Sub-Dissociative Dose Ketamine in the Emergency Department
Uncontrolled Pain During Procedure
A 44-year-old male presents to the emergency department (ED) after a motor vehicle collision. He was the restrained driver traveling at highway speeds. Per paramedics, he was unable to ambulate on scene and received two doses of Fentanyl 100 mcg en route for pain control. On arrival, trauma assessment is significant for left pelvic tenderness to palpation but otherwise normal examination with stable vital signs. Computed tomography scan of the abdomen/pelvis reveals a left posterior acetabular wall fracture with intra-articular fragments. Orthopedic surgery evaluates the patient and plans for placement of a femoral skeletal traction pin. He has appropriate pain control when lying still and receives additional doses of Fentanyl before and during the procedure. However, the patient continues to scream and move in pain while the traction pin is being advanced through the skin. Your consultant does not feel comfortable proceeding (the drilling part has not even started!) and asks for procedural sedation. Unfortunately, the ED remains chaotic with multiple trauma and medical resuscitations and a growing waiting room. Your charge nurse also states there is no available respiratory therapist at this time for the procedural sedation. You then remember your colleague the other day successfully reduced a shoulder dislocation after administering low dose ketamine due to ineffective opioid usage. You immediately draw up 0.3 mg/kg of ketamine and administer it to the patient. The consultant places the traction pin without difficulty, and everyone, including the patient, is satisfied with the outcome.
Ketamine for Analgesia?
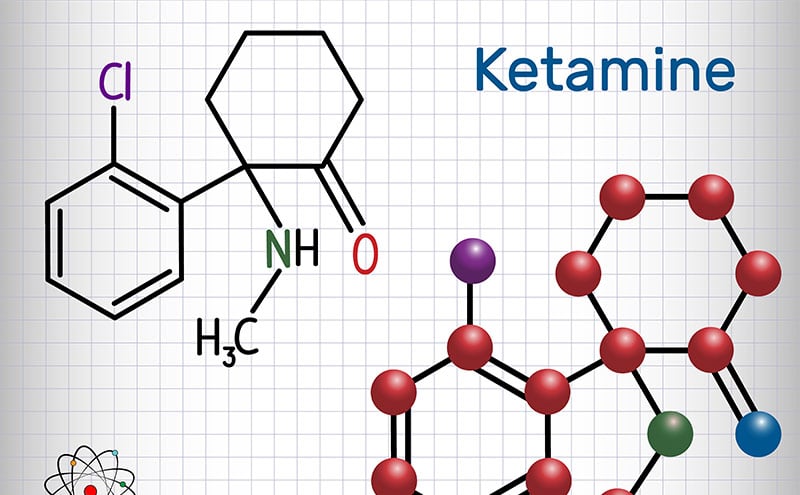
Amid the search for non-opioid alternatives, ketamine has been growing in popularity within the prehospital and ED settings over the last few years. Ketamine is a noncompetitive NMDA/glutamate receptor complex antagonist that reduces pain by acting at the dorsal horn of the spinal cord, thereby decreasing central sensitization.1 This pathway is implicated in the development of chronic pain syndromes, opioid tolerance, and hyperalgesia.1 As a result, ketamine can provide effective analgesia for acute pain, chronic pain, and opioid-tolerant pain at sub-dissociative doses, while sparing the patient moderate sedation and hemodynamic instability.1 Several trials have demonstrated no differences in pain control compared to opioids, but with relatively higher rates of short-lived and minor adverse effects (dizziness, nausea, and mild dysphoria).2 No severe adverse events, such as apnea, cardiac arrest, or true emergence phenomena were detected.2 Although there were concerns of its usage in patients with suspected increased intracranial pressure, a systematic review by Cohen, et al3 demonstrated no differences in cerebral perfusion pressure or outcomes in 953 trauma patients.
Before proceeding, ask if there is any history of hypersensitivity or severe allergies to ketamine in the past or any psychiatric illnesses. Explain the risks and benefits of ketamine analgesic therapy, including the common adverse effects, with the patient and confirm understanding. For administration, an initial bolus of 0.1 to 0.3 mg/kg can be given over 5-15 minutes. Data suggests giving it over a longer duration can significantly reduce the rate of adverse effects.1 For continued pain control, an infusion can be started at 0.15 to 0.2 mg/kg/hr and titrated every 30 minutes as needed by 2.5 to 5 mg or intravenous pushes of 0.3 mg/kg. Draw up 1 mL of ketamine (100 mg/mL) and mix in 100 mL of normal saline; this can serve as your infusion bag that will deliver close to 1 mg/mL. No monitoring of the patient is required at this dosing range, allowing the physician to otherwise continue running the ED. ACEP has a patient care tool for more information on utilizing ketamine for acute pain control in this link here.
References:
- Motov S, Drapkin J, Likourezos A, et al. Sub-dissociative dose ketamine administration for managing pain in the emergency department. World J Emerg Med. 2018;9(4):249-255. doi:10.5847/wjem.j.1920-8642.2018.04.002
- Motov S, Rosenbaum S, Vilke GM, et al. Is there a role for intravenous subdissociative-dose ketamine administered as an adjunct to opioids or as a single agent for acute pain management in the emergency department? J Emerg Med. 2016;51(6):752-757. doi:10.1016/j.jemermed.2016.07.087
- Cohen L, Athaide V, Wickham ME, et al. The effect of ketamine on intracranial and cerebral perfusion pressure and health outcomes: a systematic review. Ann Emerg Med. 2015;65(1):43-51.e2. doi:10.1016/j.annemergmed.2014.06.018
Sunny Bang, MD
Resident Physician PGY-2
Department of Emergency Medicine
Loma Linda University Medical Center


