POCUS for Bladder Assessment and Volume: Technique, Tips, and Role in System-Wide Use
Amie H. Woods, MD, FACEP, Co-Chair, System Wide Clinical Ultrasound Subcommittee, Emergency Physician, INOVA Fairfax Hospital, Clinical Assistant Professor, George Washington University
Zachary P. Soucy, DO, FACEP, Co-Chair, System Wide Clinical Ultrasound Subcommittee, Assistant Professor, Emergency Medicine Director, Emergency Ultrasound Director, Emergency Ultrasound Fellowship, Co-Chair, System Wide POCUS, Dartmouth-Hitchcock Medical Center, Geisel School of Medicine, Dartmouth
Clinical Case 1
A 65-year-old male with a history of HTN, BPH, IDDM, and lumbar spinal stenosis presented to the ED with low back pain and lower extremity weakness. He denied fever, abdominal pain, and dysuria. He reports that he is able to urinate but unable to state if his urinary frequency has increased beyond “my normal prostate issues.” He notes he has fallen twice because “my legs just seem to give out on me.” On physical exam, he demonstrates 4+/5 bilateral LE strength, mild distal sensory loss, and absent patellar and Achilles reflexes. His rectal tone was equivocal. After use of a urinal, bedside POCUS was used to measure his post-void residual bladder volume:
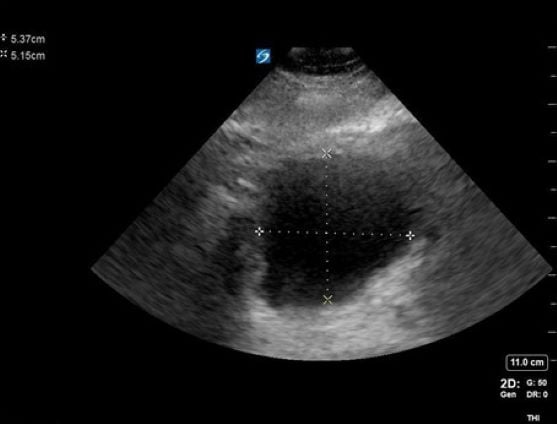
Figure 1. A cross-sectional view of the bladder with AP and transverse measurements
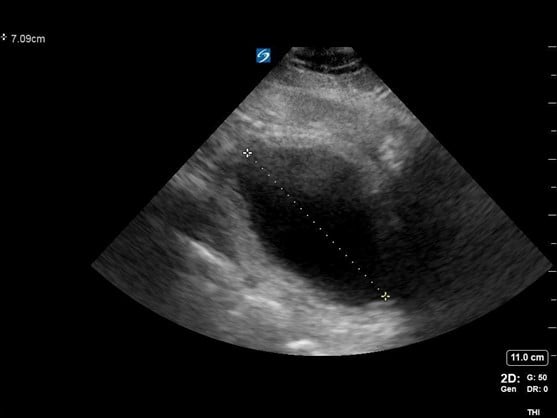
Figure 2. A sagittal view of the bladder with cranial-caudal measurement
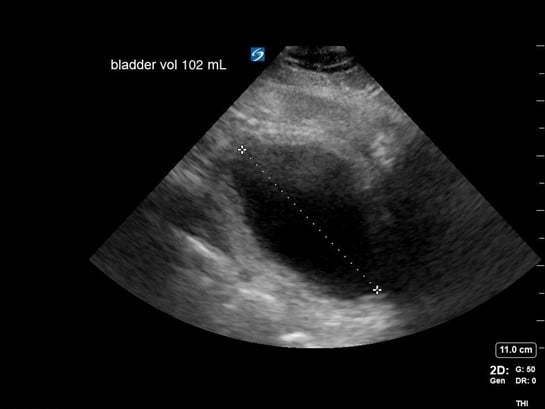
Figure 3. Calculation of bladder volume using the ellipsoid method (L x W x H x 0.52 = mL)
Discussion
Findings concerning for Cauda Equina were all present in this patient’s history, physical exam, and workup. Current literature defines normal post-void bladder volume in adults as < 50 mL in patients under 65 years of age, and < 100 mL in those older than 65. Two hundred milliliters or greater is generally regarded as the threshold for retention.1 In this case, the patient was just on the cusp of normal vs abnormal post-void urinary volume, but with his other clinical signs and symptoms, warranted emergency spine consultation and MRI. Imaging eventually showed severe compression of the spinal nerve roots by discs at the L2-3 and 3-4 levels, necessitating emergent decompression.
Clinical Case 2
A 59-year-old male with a longstanding history of BPH and urinary retention presented with a chief complaint of suprapubic abdominal pain and non-draining of his foley catheter. He stated that his catheter was changed every 8 weeks and had just been changed the prior month. On examination, his catheter was found to be obstructed with urinary sediment and clot and was removed with a plan for exchange. When the new catheter was placed and the balloon inflated, the patient reported significant pain. A POCUS image of the bladder revealed the following:
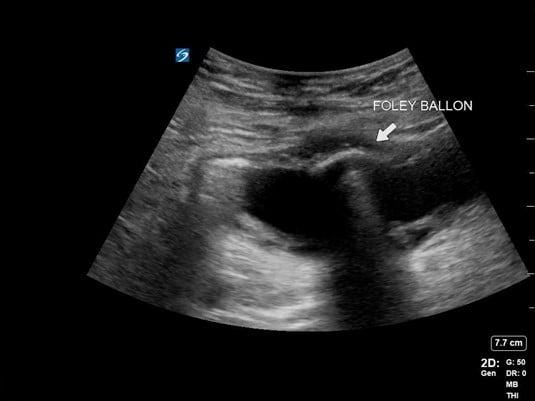
Figure 4. Image of foley balloon inside bladder
Discussion
Foley catheter insertion can be challenging in the patient with BPH. POCUS can be especially useful in identifying the location of the catheter, with the balloon creating a hypoechoic shadow artifact. When the patient’s urinalysis resulted, he was found to have a catheter-associated UTI (CAUTI) causing his pain, but the catheter was appropriately placed.
