Patients who don’t get bathed each day or don’t get meals on time, because there’s not enough staff. Patients just out of surgery who need a nurse dedicated to watch only them, but instead have to share.
Patients in pain from a broken bone who wait hours for sedation because there are no ER beds, while ER patients wait for the ICU beds their lives may depend on.
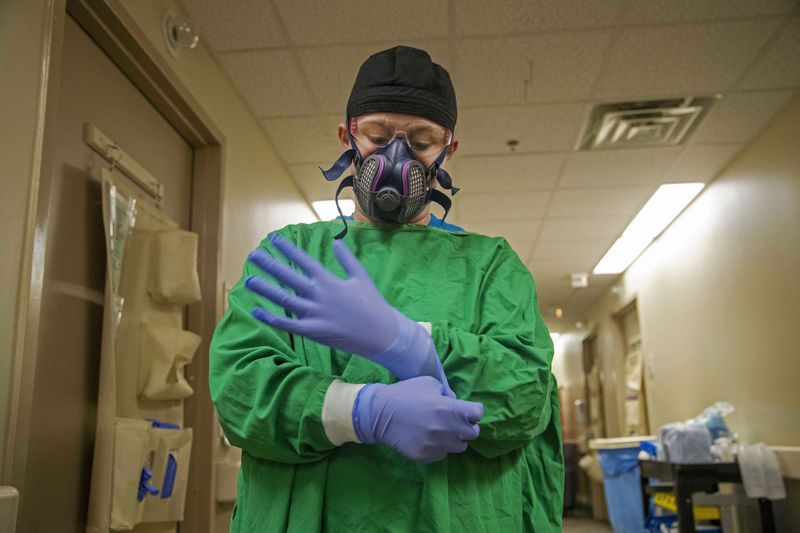
These things are happening now. COVID-19 cases are swamping more Georgia hospitals, testing them in ways that were previously unimaginable. Hospitals say that they are not rationing the most important care — yet. But, caregivers are already making decisions about who gets which scarce resources. The only question is how grave those decisions will become, with projections showing that hospitalizations will continue to surge in the weeks ahead.
“We are treating patients in the hallways, in triage areas, in waiting rooms,” said Deborah Matthews, senior vice president and chief nursing officer at Tanner Health System in west Georgia. “Every day we huddle as a team and look at our options. We are having to do things we have never had to do before.”
Grady Memorial Hospital is full. Wellstar Atlanta Medical Center is full. The intensive care units or emergency departments of Piedmont Atlanta Hospital, Northside Atlanta Hospital, Emory University Hospital, Wellstar North Fulton Hospital, Wellstar Kennestone Hospital and others in the Atlanta metro area are full, as of data reported Wednesday afternoon. So were ERs in Covington, Chatsworth, Eatonton, Statesboro and other towns throughout Georgia at points on Wednesday, and ICUs in most parts of Georgia.
“If it were just one area of the state that was disproportionately hit, you can shift resources,” said Dr. Harry J. Heiman, clinical associate professor at Georgia State University School of Public Health. “We’re being stressed across the state.”
Credit: Alyssa Pointer / Alyssa.Pointer@
Credit: Alyssa Pointer / Alyssa.Pointer@
It’s not just COVID-19 patients who are affected. Hospitals are running out of beds, and, most crucially, staff, for all patients.
Dave Williams, a member of the civilian Metropolitan Fire Association who monitors emergency scanners across the region, this week heard a North Fulton County ambulance worker trying find a hospital to accept a 90-year-old with a broken bone. Hospital after hospital had turned the ambulance away, until the crew took the matter into their own hands. “They finally just said, too...bad, they’re coming,” Williams said.
Gov. Brian Kemp said his focus is on making sure that the state has enough hospital beds for everyone who needs one. The state is racing to reopen the Georgia World Congress Center as an emergency field hospital for a third time. It will take overflow patients from other Georgia hospitals who need a hospital bed but not intensive care.
But Kemp acknowledged the challenge is more than just buildings and beds — it’s the limited availability of trained medical workers. The facility has equipment for 112 total beds, but plans to ramp up to 60 staffed beds in the coming days, as staff is acquired.
“The real issue there is the staffing because of what we’re seeing going on in the rest of the country,” Kemp said. “The staffing issue has been the hardest part for any governor, any hospital CEO and it doesn’t matter what state you’re in.”
EARLIER IN THE AJC: Georgia doctors plan for wrenching choices amid slim ventilator supply
Meanwhile, hospital officials are bracing for more patients to flood in.
