ACEP ID:
- My Account
- My CME
- Sign Out
ACEP ID:
June 17, 2011
ACEP Weighs in on Accountable Care Organizations (ACO) Proposals
ACEP cited numerous concerns with two rules on Accountable Care Organizations (ACOs) proposed by the Centers for Medicare and Medicaid Services (CMS) and the Federal Trade Commission (FTC).
In a comment letter to CMS, ACEP expressed disappointment that the bar was set too high on the investment and risk front to allow only the largest and most sophisticated systems to apply. In part, the letter urged CMS to provide broader opportunities for smaller physician-based groups, and align the rulemaking, implementation and reporting rules of the ACO, Physician Quality Reporting System (PQRS) and Electronic Health Records (EHR) incentive programs.
The comment letter also called for parity between Medicare Advantage Plans and fee-for-service plans. ACEP urged CMS to give ACOs the same flexibility under the 3-day rule extended to Medicare Advantage plans that allows Medicare patients to be admitted to a skilled nursing facility (SNF) without having to first meet a 3-day inpatient stay.
Another letter to the Federal Trade Commission pointed out what may be unintended consequences of the Proposed Statement of Anti-Trust Enforcement Policy regarding ACOs. In particular, the decline of emergency departments in non-rural areas could result in remaining EDs tripping the market share threshold and triggering a lengthy and expensive anti-trust assessment. Additionally, the letter explains that because emergency services are provided to everyone, no anti-competitive issues arise.
In response to the widespread criticism, CMS has proposed two new ACO models – one that would address some of the interests and abilities of organizations that are already risk-bearing, and one that might provide up-front funding (loans) for ACO start-up costs.
Information from CMS
Other ACO Resources
Summary of the Accountable Care Organizations (ACOs) draft regualtions (Alston & Bird consultants, May 2011)
Summary of the ACO waivers of various Federal laws (Hart Health Strategies, May 2011)
Proposed Quality Measures for ACOs (Davis Wright Tremaine LLP, April 2011)
This is a short synopsis of the quality reporting requirements for ACOs. CMS sets a high bar in that ACOS must report on all 65, even in its first year. For a complete synthesis of draft rule highlights, click here.
What Are the Characteristics of a Successful Shared Savings Program? (The Commonwealth Fund, April 2011)
The ACA-Driven ACO Movement: Implications for Emergency Medicine (By Michael Gerardi, MD, FACEP; March 2011)
HHS Office of Inspector General Proposal for Waivers of Certain Federal Laws
FTC-DOJ Antitrust Policy Statement
Internal Revenue Service Guidance for Tax-exempt Organizations Seeking to Participate as ACOs
The Joint Commission Criteria for Primary Care Home Standards (Feb. 2011)
2011 Benchmarks in Accountable Care Organizations: Metrics from Early ACO Adopters (Healthcare Intelligence Network, Feb. 2011)
Is There an ACO in Your Future? (MGMA Connexion, Medical Group Management Association, Jan. 2011)
Comment Letter from MedPAC (Nov. 2010)
Technology Fundamentals for Realizing ACO Success (Medicity, Sept. 2010)
Accountable Care Organizations in California: Lessons for the National Debate on Delivery System Reform (Integrated Healthcare Association, 2010)
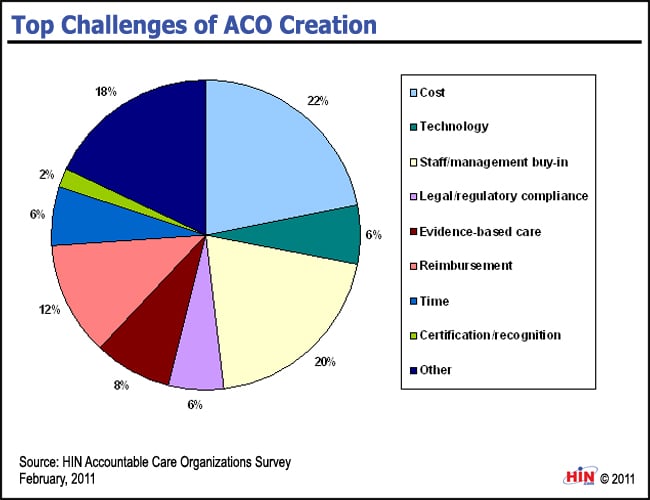
Top Challenges of ACO Creation
The February 2011 Accountable Care Organizations e-survey by the Healthcare Intelligence Network set out to assess the industry’s awareness of and readiness for ACOs.
Responses provided by 228 healthcare organizations, submitted before CMS released its proposed rule, indicate that a significant segment of the industry is reframing its care delivery structure as an ACO or will do so in the near future. According to respondents, the top five challenges of ACO creation are: