
Tendon Injuries in the Emergency Department
Emily Harrington, MD
PGY2, Medstar Health/Georgetown-Washington Hospital Center
R. Conner Dixon, MD, CAQ-SM
Attending Physician, Kaiser Permanente Santa Clara
Korin Hudson, MD, CAQ-SM
Associate Professor of Emergency Medicine, Medstar Health/Georgetown-Washington Hospital Center
Pearls
- Consider tendon injury for any mechanisms involving an eccentric load
- Ultrasound is the imaging of choice as it is 1) accurate; 2) fast; 3) easy; and 4) inexpensive
- Ensure proper immobilization and timely orthopedics follow up
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen are appropriate for pain control
- In patients with an acute tendon rupture, consider possible secondary causes:
- Anabolic steroid abuse
- Renal disease
- Metabolic bone disease (hyperparathyroidism)
- Medications associated with tendon rupture (eg, quinolones, corticosteroids)
Pitfalls
- Failing to further assess a musculoskeletal injury after a negative x-ray
- Failing to assess for deficits in active range of motion
- Failing to assess resisted strength
Case 1 - A Powderpuff Pop
You’re working in the fast track section of the ED, and your next patient is a 22 year old female who presents with right ankle pain and swelling. She states she was playing in a charity powderpuff football game at her college and while she was running with the ball, she cut sharply to avoid a defender and felt a pop in her ankle. She is unsure if she rolled her ankle or if the defender stepped on her, but states she was immediately unable to walk and came straight to the hospital.
On exam, the ankle is diffusely swollen. She has no bony tenderness of the medial or lateral malleolus but does have some calcaneal tenderness. No other bony foot tenderness on palpation. She is able to dorsiflex but unable to plantarflex. She has no neurovascular deficits.
Differential DDx
- Ankle sprain
- Ankle fracture
- Ankle dislocation
- Achilles tendon rupture
- Calf strain
You order ibuprofen and x-rays of the ankle and tib/fib. Your x-rays come back normal; however, the patient’s swelling has continued to worsen, and she is unable to bear weight after pain medications.
You decide to grab your ultrasound to examine the ankle and notice an obvious defect in the Achilles tendon. You put her in a short leg posterior splint (pearl: place them in slight plantarflexion to oppose the two tendon fragments), prescribe ibuprofen for home, and discharge her with referral to orthopedics within the next week.
Discussion
Achilles tendon ruptures usually occur during activities with rapid acceleration/deceleration and/or pivoting. The characteristic patient is a middle aged male playing sports which require jumping (volleyball, basketball, etc.) The rupture most commonly occurs two-six cm above the calcaneus, where blood supply to the tendon is poor. Patients will often complain of feeling a sharp, sudden pain and hearing or feeling a “pop.”
On physical exam, they have inability to plantar flex and are unable to perform a heel raise or stand on their toes. Providers can often feel a defect while palpating the Achilles tendon, with a sensitivity of 73% and a specificity of 89% for detecting a partial tendon tear. However, this finding may be obscured by significant swelling. The Thompson Test, or calf squeeze test, may be performed by having the patient lie prone with their ankles hanging off the end of the bed (see Figure 1). The clinician then squeezes the gastrocnemius muscle belly and watches for passive plantar flexion at the ankle. Lack of plantar flexion is considered a positive test, with a sensitivity of 96% and a specificity of 93%.

Figure 1- Thompson test with no movement of the foot when the calf is squeezed
X-rays usually do not identify any osseous pathology, although avulsion fractures can occur. However, on closer examination, soft tissue swelling and changes in the Achilles shadow are often evident. In the ED, ultrasound is the best confirmatory test. Using the linear probe, the Achilles tendon is best evaluated in longitudinal view, evaluating for tissue gaps, disorganized fibers, fluid, or hypoechogenicity (see Figure 2).
Figure 2 - Tissue gap, fluid, and disorganized muscle fibers seen in longitudinal view of the Achilles
Treatment in the ED involves analgesics (NSAIDs are appropriate if the patient has no contraindications), crutches, CAM or walking boot with a one inch heel lift or a splint in equinus, and referral to orthopedics. While traditional teaching has been to place the patient in a posterior short leg splint with about 30 degrees of plantarflexion (equinus), recent studies are suggesting that this may be inferior to the CAM/walking boot with a one inch heel lift and early mobilization. Given this is new data, it is still important to discuss treatment protocols with your orthopedic surgery department and have an agreement as to avoid miscommunication with management. With either method, the heel lift/equinus positioning is important to approximate the two ends of the tendon for the best chance at complete recovery. All suspected Achilles tendon ruptures should receive surgical consultation, as many surgeons will offer patients surgical repair. Non-athletes and older patients may be treated non-operatively with six-eight weeks of immobilization in a short leg cast or splint; however, they should be informed there may be a higher risk for re-rupture.
