CEDR Operations Update
This year brought unprecedented events impacting all of emergency medicine, including CEDR. The COVID-19 pandemic brought executive action from the Centers for Medicare and Medicaid Services (CMS) to eliminate the Merit Incentive Payment System (MIPS) reporting requirements for 2019. This resulted in an almost complete removal of penalties for 2019 reporting. Since MIPS is a budget neutral program, this evaporated the bonuses for those who performed well in 2019 quality measures.
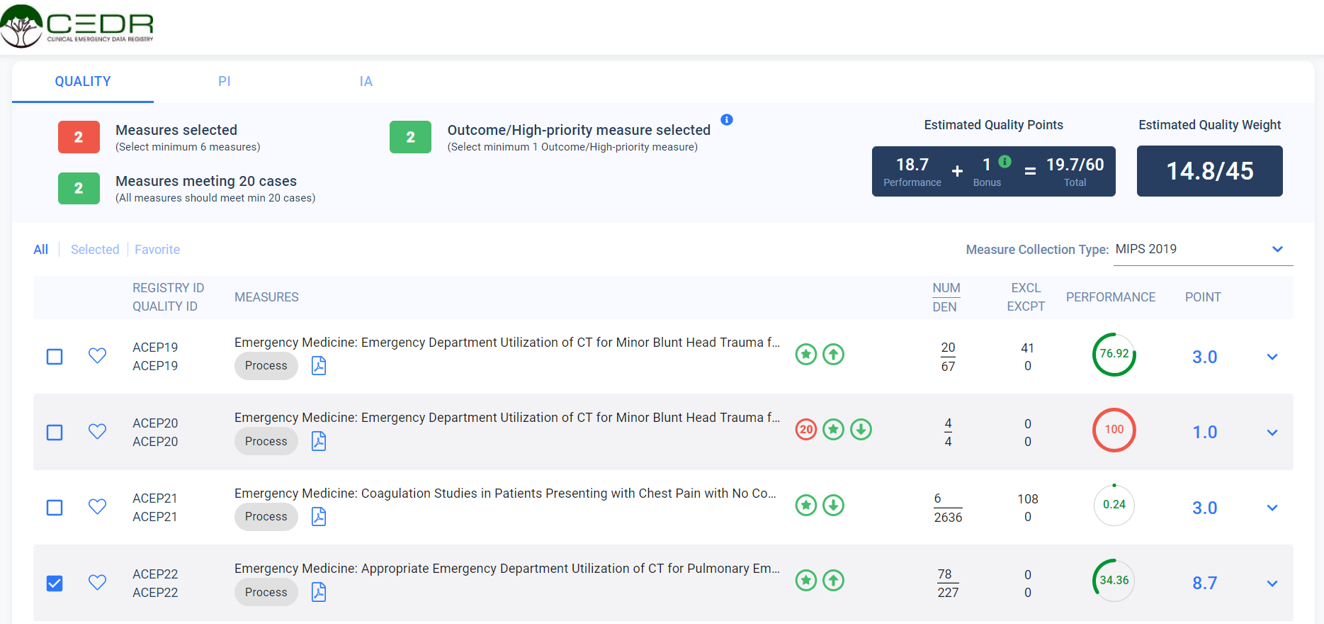
We found in July that only participants who scored above the exceptional performance threshold received any positive adjustment and the maximum adjustment was an anemic 1.79%. Fortunately for our CEDR participants, 80% of Tax Identification Numbers (TINs) submitted through CEDR reached the exceptional performance threshold and still received some benefit from their 2019 efforts. Based on the feedback from CMS and some basic assumptions about Medicare billing in the Emergency Department (ED), ACEP estimates that CEDR participants overall will receive approximately $3.4 million in additional reimbursement during 2021.[1]
For 2020, COVID-19 continues to impact the MIPS program. CMS announced that clinicians and groups impacted by COVID-19 could apply for extreme and uncontrollable circumstances exemption by reporting for the 2020 performance year. While the benefit of this option is the removal of any chance of a penalty from the 2020 performance year, this will likely result in similar impacts to the positive adjustments which occurred for 2019. The maximum bonus may increase a bit, as the threshold for the exceptional performance pool has increased from a MIPS score of 75 in 2019 to 85 in 2020.
CMS released the 2021 Proposed Final Rule in August. Some important proposed changes to the MIPS program create significant opportunities for CEDR participants to protect their reimbursements in 2021. CMS proposes to remove historical benchmarks as the basis for scoring measures submitted for the 2021 performance year. CMS will calculate benchmarks after all 2021 data is submitted in Q2 of 2022. This will blind clinicians who participate in the program from any knowledge of how their quality measures might score in the program during 2021. As such, participation in the program evolves into a statistical numbers game, with possible MIPS scores increasing proportionally to the number of measures reported. With CEDR providing 10-20 measures on average for participants with clinical data submissions to CEDR, their statistical chances of avoiding penalty are practically 100%, and the probability for exceptional scores is also very likely. CMS will release the 2021 Final Rule later this year, so this benchmark challenge is not yet final. Either way, ACEP’s CEDR program will continue to maximize the benefits we offer to our clinicians.
If you are interested in learning about CEDR, please contact us at cedr@acep.org or visit our website.
[1] Assumes $140 average base reimbursement, 28% of ED visits are Medicare reimbursed, and 15 MIPS points from the Cost category and Complex Patient Bonus.
Author(s)

Bill Malcom, MS, MBA, PMP
CEDR Program Director, ACEP
 American College of Emergency Physicians
American College of Emergency Physicians

