
Tips and Tricks: Ultrasound Guided Regional Anesthesia of the Hand
Introduction
Emergency medicine physicians commonly perform painful procedures including laceration repair, reductions of fractures and dislocations, incision and drainage of abscesses and debridement of burns. Local anesthesia is an essential component of procedural pain control. Direct infiltration of local anesthetic is only efficient for simple wounds in cooperative patients. Nerve blocks allow physicians to anesthetize large anatomic regions with smaller volumes of local anesthetic than would be required for direct infiltration. Ultrasound (US) guidance for nerve blocks allows physicians to target peripheral nerves under direct visualization which may improve first pass success compared to the landmark approach to regional anesthesia.1-2
US guided nerve blocks in the forearm target the Radial, Median and Ulnar nerves. They are indicated for pain control in various hand injuries including lacerations, fractures, and deep soft tissue infections. Contraindications include an infection at the site of injection, allergy to anesthetic, risk for compartment syndrome, and the uncooperative patient. Emergency physicians who have had only one hour of training can anesthetize all 3 nerves in under 10 minutes.3 These blocks can be used individually, or in conjunction, to achieve either partial or total anesthesia of the hand.4-5 Using forearm blocks for hand anesthesia may actually reduce the risk of local anesthetic systemic toxicity when compared to extensive local injection.6 Below we describe the technique for ultrasound guided regional anesthesia of the hand.
Technique
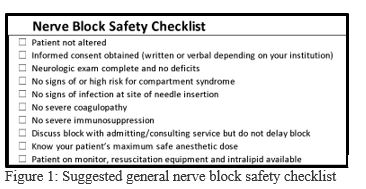
1. Use a safety checklist (Figure 1)
With any nerve block we recommend using a safety checklist.
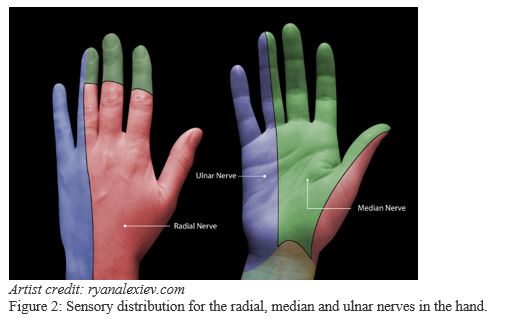
2. Know the sensory distribution of each nerve (Figure 2)
Decide on either a partial or complete block of the hand.
For major hand injury:
- Block the radial, median and ulnar nerves (complete hand block)
For injury to thumb, index, middle and ring fingers or for injury to palmar or dorsal hand not on ulnar aspect:
- Block the radial and median nerves
For boxer’s fracture, injury to ulnar hand or little finger:
- Block the ulnar nerve
3. Locate the nerves (Figure 3)
Difficulty clearly identifying nerves amongst the other structures is a common frustration. In cross-section on US, a nerve appears as an elliptical bundle containing many small scattered echogenic foci and running within a fascial plane. These blocks are best performed in the mid-forearm. The distal forearm has many tendons which may be mistaken for nerves and in the proximal forearm the nerves are deeper making them more difficult to target.
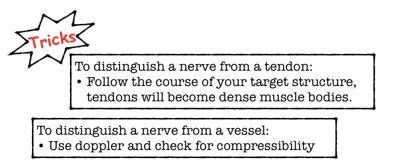
Finding the radial nerve:
- Find the radial artery in cross section at the wrist.
- The radial nerve is seen adjacent to the artery on the radial side.
Finding the median nerve:
- Start with probe centered on volar wrist and move proximally to mid-forearm.
- The median nerve can be visualized between flexor digitorum muscles.
Finding the ulnar nerve:
- Find the ulnar artery in cross section at the wrist.
- The ulnar nerve is seen adjacent to the artery on the ulnar side.
