyroid cartilage and divides into its four branches: greater auricular nerve, transverse cervical nerve, lesser occipital nerve, and the supraclavicular nerves (Figures 2A, B).
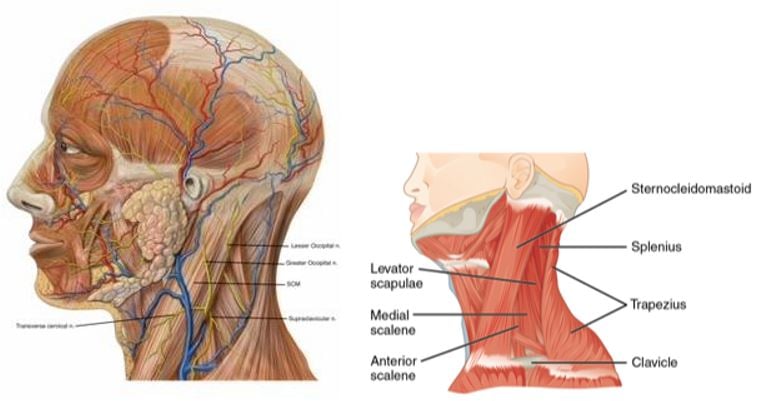
Figure 2A. The four main branches of the superficial cervical plexus as it wraps around the SCM. Credit: Patrick J. Lynch, medical illustrator, CC BY 2.5<https://creative commons.org/licenses/by/2.5>, via Wikimedia Commons. Figure 2B. Muscles of the lateral neck. Note the relationship of the sternocleidomastoid to the LSM and the anterior and middle scalene muscles. Credit: OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons. Modifications by author.
Surface landmarks to identify the SCP include the superior border of the thyroid cartilage, lateral border of the SCM, sternal notch, and the mastoid process. The midpoint of an imaginary line (or drawn with a skin marker) along the lateral border of the SCM that extends from the mastoid process down to the insertion of the SCM into the clavicle marks the injection site (Figure 3).
The dermatomal distribution of anesthesia achieved with the SCPNB extends from the anterior auricular and retro-auricular areas, the submandibular area, the lateral neck, and the cape region along the shoulder and clavicle (Figure 3).

Figure 3. Surface landmarks. The midpoint between the clavicular insertion and the mastoid process marks the site of injection (star). The white outlined area represents the distribution of anesthesia. 1. Sternal notch. 2. Thyroid cartilage. 3. Mastoid process. Credit: http://highlandultrasound.com/superficial-cervical-plexus-block
Patient Positioning
The patient is seated upright with the head of the bed elevated near or at 90 degrees. The block may also be performed with the patient in the supine position with their head rotated slightly to the contralateral side.
Equipment and Procedure
This procedure requires a high-frequency linear transducer, sterile probe sheath and gel, chlorhexidine scrub, a standard 25-gauge 1.5-inch needle, 10 mL syringe, and a local anesthetic agent (we recommend 0.5% ropivacaine or 0.5% bupivacaine). The ultrasound machine is placed on the contralateral side opposite the physician to optimize ergonomics.
Place the transducer on the lateral neck over the SCM at the level of the thyroid cartilage and slide laterally to identify the tapering edge of the SCM, the underlying LSM, the IJV, and the pulsating carotid artery (CA). The SCP nerve bundle may or may not be visible as hypoechoic dots within the fascial plane immediately deep into the SCM. This hyperechoic fascial layer deep to the SCM is the target plane for deposition of anesthesia (Figure 4A, B).
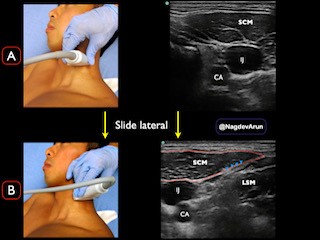
Figure 4A. Transducer placement over the SCM at the level of the thyroid cartilage with corresponding sonographic anatomy. Figure 4B. Slide transducer to the lateral border of the SCM where it tapers and finds the LSM just below. The SCP is located within the fascial plane (arrow heads).
Using an in-plane approach, insert the needle until the tip is visualized within the fascial plane just deep to the SCM and superficial to the prevertebral fascia overlying the LSM and scalene muscles (Figure 5A). After negative pressure aspiration, inject 5-10 mL of anesthetic, which should “hydrodissect” open the fascial plane between the SCM and the deeper muscle layer (Figure 5B). You can also trial 1-2 mL of normal saline in the initial hydrodissection until you have confirmed the right facial plane.
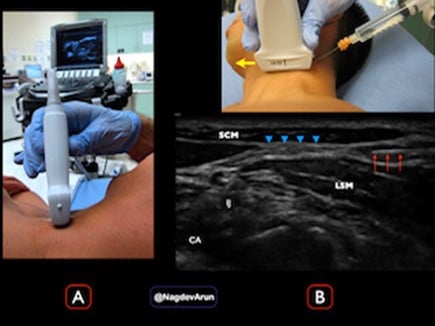
Figure 5A. Probe placement with the machine in direct view on the contralateral side of the patient. Figure 5B. (Top) Needle approaches in-plane from lateral to medial, with probe marker oriented medially (yellow arrow). (Bottom) Corresponding images demonstrating needle tip (red arrows) entering the fascial plane (blue arrowheads) between the SCM and LSM. Anechoic anesthetic is seen to hydrodissect the fascial layers apart.
Complications
Although rare, vascular puncture into the IJV or CA can usually be avoided with direct needle visualization throughout the procedure. Local anesthetic systemic toxicity (LAST) may occur when large quantities of anesthetic are used. Determining the maximum doses for each local anesthetic agent is vital before performing this block. Finally, be sure to keep the needle superficial to the prevertebral fascia and its underlying muscles to avoid potential injection into the brachial plexus.
Discussion
Regional anesthesia offers an effective alternative method to pain control where opioids are inadequate or contraindicated, as in the elderly or obese population who are at risk of over-sedation, delirium, and respiratory depression. The SCPNB is a rapid, simple approach to achieving anesthesia along the lateral neck, submandibular area, clavicle, and overlying cape region for multiple indications. In the above example, SCPNB was used successfully in an elderly patient presenting with severe pain from a clavicular fracture.
References
- Herring AA, Stone MB, Frenkel O, et al. Case Report: The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am J Emerg Med. 2012;30(7):1263-7.
- Kim JS, Ko JS, Bang S, et al. Cervical plexus block. Korean J Anesthesiol. 2018;71(4):274-88.
- Nagdev A, Hering AA. Pain control using ultrasound-guided superficial cervical plexus block. November 19, 2014. Accessed June 1, 2022.
- Highland Emergency Ultrasound. Superficial cervical plexus. Accessed June 1, 2022.
- Bendtsen TF, Abbas S, Chan V. Ultrasound-guided cervical plexus nerve block. Accessed June 1, 2022.



