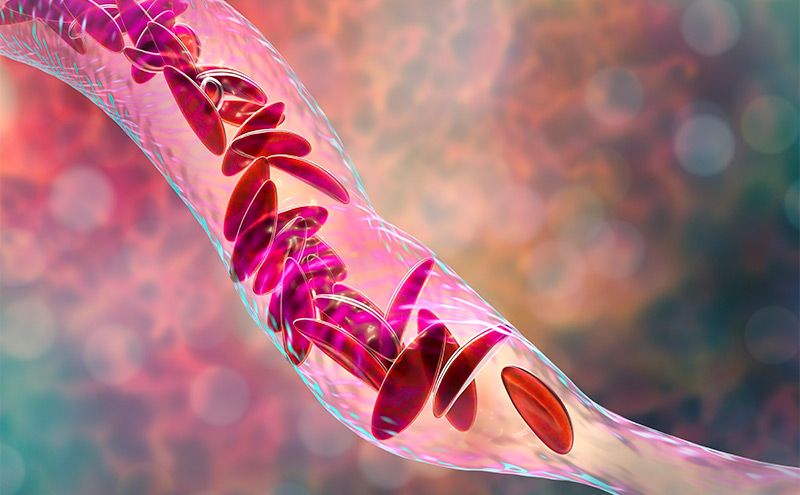
Low-Dose Ketamine for Pediatric Sickle Cell Pain Crisis
An eight-year-old male presented to the emergency department (ED) with his mother for left leg pain consistent with his prior sickle cell pain crises episodes. He had first presented two days earlier with the same. Labs and imaging were unremarkable at the initial visit. He was treated with acetaminophen, morphine, and fluids, then discharged home with his mother. The patient's mother continued to treat him with PO morphine between visits but was unable to provide adequate analgesia at home. Upon representation, he was in notable distress, tachycardic, and complained of ongoing left thigh pain with limited ability to ambulate. There was no history of trauma. He initially reported 8/10 pain. Doses of fentanyl and morphine provided some relief, but he continued to be tachycardic and appeared uncomfortable. He was subsequently treated with sub-dissociative ketamine (0.3mg/kg IV over 15 minutes). After 30 minutes, his tachycardia resolved, his pain reduced to 2/10, and he actually fell asleep. Later, he was able to ambulate in the ED and was discharged home with his mother. There were no additional ED visits related to this pain crisis episode.
The use of ketamine to treat acute pain in adult patients has widely been studied yet remains relatively unchartered for pediatric patients. Research on its use for the treatment of pediatric sickle cell pain crises is even further lacking. The little amount of published material on the topic, however, does show promise. One case series demonstrated clinically significant pain control, as well as a significant reduction in opiate usage after treatment with ketamine.1 A second case series demonstrated the same but was confounded by the use of midazolam.2 Another group showed a lower rate of treatment failure with ketamine compared to opiates.3
Early signs point to ketamine’s potential to become the mainstay of treatment for pediatric sickle cell pain crisis. While more rigorous, peer-reviewed evidence is certainly needed, clinicians can and should begin to look to ketamine in lieu of opiates when treating pediatric sickle cell pain crises. Unfortunately, uniform dosing regimens have not been established. Some of the aforementioned studies included bolus dosing (0.25-1 mg/kv IV) prior to initiation of an infusion that can be used to infer dosing. ACEP’s clinical policy on sub-dissociative dosing of ketamine for analgesia (0.1-0.3 mg/kv IV) can also be used to infer dosing, although care should be taken as this was created for use in adult populations.4 Pairing these with studies that offer information on how to mitigate adverse effects while administering ketamine can provide a starting point for determining a universal dosing regimen.5 For now, low-dose ketamine (0.1-0.3 mg/kg IV over 15 minutes) seems like a safe starting point to treat pediatric sickle cell pain crisis, as it falls well below ketamine dosing for procedural sedation (1-2 mg/kg IV).
References
- Zempsky W, Loiselle K, Corsi J, et al. Use of low-dose ketamine infusion for pediatric patients with sickle cell disease-related pain: A case series. Clin J Pain. 2010 Feb;26(2):163-67. doi: 10.1097/AJP.0b013e3181b511ab.
- Tawfic QA, Faris AS, Kausalya R. The role of a low-dose ketamine-midazolam regimen in the management of severe painful crisis in patients with sickle cell disease. J Pain Symptom Manage. 2014;47(2):334-340. doi:10.1016/j.jpainsymman.2013.03.012.
- Lubega FA, DeSilva MS, Munube D, et al. Low dose ketamine versus morphine for acute severe vaso occlusive pain in children: a randomized controlled trial. Scand J Pain. 2018;18(1):19-27. doi:10.1515/sjpain-2017-0140.
- American College of Emergency Physicians. “Sub-Dissociative Dose Ketamine for Analgesia.” Policy Resource and Education Paper. Approved March 2019.
- Motov S, Mai M, Pushkar I, et al. A prospective randomized, double-dummy trial comparing intravenous push dose of low dose ketamine to short infusion of low dose ketamine for treatment of moderate to severe pain in the emergency department. Am J Emerg Med. 2017 Aug;35(8):1095-1100. doi: 10.1016/j.ajem.2017.03.004. Epub 2017 Mar 3.
Shehzad Muhamed, MD
Attending Physician
Georgia Emergency Department Services
Northeast Georgia Health System