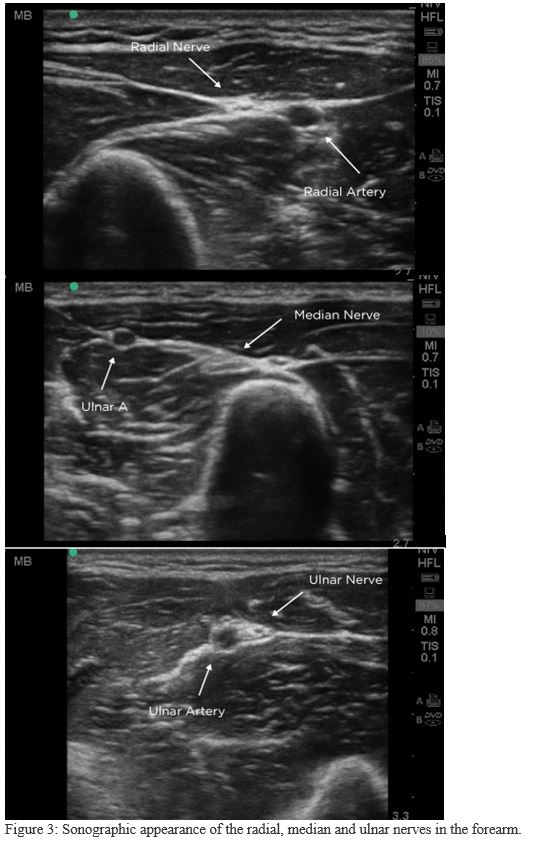
4. Gather your equipment and anesthetic
Know the duration of action and the maximum safe dose for your chosen anesthetic (Figure 4). For prolonged anesthetic duration use anesthetic with epinephrine. Inject 5-10 mL of anesthetic per nerve.
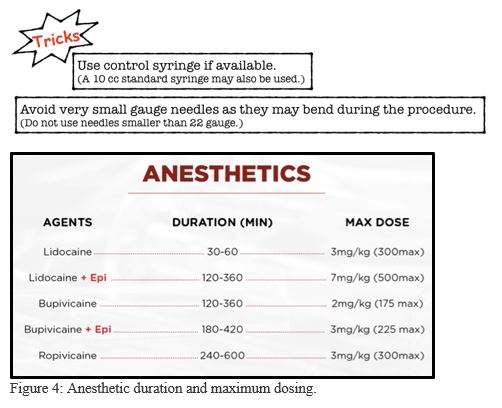
5. Position yourself and your patient (Figure 5)
Spend sufficient time setting up for the procedure. If you and your patient are comfortable, you are more likely to perform a safe and successful block. Rest the patient’s arm on a mayo stand for greater stability. Position the ultrasound machine in front of you, don’t look sideways or backwards over your shoulder. The patient’s arm will be between you and your US machine.
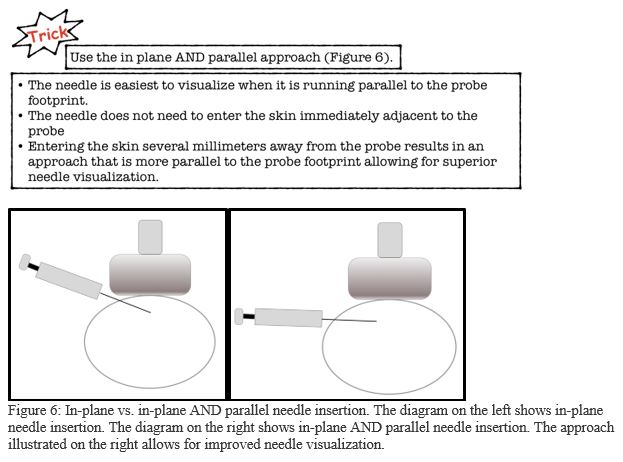
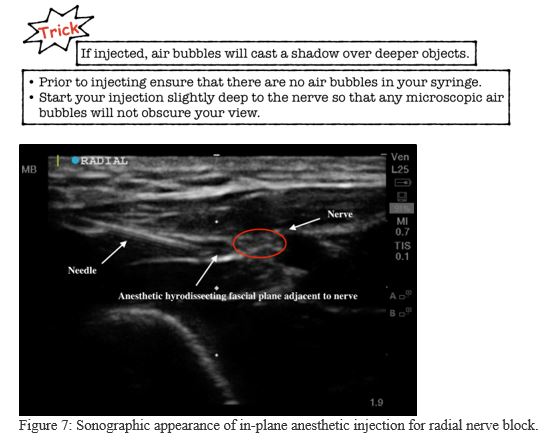
6. Inject the anesthetic (Figure 7)
Clean the injection site with chlorhexidine or alcohol and use an US probe cover to avoid any contamination of the injection site. This procedure should be done using a clean technique but does not require sterility. Hydro-dissect the fascial plane surrounding the nerve without penetrating the nerve bundle. The nerve bundle does not need to be completely surrounded by anesthetic. Anesthetic injected immediately adjacent to the nerve is usually sufficient.