Case 2 - “Still Got It”
On a particularly busy day in the ED, your next patient was brought in by EMS for knee pain. At first, you are confused because people in the waiting room have been waiting for four hours and this knee pain was brought straight back into the room. Upon entering, however, you see a 46 year old man with an obvious left knee deformity. He states he was a basketball star in college; however, he hasn’t played in the last 15 years. That afternoon, he was playing basketball with his son and his son’s friends when he tried to show off and dunk the ball. He states when he came down, he landed awkwardly and immediately felt a pop in his knee.
On exam, he is very uncomfortable appearing, and you immediately notice a deformity. He has no femoral, tibial, or patellar bony tenderness and no distal neurovascular deficits. He is unable to lift his leg straight off of the bed or fully extend his knee against gravity. Anterior and posterior drawer tests are negative, and there is no pain or laxity with varus or valgus testing either.
DDx
- Patellar fracture
- Patellar dislocation
- Patellar tendon rupture
- Quadriceps tendon rupture
- Knee dislocation
- Patella dislocation
- ACL, PCL, other ligamentous injury
- Meniscal injury
- Patellar tendinitis
- Tibial plateau fracture
- Quadriceps muscle strain
- Tibial tubercle avulsion fracture
The nurse immediately gets an IV started, and you give him 50 mcg IV fentanyl. He goes to x-ray, which shows no fracture or dislocation, but does reveal a high-riding patella. You grab your ultrasound and immediately notice a defect in the patellar tendon (See Figure 3).
Figure 3- Patellar tendon rupture
You put him in a knee immobilizer in full extension, prescribe ibuprofen for home, and discharge him with referral to orthopedics within the next few days with the typical goal for surgery to occur within a week of the injury.
Discussion
Patellar and quadriceps tendon ruptures both often occur during forceful contraction of quadriceps muscle, such as landing from a jump or forceful change in direction or from falling on a flexed knee. Stated differently, there is typically an eccentric load on the extensor mechanism. You may feel a defect above the patella with quadriceps tendon rupture or below the patella with patellar tendon rupture. Both occur approximately 2cm from their respective insertions onto the patella, and both injuries lead to difficulty with straight leg raise and extension of the knee. Quadriceps tendon ruptures are less common. However, they are missed at initial presentation up to 50% of the time, often incorrectly diagnosed as “knee sprain.”
The diagnosis of patellar and quadriceps tendon rupture can be made clinically, based on history and exam findings alone. However, x-rays should be obtained as patellar, and quadriceps tendon ruptures can be associated with avulsion fractures of the patella. You may also see a low riding patella (patella baja) with a quadriceps tendon rupture or a high riding patella (patella alta) with a patellar tendon rupture, which can help make the diagnosis. Ultrasound is the best confirmatory test in the ED, as it allows the clinician to determine the presence and size of muscle and tendon rupture and to view the muscle and tendon function dynamically to assess for gaping with motion or mild resistance.
Treatment in the ED involves analgesics (NSAIDs are appropriate if no contra-indication), knee immobilizer, crutches, and referral to orthopedics. Surgical treatment is indicated if there is a loss of knee extension as seen in complete tears, and in some cases, with partial tears where progression to a complete tear is likely. Prompt surgical consult is indicated as repair within one week is associated with better outcomes. Smaller or partial tears can be treated conservatively with knee immobilization.
Case 3: Popeye - Not the Sailing Kind
It’s the end of your 12 hour shift on a busy day, and you decide to see one more patient that you are hoping to evaluate and quickly discharge before going home. A 57 year old man checked in for right shoulder pain and has been waiting for three hours. You pull him into a chair near the triage area to evaluate him. He states he is a construction worker and was helping carry a heavy sheet of metal when he suddenly felt a sharp pain in his right shoulder with immediate weakness of his right arm.
On exam, you first notice a mass in the mid-upper arm. You also see some swelling and ecchymosis near the shoulder, though he denies any direct trauma. The patient has no neurovascular deficits; however, he has significant pain with flexion of the elbow.
DDx
- Biceps tendon rupture
- Rotator cuff injury
- Dislocated shoulder
- Humeral fracture
- Medial or lateral epicondylitis
You order ibuprofen and an x-ray of the shoulder and humerus. X-rays show degenerative changes of the shoulder joint but no fracture or dislocation. You have a high suspicion for tendon injury, given the exam, so you grab the ultrasound and notice a rupture of the proximal end of the long head of the biceps tendon.
You prescribe ibuprofen, put him in a sling, and refer him to orthopedics, to be seen in the next three-five days.
