I know what you’re thinking – “this isn’t my traditional Thursday morning Regs & Eggs content, so freshly delivered.” You’re correct. Instead, it’s Ryan McBride, ACEP's Congressional Affairs Director, and this is a hostile takeover lovely opportunity to share a rundown of ACEP’s legislative advocacy and accomplishments throughout 2022, especially given the mammoth $1.7 trillion year-end package that Congress managed to cobble together last week.
In a decision he certainly won’t regret, ACEP’s regulatory expert, Jeffrey Davis, has graciously given me some space on DC’s #1 health care regulatory blog (as voted on by his coworkers) to engage in some jolly cooperation and highlight the legislative side of ACEP advocacy for a little change. It brings me great pleasure to bring you the first issue of “Legs & Eggs!” (Editor’s note: absolutely not. We’ve talked about this. Please stop.)
We had some big wins, some qualified victories, and to be totally candid, some letdowns. But even still, despite what was truly a difficult and limited year, we managed to defy the odds and get many ACEP-developed, -led, and -supported priorities across the finish line – not least of which was a law named in honor of the life and legacy of emergency physician Dr. Lorna Breen. (On a personal note, as someone from a family with several physicians and health care providers and whose family has been affected by suicide, as well as someone who has the privilege of working for emergency physicians, helping see this bill into law is the thing I’m most proud of in my career.) We also managed to enact or renew several advocacy priorities from previous Leadership and Advocacy Conference (LAC) Hill days, like eliminating the “X-waiver” for buprenorphine and turning the Alternatives to Opioids (ALTO) in the Emergency Department program into a full, permanent program and increasing its funding. We also have a direct line from ACEP Council action to federal law, with the passage of the Bipartisan Medical Marijuana and Cannabidiol Research Expansion Act. More on these and other legislative efforts later.
I’m starting to feel like I say this every year, but this year was…a weird one in Congress. Sure, they’re all weird in their own way, but I want to give you a bit of a recap of why it was so for 2022. To set the stage a bit, in scenarios where one party controls the White House and both chambers of Congress, historical trends typically foreshadow less-than-ideal results for the governing party in midterm elections, resulting a shift in the balance of power. In 2022, these already-strong headwinds were exacerbated by low presidential and congressional approval ratings, poor economic indicators, and some truly brutal electoral conditions – Democrats had some very tough Senate seats to defend, and they also suffered some bitter defeats in several big redistricting battles, so all expectations were that Democrats would lose both the House and Senate by substantial margins (spoiler alert: that was not how it played out, to the surprise of most). Republicans were not exactly looking for the chance to help them out of this jam, either. For President Biden, Speaker of the House Nancy Pelosi, and Senate Majority Leader Chuck Schumer, the writing was on the wall – it was now or never if there was any chance of getting ambitious policy goals across the finish line.
Oh, and not to mention, to get anything done requires making the most of the absolute slimmest of majorities in the Senate, where a 50-50 split rests on the tie-breaking vote of the Vice President. In most cases, this amounts to not much more than a majority on paper, given that you need 60 votes to get most anything done in the Senate. Enter budget reconciliation – a special filibuster-proof procedural tool that requires only a simple majority (51 votes) to clear the Senate. So, when you have a slim majority, why wouldn’t you use this for everything, then? Well, reconciliation is one of the more arcane congressional processes, subject to unique rules and limitations on what kinds of provisions can be included – the tl;dr (too long; didn’t read) version is that only policies that directly affect revenues or spending can be included and other “extraneous” provisions cannot, and it can (generally) only be used once per fiscal year. There’s also a somewhat self-aware cheekiness to it, with things like “Byrd Baths” and “vote-a-ramas.” Above all, budget reconciliation is a good reminder that often the most powerful person in Washington is not an elected official like the President, Speaker of the House*, or any other member of Congress, but rather the humble Senate Parliamentarian who determines what provisions are in order (i.e., which ones make it or don’t make it in). In recent years, reconciliation has been used by both parties with growing frequency as a way of bypassing the Senate filibuster because getting to 60 is a tall order in a hyper-partisan environment, even if you have 60 members on your side!