“This week, we surpassed the number of hospitalized patients with COVID-19 in critical and acute care as compared to any time since the pandemic started,” Emory Healthcare spokeswoman Janet Christenbury said. “The rapid and continuous rise in cases remains very concerning. We do not expect any reduction in cases over the next few weeks, which will only make a very difficult situation more extreme.”
Hospital officials in northeast Georgia, where COVID-19 patients make up nearly 40% of all those hospitalized, issued a public statement begging people to wear masks and distance for the holidays, openly warning that with rising cases health care will have to be rationed.
“We never really imagined that anything like this could really happen,” said Dr. Clifton Hastings of Northeast Georgia Health System.
Hastings walked outside the system’s flagship Gainesville hospital earlier this week and saw eight ambulances, waiting, with patients needing space in the ER. The situation is wearing on caregivers, too, he said. “They’re beat,” he said. “I’ve seen probably six people crying today.
“Our needs are greater than the ability to meet those needs sometimes,” Hastings said.
“We are over capacity’
Both of the Atlanta’s area top tier trauma centers — Grady Memorial Hospital and Wellstar Atlanta — were diverting ambulances Wednesday afternoon, with their ERs severely overcrowded and their ICUs full.
Dr. Robert Jansen, chief medical officer for Grady Health System, said it is doing all it can to make sure it can accept trauma, stroke and burn patients from across the state while juggling the heavy pandemic caseload.
“We currently have more COVID patients than we’ve ever had,” Jansen said Wednesday. “As for critical care capacity, we are over capacity.”
COVID-19 patients who need critical care beds are waiting in the emergency department for ICU beds to become available, he said.
“It is concerning. The more people you have in the emergency department waiting to go into (an ICU) bed that limits the capacity you have in the emergency department to care for new patients,” he said. “Right now, we’re doing OK at that, but it’s a constant balancing act. It’s a struggle.”
Jansen said the hospital is planning to find “non-traditional” areas within its campus to add 50 to 100 patient beds.
“We just have to find the staff to serve those areas,” he said. ‘If you look across the region and the state you will find just about everybody is in the same position, which is really frightening.”
Some parts of the state, he said, could reach the point that hospitals in California have. There, some have had to resort to “crisis care” guidelines that allow for rationing care, according to the Associated Press.
Paramedics are declining to transport some less severely ill patients whom they might take to the hospital under ordinary circumstances.
— Los Angeles Times (@latimes) December 30, 2020
It’s one of a limited number of tools left to deal with the wave amid a crisis due to a flood of COVID-19 patients.https://t.co/yI7whPWIzd
Jansen said he doesn’t think metro Atlanta will reach that point but he said, “If the surge is worse than we expect...it could overwhelm us.”
Georgia hospitals held 4,518 COVID-19 patients as of about 2 p.m. Wednesday, according to state data. That’s more than three times the number of patients hospitalized in mid-October. As bad as the summer peak was, the number now is 41% higher.
Limited resources
While COVID-19 vaccines are beginning to arrive in Georgia, they are currently only being administered to health care workers and nursing home residents and at a much slower rate than expected.
“It is not quick enough to get us out of this crisis at this point,” said Jen Kates, with Kaiser Family Foundation.
Credit: HANDOUT
Credit: HANDOUT
Reimposing restrictions, such as shutting down indoor dining and suspending elective surgeries, could ease the situation, she said. Some states have taken those steps, but Kemp has refused, calling instead for Georgians to wear masks and follow other advice from experts.
The worst case scenario: rationing.
Many hospitals across the state already developed written plans last spring for how to ration care, when officials feared a shortage of breathing machines, called ventilators.
The ventilator crisis faded, but now the plans may guide decisions on which patients will get the limited resources, including staff time, they may need in order to survive.
The U.S. Health and Human Services Department’s civil rights office earlier this year said that states can’t allow medical providers to discriminate on the basis of age, race or disabilities in deciding who would receive lifesaving medical care during the pandemic.
But plans such as the University of Pittsburgh’s, which a number of Georgia hospitals have used as a model, suggest factors such as the patients’ likelihood to survive and the years of life that would be saved.
Georgia hospital officials interviewed said that they hoped never to make such calls. But calls with lower stakes are already being made.
“People don’t like to hear about the idea of rationing care, and hospitals don’t like to talk about it because it is a PR disaster. But it will become a reality once you run out space and devices, and don’t have enough health care workers,” said Dr. Ryan Stanton, a board member with the American College of Emergency Physicians based in Kentucky. He said much of the country is “teetering on the edge” of hospital capacity.
Americans assume they will have access to high levels, almost perfection levels, of health care, Stanton said. “But the sobering reality is when people go to the hospital, this may no longer be the case.”