Discussion
The biceps brachii muscle is made up of a long head and a short head, each of which have a unique origin on the scapula, but share an insertion on the radial tuberosity (see Figure 4). The main functions are flexion and supination of the elbow.
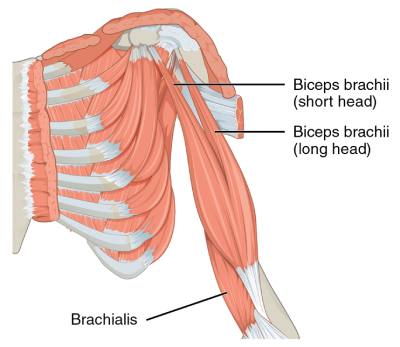
Figure 4 - Anatomy of the biceps brachii
Vast majority of biceps tendon injuries occur to the proximal portion of the long head of the biceps brachii, usually due to sudden or prolonged contraction in a patient with chronic bicipital tenosynovitis or other underlying shoulder dysfunction. Distal biceps tendon tears are less common; however, they usually occur due to the same mechanism of sudden or prolonged contraction.
In patients with a long head biceps tear (LHBT), there may be a distinct demarcation of the distal muscle belly, known as a “Popeye” deformity (see Figure 5). On ultrasound, it appears as you move caudally towards the shoulder in the long axis, you will notice disruption of the tendon away from the glenoid with a fluid filled space (see Figure 6).

Figure 5 - Popeye deformity
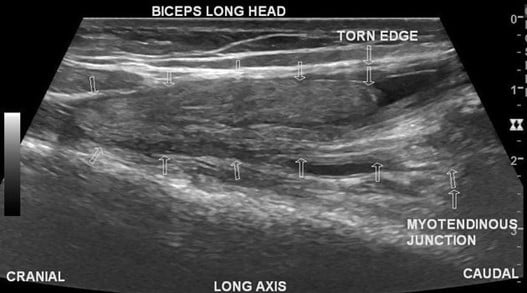
Figure 6 - Rupture of long head of biceps tendon on ultrasound
Patients often have difficulty with flexion and supination of the elbow; however, it is important not to rule out a tendon injury due to a lack of weakness, as lack of strength may be minimal due to the intact short head. With a LHBT, palpation over the bicipital groove often elicits tenderness. There are two special maneuvers, the Speed’s and Yergason’s tests, to further evaluate for biceps tendon injury. For the Speed’s test, the patient’s arm is extended in supination with the shoulder flexed, and the patient is asked to elevate the arm against resisted force. Pain in the anterior shoulder is considered positive. For the Yergason’s test, the patient’s arm is pronated and flexed at the elbow to 90 degrees, and the patient attempts to supinate the arm against a resisted force. Pain localized to long head biceps tendon is considered positive.
For distal biceps tendon evaluation, there is usually pain, swelling, and tenderness over the antecubital fossa. The Hook test can be performed, where the patient flexes the affected elbow to 90 degrees with the forearm fully supinated, and the examiner then attempts to "hook" the distal biceps tendon on the lateral side of the elbow with their index finger and pull it forward. The sensitivity of the Hook test was 78% for all tears and 83% for complete tears but is subject to false negatives.
The diagnosis can be made clinically; however, if unsure, ultrasound is the imaging modality of choice in the ED. X-rays can be obtained to rule out avulsion fractures at the shoulder or elbow. MRI allows for evaluation of underlying shoulder pathology, such as rotator cuff or labral tears, but are not necessary, especially in the ED.
Management in the ED includes analgesics (again NSAIDs are appropriate, if not contraindicated), sling, and orthopedic referral. The majority of proximal biceps tendon tears, especially in elderly and less active patients, are managed conservatively, without surgery. Patients with complete tears that are younger and require full return of strength may opt for surgical repair, which should occur within two weeks of injury. Distal biceps tendon tears are more frequently managed surgically and require prompt orthopedic evaluation.
Resources
- Maughan KL. (2022, June 23). Achilles tendinopathy and tendon rupture. UpToDate. Retrieved July 6, 2022
- Maempel JF, Clement ND, Duckworth AD, et al. A randomized controlled trial comparing traditional plaster cast rehabilitation with functional walking boot rehabilitation for acute Achilles tendon ruptures. Am J Sports Med. 2020;48(11):2755-2764. doi:10.1177/0363546520944905
- Simons SA. (2022, June 21). Biceps tendinopathy and tendon rupture. UpToDate. Retrieved July 6, 2022
- Von Fange, T. (2022, March 30). Quadriceps muscle and tendon injuries. UpToDate. Retrieved July 6, 2022
- WikEM contributors. Achilles tendon rupture. WikEM, The Global Emergency Medicine Wiki. March 22, 2020. Accessed July 6, 2022