At the beginning of 2022, President Biden’s “Build Back Better” agenda (BBBA) appeared to be dead on arrival after Senator Joe Manchin (D-WV) pulled his support for it in late 2021. I’m skipping a lot here so stay with me – but while legislators continued to work on other things and hold hearings on a variety of issues, rumors of Build Back Better’s death were greatly exaggerated. After persistent efforts to get Sen. Manchin on board were finally successful, from the shambling zombie BBBA that just wouldn’t die came the Inflation Reduction Act – a scaled back effort focused on addressing energy policy and climate change, reducing the deficit, prescription drug pricing reform, and tax reform, among others. Given the expansive scope and breadth of this plan, the rollercoaster of negotiations sucked up a ton of the oxygen in the room as well as valuable committee and floor time, to the detriment of other legislative priorities. All in all, it can be tough to get much done in an election year without any complicating factors, so all this reconciliation work made everything else that much harder.
Ultimately, this work wrapped up in early August – after which legislators headed home for the remainder of the August recess, returned for a few weeks in September, then recessed again to hit the campaign trail in October. After the November elections, they once again returned to Washington to begin working on clearing the decks for the end of the 117th Congress, but even then, much of that work didn’t truly begin in earnest until early/mid-December. Never letting a good deadline go to waste, Congress went right up until the very last minute and dropped a 4,155 page bill (not including explanatory/report language) weighing in at $1.7 trillion and passed it just before the recently-extended government funding deadline of December 23.
The point of sharing all this inside baseball is to highlight just how much ACEP was actually able to accomplish in a significantly compressed timeline. So, here are some of the key highlights of 2022:
Dr. Lorna Breen Health Care Provider Protection Act Becomes Law
As noted above, on March 18, 2022, President Biden signed the “Dr. Lorna Breen Health Care Provider Protection Act” into law (Public Law 117-105). This law ensures that the appropriated funding made available under the American Rescue Plan in 2021 for the grants, resources, training, national awareness campaign, and more to help address mental health and burnout for health care professionals can be carried out to its fullest extent. (This law also took a weird path – while authorizing legislation precedes appropriations, we actually got the appropriations first and then the authorizing language a year later – very atypical!)
From start to finish, ACEP was a part of the process. We worked closely with Sen. Tim Kaine (D-VA) and Rep. Susan Wild (D-PA), as well as Rep. Raja Krishnamoorthi and others, to develop this legislation named in honor of your colleague. It has been a top priority of the College to get this bill through the legislative process and across the finish line, and we succeeded. And now, we continue working with our champions to ensure additional funding can go to help address the stress, burnout, and other mental health needs for emergency physicians and other health care providers.
Medicare Cuts
First, as Regs & Eggs detailed in November and as many of you know, the Centers for Medicare & Medicaid Services (CMS) calendar year (CY) 2023 Medicare Physician Fee Schedule (PFS) final regulation cemented a cut to the PFS conversion factor of about 4.5 percent. Additionally, thanks to some previously enacted laws and additional reconciliation work, congressional rules required a statutory “Pay-As-You-Go” (PAYGO) sequester of 4 percent. And on top of all of this is the 2 percent sequester that was fully phased back in this year after a temporary reprieve during the height of the COVID-19 pandemic. All in all, this meant physicians and other Medicare providers faced a 10.5 percent cut heading into 2023.
ACEP, other physician specialties, non-physician provider groups, and others worked from the beginning of the year to urge Congress to fully prevent this cut. In the year-end omnibus (“omni”) appropriations package, the Consolidated Appropriations Act, 2023 (CAA), Congress provided a 2.5 percent infusion for the conversion factor cut for CY 2023, and 1.25 percent for 2024, as well as two years of PAYGO relief (additionally, legislators have made it clear that the 2 percent sequester is unfortunately back to stay after that temporary reprieve). There’s no getting around it – this is obviously less than we wanted and less than what we’d advocated for, and I know it’s tough to swallow the notion that “well, it could’ve been worse” as consolation.
