
Exertional Heat Stroke
I am writing this while at a conference at the NCAA in Indianapolis. Doug Casa, Ph.D., the foremost authority on exertional heat stroke and director of the Korey Stringer Institute, presented athlete after athlete who either died or ended up in a unit and/or on a transplant list as a result of heat stroke. When these cases were dissected, the failed intervention became clearer. In some instances, rapid cooling was never initiated on the sideline. In some, it was initiated but then stopped when EMS arrived and transported the patient, instead of allowing the patient to cool before transport; a mantra of the National Athletic Trainers Association (NATA).
As an emergency physician, the most devastating cases were when the patient was in the ED but the diagnosis was never considered. Defending my primary specialty, I can argue that the error is not totally unreasonable - a patient presents to the ED with altered mental status and is put in the AEIOU-TIPS algorithm or the sepsis pathway. And until an elevated rectal temperature and a correlating history are obtained, and makes the diagnosis a slam-dunk (it is Final Four season in Indy right now), precious minutes are lost. Heat related death is a completely preventable type of death. And any death, but especially a preventable death, is an opportunity to learn. Sadly, the problem is getting worse.
The rate of heat stroke in the five year period of 2005-2009 was higher than any five year period in the previous 35 years. When “prompt, proper, and aggressive treatment begins within 10 minutes of collapse” (EHS- new concepts regarding cause and care), heat stroke is 100% survivable. The ongoing trend in heat stroke deaths represents a gap between current evidence and practice patterns, both in the emergency department and at the site of collapse. On the sideline, the NATA recommends ‘Cool First, Transport Second” for the treatment of heat stroke patients. EMS protocols don’t match this evidence based guideline and there is much work to be done to change this, on paper, and in practice.
To review, exertional heat stroke is a life threating condition characterized by CNS dysfunction and a core temperature of >104F (40.0C). The long term pathophysiological response to heatstroke is caused by a systemic inflammatory response syndrome (SIRS) that commences following damage to the gut, which leads to an endotoxin leak in the systemic circulation, leading to a systemic immune response. The thermoregulatory, immune, hematologic, and coagulation systems respond in a way that is similar to sepsis. In a short time, encephalopathy, rhabdomyolysis, and hepatic and renal failure result, and eventually, the damage becomes irreversible and ultimately fatal.
Heat stroke victims may exhibit a range of CNS dysfunction from sudden collapse and altered level of consciousness to subtle behavioral changes such as aggression.
Recognition on the sideline is not nearly as difficult as recognition in the emergency department. The sideline differential for an athlete with CNS alterations on a hot day is long, but common things being common, really boils down to one or two things. However, in the ED, the differential shifts and campaigns that push timeliness of antibiotic or medication administration practically shoves providers down the wrong algorithm.
We know that there are numerous possible etiologies for the confused or altered patient (the age old mnemonic – AEIOU-TIPS). However, exertional heat stroke must be considered early in the young, active population and especially in high risk populations such as football players, runners, and the military. To rule out EHS, a rectal temperature must be obtained. Other, more convenient body temperature measurements such as temporal, tympanic, sublingual, and axillary do not measure core body temperature and delays arrival to the correct diagnosis.
The goal of treatment is reducing core body temperature to less than 102F (39C) in less than 30 minutes of collapse or presence of other neurophysiologic deficits.
The most rapid cooling rates are achieved with cold water immersion, making this the gold standard for treatment. 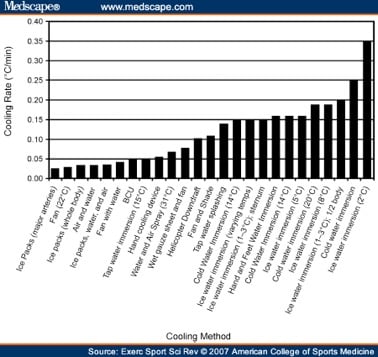
Many consider heat related illness a problem of the south. In fact, it is not the absolute temperature that results in exertional heat stroke but one’s acclimatization to the rise in temperature. So while heat stroke is common in the south, it is in fact, quite common in the north as well.
Spring football is currently underway in most of the country, and after a short respite, football will be in full swing. If you encounter an athlete presenting right off the field with altered mental status, get a rectal temperature and start cooling as you entertain other etiologies. Who knows? Maybe by the time you hang the antibiotics, the patient will be back to normal.
Neha Raukar, MD, MS