7. How to avoid complications
To avoid accidental vascular puncture
- Track the nerve up and down the forearm to find the optimal site for safe injection. Ensure that your targeted nerve is at a safe distance from the vessel.
- Draw back prior to injecting your anesthetic to ensure you are not in a vessel.
To avoid intraneural penetration
- Always inject your anesthetic very slowly.
- Visualize the anechoic fluid as it surrounds the nerve.
- Your patient should not experience pain while you inject. If your patient has discomfort, or you feel resistance while injecting, withdraw your needle, to make sure you clearly see the needle tip.
8. Documentation and completion of the procedure
Documentation in the medical record should include:
- Indication for block
- Type of block
- Type and volume of anesthetic used
- Confirmation of informed consent
- Confirmation that patient had no contraindications
- Documentation of clean or sterile technique
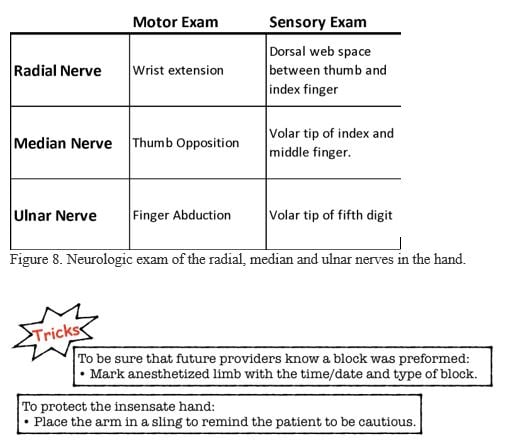
- Neurovascular exam before and after procedure (Figure 8)
- Any complications of the procedure
- After the procedure the neurologic exam should be repeated when the block wears off to document return of function.
References
- Marhofer P, Harrop-Griffiths W, Kettner SC, et al. Fifteen years of ultrasound guidance in regional anesthesia; Part 1 and 2. Br J Anaesthesia. 2010; 104(5): 538-46.
- Bhoi S, Sinha TP, Rodha M, et al. Feasibility and safety of ultrasound-guided nerve block for management of limb injuries by emergency care physicians. J Emerg Trauma Shock. 2012;5(1):28-32.
- Liebmann O, Price D, Mills C, et al. Feasibility of forearm ultrasound-guided nerve blocks of the radial, ulnar and median nerves for hand procedures in the emergency department. Ann Emerg Med. 2006;48:558-61.
- Loewy J. Sonoanatomy of the median, ulnar and radial nerves. Can Assoc Radiol J. 2002;53(1):33-8. Review.
- McCartney CJ, Xu D, Constantinescu C, et al. Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med. 2007;32(5):434-9. Erratum in: Reg Anesth Pain Med. 2008;33(2):188.
- Barrington M, Kluger R. Ultrasound guidance reduces the risk of local anesthetic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38:289-99.
Siobhan Smith, MD, MS
Viveta Lobo, MD, FACEP
Stanford University Medical Center