Here’s a breakout of the PFS conversion factor in 2023:
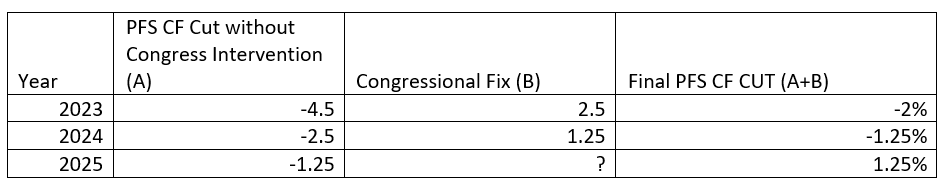
The new conversion factor for CY 2023 will be around 33.89, a 2 percent cut from the 2022 conversion factor of 34.61. This is just an estimate, as CMS has yet to calculate the revised conversion factor.
Beyond the very real impact of these cuts, the larger problem we (the physician and provider community) have is that not only do these now-annual battles detract from our ability to focus on other important advocacy priorities, but they also strain our relationships on Capitol Hill. It reminds legislators of the yearly (and costly) battles over the Sustainable Growth Rate (SGR) formula cuts that we thought we’d all fixed with the passage of the Medicare Access and CHIP Reauthorization Act (MACRA) back in 2015. Congress simply doesn’t have much appetite anymore to spend billions of dollars every year for something many of them view as CMS’ problem. So, we’re left with outcomes like this, where we’re unsatisfied because we’re dealing with payment cuts, and Congress is frustrated because they feel like they did as much as they could to mitigate the majority of the cuts but the physician and provider community is just going to be upset that they didn’t get full relief regardless. This is not a productive, effective, or sustainable path.
Rather than deal with the annual threat of PFS cuts every year, we need long-term payment reform that provides much-needed stability by addressing Medicare’s “budget neutrality” provisions that often pit physician specialties against one another, as well as providing an inflationary update for physician payments like there are for other Medicare participants (like hospitals). We have been working in earnest to shift the narrative and effort away from short-term solutions to longer-term reform, as we detailed in our response to a MACRA request for information issued by several House members earlier this year. Reinforcing the need for stability and certainty in the Medicare physician payment system, as well as our history of good faith efforts to operate within the limitations of MACRA, will be a central part of our federal advocacy as we prepare for the upcoming 118th Congress.
X-Waiver Repeal
Also included in the omni was another longstanding ACEP priority – over the past several years, ACEP has worked to fully eliminate the burdensome and unnecessary “X-waiver” requirement for physicians who wish to prescribe buprenorphine and other medication assisted treatment (MAT) for opioid use disorder (OUD), both in terms of legislative and regulatory advocacy. The year-end package fortunately included the language of the “Mainstreaming Addiction Treatment (MAT) Act” (H.R. 1384/S. 445), finally repealing this outdated federal requirement and giving emergency physicians more tools to initiate MAT from the emergency department (ED) and get patients on the path to longer-term recovery.
You are going to have to wait a little for the X-waiver to officially go away. The Substance Abuse and Mental Health Services Administration (SAMHSA) and the Drug Enforcement Administration (DEA) are going to issue guidance shortly after the new year with more information about the removal of the x-waiver requirement—and until that time, they will continue "current procedures." In other words, until this guidance is issued (which should be shortly), physicians will still need an x-waiver to prescribe buprenorphine. So stay tuned, and we’ll let you know when this guidance is released!
There’s also a catch – and a big one. The omni included the “Medication Access and Training Expansion (MATE) Act,” which essentially re-establishes the 8-hour training requirement we’d successfully worked to remove, but now for all DEA controlled substance prescribers (Schedule II, III, IV, or V) on condition of receiving or renewing your DEA registration. If you’re boarded in addiction medicine or addiction psychiatry, have already completed 8 hours of training provided by accredited organizations, or you’ve graduated from medical school or completed residency within the preceding 5 years, you’re covered. ACEP (and others) did not support this legislation – while we are supportive of continued education, we do not support federal education requirements and believe this works counter to the purpose of the MAT Act. This new requirement does not kick in for around 6 months, and we’ll provide you with much more information before then about how you can get this training (if you haven’t already).
