Creation of an Observation Visit Outcomes Database using the Clinical Emergency Data Registry (CEDR)
Greetings section members! Recently, our section voted for this year’s ACEP section grant topics, here are the results:
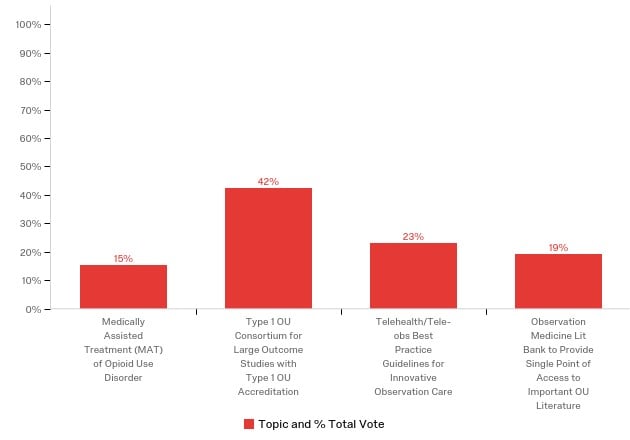
As you can see, our members selected the creation of a type 1 OU consortium for large outcome studies with type 1 OU accreditation as the topic for this year’s ACEP section grant topic. Thank you to all who took the time to consider these important initiatives and vote.
Currently, there are no universal requirements for hospitals in the United States to report outcomes related to patients cared for with observation services. Creation of a registry for observation stays would allow members of the ACEP observation medicine section, the largest society related to this type of care, to measure and benchmark clinical outcomes of observation care on a national level. Health care systems opting to participate with the registry would share their outcomes with the registry and in exchange, be allowed to compare their outcomes to other participating centers. Additionally, health care systems would have the option to collaborate with other centers who are experiencing more favorable outcomes to share best practices and improve the value of their care.
Our leadership team identified the existing ACEP Clinical Emergency Data Registry (CEDR) as an initial option for Emergency Department Observation Unit (EDOU) clinical outcomes reporting. The CEDR group is excited to partner with our section on this and we believe there is an opportunity to leverage the existing infrastructure to create an EDOU reporting interface. Initially, the ACEP observation medicine section and CEDR would pilot use of the registry at several select health systems and then scale and refine the project based on lessons learned.
Ultimately, the collaboration could include recommendations to CMS regarding benchmarking and quality reporting related to observation care. Additionally, a large data set could provide an opportunity for multicenter collaboration in quality improvement and research projects related to observation care, which is a significant limitation of existing national data registries.
The objectives of this project are three-fold. The first is to take initial steps towards defining, measuring and ultimately improving the value of observation care through the acquisition of grant support and recruitment of resources to create an observation outcomes registry. The second is to measure and compare patient level outcomes on a national level in collaboration with an existing (CEDR) platform to leverage available resources and expertise. The third is to place the ACEP observation medicine section in a position to drive quality improvement related to patient care and make further recommendations to CMS regarding value-based care provided by emergency department observation care.
Existing, large-scale clinical data sets are limited by their inability to distinguish outcomes related to patients in observation status versus those receiving observation care. Observation status is a simple billing distinction and does not signify any difference in the delivery model of care, whereas observation care is a distinct health care model using evidence based, protocolized care in a geographically distinct unit. Only observation care has been demonstrated to improve the value of care for patients in need of a short-term hospitalization, whereas observation status is a billing distinction that may or may not be associated with a change in delivery such as observation care and is often a source of confusion and potential cost shifting.
Existing reporting and validation of observation care is limited to small, or single-site reports. A large database of observation stays would allow experts in observation medicine to measure and report best practices for this type of care (ie, defining and measuring quality of observation care in terms of length of stay, conversion to inpatient status, recidivism, diagnostic test utilization, adherence to medication best practice guidelines by condition such as heart failure or diabetes, fall rates, venous thromboembolism prophylaxis rates, etc.). Additionally, ACEP members starting new observation units would be able to both contribute to the database and apply the registry data to their units to improve the quality and performance of their care.
Emergency physicians are content experts in observation medicine. This project would advance that position and further develop the relationship with CMS towards improving care in this field. As emergency physicians gain more insight into the optimal care for patients in observation status, we can educate the health care industry and patients about the benefits of observation care as well as addressing concerns regarding quality of care or increased patient costs when care is not delivered according to existing ACEP published best practices.
Christopher Caspers, MD, FACEP
Chair-Elect ACEP Observation Medicine Section
Chief, Observation Medicine, NYU Langone Health System
Associate Professor, NYU School of Medicine