On the whole, I think the good outweighs the bad here, but it’s a qualified win to be sure and Jeffrey and I have some work to do here. The most significant hurdle – the separate X-waiver process itself – is gone, and hopefully this will help address some of the stigma unfairly associated with MAT and increase the number of physicians providing this lifesaving treatment.
Alternatives to Opioids (ALTO) in the Emergency Department
Another omni victory! In 2018, ACEP was successful in getting our Alternatives to Opioids (ALTO) in the Emergency Department Act signed into law as part of a larger opioid/substance use disorder legislative package (the SUPPORT Act), to help EDs across the country establish and implement their own opioid-alternative pain treatment protocols. That legislation was built from the successful ALTO program initially developed by former ACEP President Mark Rosenberg, DO, FACEP, in New Jersey.
The federal ALTO program was established as a demonstration project, and the omnibus appropriations package makes it a full permanent program, authorized for five years, AND bumps up the funding appropriated for it to a total of $8 million for fiscal year 2023.
Telehealth Extensions
We also got another two years of telehealth flexibilities as part of the omnibus—through 2024! I think this bodes well for maintaining telehealth as a permanent fixture of the health care system – there’s a recognition on the Hill that telehealth was not only a great asset during the COVID-19 pandemic, but it’s a force multiplier that extends the reach of health care providers, and it’s also been incredibly popular among patients. Telehealth is here to stay, in one form or another, but gathering more data is going to be key in our collective efforts to make it permanent. Among the policies that were extended through 2024 in the omni:
- Removing Geographic Requirements and Expanding Originating Sites for Telehealth Services
- Expanding Practitioners Eligible to Furnish Telehealth Services
- Expanding Telehealth Services for Federally Qualified Health Centers and Rural Health Clinics
- Delaying the In-Person Requirements Under Medicare for Mental Health Services Furnished Through Telehealth and Telecommunications Technology
- Allowing for the Furnishing of Audio-Only Telehealth Services
- Use of Telehealth to Conduct Face-to-Face Encounter Prior to Recertification of Eligibility for Hospice Care During Emergency Period
- Study on Telehealth and Medicare Program Integrity
Some of you may wonder what these changes mean for emergency medicine. It is great that the geographic and originating site restrictions in Medicare will continue to be waived through the end of 2024. That means you can continue providing telehealth services regardless of where you or your patient are located—in both rural and urban areas. However, the actual codes you can bill when providing telehealth services are on a different timeframe. Currently, the ED evaluation and management (E/M) services, some observation services, and the critical care services are on the list of approved Medicare telehealth services through the end of CY 2023. Since Congress extended many of the telehealth waivers for two years, we are hopeful that CMS will follow suit and keep these codes on the list of approved telehealth services through at least 2024. We will have to wait and see if CMS in fact does issue a regulation to make that change.
Pandemic Preparedness
In another direct line from ACEP advocacy to federal law, the CAA also included a number of pandemic preparedness policies, including significant pieces of the PREVENT Pandemics Act that the Senate Health, Education, Labor and Pensions Committee put together earlier this year. Since the beginning of the COVID-19 pandemic, ACEP provided substantial input and feedback on what policies and changes were needed to respond to the current pandemic and prepare for future public health emergencies, and many of our suggestions were incorporated and concerns addressed.
These include improving medical countermeasure research coordination, expanding “warm base” manufacturing capacity for medical countermeasures, strengthening and maintaining the Strategic National Stockpile and improving its transparency and supply chain flexibility, studies on how to expand domestic production of generic medicines and their APIs, and preventing PPE and medical device shortages.
ED Suicide Screening
The omni also included another one of our ACEP priorities that we advocated for alongside the Emergency Nurses Association (ENA) and others. The final product was not identical but was based on the ACEP-supported “Effective Suicide Screening and Assessment in the Emergency Department Act of 2021” (H.R.1324/S. 467). It includes provisions under Substance Abuse and Mental Health Services Administration adult suicide prevention programs to include identifying best practices to improve identification, assessment, treatment, and timely transition, as appropriate, to additional or follow up care for individuals in EDs who are at risk for suicide and enhance coordination of care for such individuals during and after discharge.
Appropriations
And some of the highlights from the appropriations side of the omnibus:
- BARDA: $950 million to support advanced research and development of medical countermeasures at the Biomedical Advanced Research and Development Authority (BARDA) an increase of $205 million
- Strategic National Stockpile: $965 million for the Strategic National Stockpile, an increase of $120 million
- Flu Preparedness: $335 million for pandemic influenza preparedness, an increase of $35 million.
- EMS Preparedness and Response Workforce Shortage: urges Administration for Strategic Preparedness and Response (ASPR) to address the crippling EMS workforce shortage, including in underserved, rural, and tribal areas and/or address health disparities related to accessing prehospital ground ambulance health care services, including critical care transport.
- Traumatic Brain Injury: $8.25 million ($1m increase from FY22 levels to initiate concussion surveillance, particularly among children and youth).
- Suicide Prevention: $28.2 million, but also directs CDC to develop a plan for integrating its Emergency Department Surveillance of Nonfatal Suicide Related Outcomes pilot to collect real-time data on non-fatal suicide related outcomes and self-harm behavior into the program.
- 9-8-8 Suicide Lifeline: $439.6 million for the 9-8-8 Suicide Lifeline (additional funding to the $62 million provided in P.L. 117-180)
- Elderly falls: $3.05m ($1m increase)
- Alternatives to Opioids (ALTO) in the Emergency Department: $8 million (a $2m increase from FY22 levels)
- MISSION ZERO: $4m for this program for civilian trauma centers to incorporate military trauma care providers and maintain readiness. $2m increase from FY22 levels.
- CAROL Act: Provides $20m for valvular heart disease research (this was an ACEP-supported bill that just passed Congress and is set to be signed by the President soon).
- Firearms Research Funding: Provides $25m for firearms injury prevention and safety research through NIH and CDC.
- $12.5m for CDC (flat funding)
- $12.5m for NIH (flat funding)
- $1m for NIJ firearms violence prevention research (new)
- Emergency Medical Services for Children (EMSC): $24.134m ($2m increase)
- Poison Control Centers: $26.846m ($2m increase)
I know this is a ton of information already, and there’s still a lot more that was included like additional mental health provisions that could probably use their own update, but I really wanted to hit some of the big highlights and how they directly relate to ACEP advocacy. There are also other things that didn’t make it this year that will continue to be part of our federal efforts in the next Congress – things like workplace violence legislation, prior authorization, due process protections, and especially addressing the nation’s ED boarding and crowding crisis.
One thing that really stands out to me in all of this is how the intrinsic adaptability of emergency physicians translates to ACEP’s advocacy. I think we’re unique in our ability to fit in to a wide variety of legislative efforts and have proven to capitalize on even the most limited of opportunities, and the nature of your work opens a lot of doors on Capitol Hill. That’s a good thing, because we’ve got a lot of work to do in 2023.
Anyhow, thanks again to Jeffrey for giving me the keys to the castle for a day (it was your idea – don’t blame me) and your regularly scheduled, eagerly anticipated, and freshly delivered Regs & Eggs will return in the new year.
*Yes, I know the Speaker of the House technically doesn’t have to be a Member of Congress, but I maintain that the idea of a non-Representative Speaker is pure fantasy, folks. House members are not going to let some random unelected individual control the House, no matter how much the Fourth Estate thinkpieces/op-eds might hope. I’ll eat my hat during the ACEP23 kickoff if that happens.**
**I will not actually eat my hat.
Until next year, this is Ryan (and Jeffrey) saying, enjoy reading your legislation (and regs) with eggs!