Clinical Case 3
A 73-year-old woman with a history of atrial fibrillation on Coumadin, presented to the ED with hematuria and urinary retention. She denied fever, abdominal pain, and dysuria. Examination revealed a well-appearing female patient with an unremarkable abdominal and genital exam. Bedside POCUS examination of the bladder revealed the following:
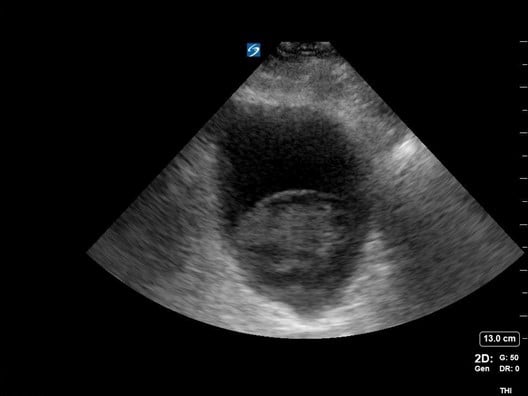
Figure 5. Bladder with large clot sitting at base
Discussion
Ultrasound images of the bladder revealed a large clot, likely spontaneous, that was causing the patient’s hematuria and contributing to obstruction of the bladder outlet. A three-way Foley catheter was inserted and the bladder was irrigated to pink-colored urine. On lab evaluation, the INR was found to be slightly supratherapeutic. Hgb and Hct levels were noted to be normal. The foley was then removed and the patient passed a trial of void in the ED and was discharged with a recommendation to hold Coumadin x 24 hrs.
Introduction, Scanning Technique and Anatomy, and Billing
With the patient in supine position, a 2- to 5-MHz curvilinear probe is placed above the patient’s symphysis pubis in the midline position. To obtain a cross-sectional view of the bladder, the probe is oriented with the marker towards the patient’s right side. Once an image is obtained, the probe can be rotated 90 degrees to orient the marker towards the patient’s head for a long or sagittal view of the bladder. Bladder volume is obtained using the ellipsoid formula of depth x width x height x 0.52 (correction factor). Normal bladder findings include a smooth wall measuring 3-5 mm, which may decrease to 2-3 mm when filled. As discussed above, normal post-void residual volume in patients < 65 yo is < 50 mL and < 100 mL in those over the age of 65. A post-void residual of > 100 should raise suspicion about a mechanical, pharmaceutical, or neurogenic cause of retention.2-7
Role for Ancillary Staff and System-Wide Program Development
As healthcare institutions increasingly recognize the role of POCUS in patient care, the target group for skill development has expanded beyond physicians and APPs. Many large health systems are implementing both ultrasound-guided peripheral IV training and bladder scanning in the clinical toolkit for nursing and other ancillary staff. Robust data exists to support the use of POCUS by both MD/APP groups, as well as nursing and clinical technician groups to reduce unnecessary catheterizations, therefore, the risk of UTIs.8 In addition, to prevent infection, the use of POCUS to assess bladder volume has been shown to aid in throughput and therefore reduce the length of stay in the ED. An assessment of female pediatric patients showed a significant decrease in time to imaging for those patients awaiting pelvic ultrasound who required a full bladder for scanning when POCUS was used to assess bladder fullness and therefore, imaging readiness.9
Coding Clarification for Imaging vs. Non-imaging in Estimate of Bladder Volume
For program leaders and those working on the coding and billing side of POCUS, it's important to know the delineation in CPT coding for bladder scanning both with and without imaging. As hospitals employ a three-dimensional volumetric probe (eg, Bladderscan), these devices calculate volume via consecutive sectional images of the bladder without direct visualization. In these cases volume may be overestimated (in the case of pelvic ascites), and may miss identification of abnormalities such as hematomas, mechanical catheter failure, and bladder masses. In these cases, the 51798 code should be used. The 76857 code should be used when a bladder image is obtained, and abnormalities are noted or sought.10
Catheter-associated UTIs (CAUTIs) as a Hospital-Acquired Condition (HAC)
The Centers for Medicare and Medicaid Services (CMS) HAC Reduction Program aims to improve patient safety and reduce or eliminate the number of complications experienced by patients during and after a hospital stay. The program applies to all acute care hospitals and calculates a composite score based on the infrequency or absence of certain known peri- and post-hospital conditions such as pressure ulcers, DVTS, and wound dehiscence. Infection reduction is an important goal of the program and includes measures to prevent events such as central line-associated bloodstream infections (CLABSIs) and catheter-associated UTIs (CAUTIs). POCUS plays a crucial role in reducing the need for indwelling Foley catheters via frequent bladder scanning and assessment for retention. These reduction tools become essential for a hospital system’s HAC score; those falling in the lowest 25% have a 1% remittance of federal reimbursement.11
References
- Nitti and Blaivas. Urinary Incontinence: Epidemiology, pathophysiology, evaluation, and management overview, 2007.
- Chan H. Noninvasive bladder volume measurement. J Neuroscience 1993;25(5):309-12.
- D'Silva KA, Dahm P, Wong, CL. Does this man with lower urinary tract symptoms have bladder outlet obstruction? The Rational Clinical Examination: a systematic review. 2014;312(5):535-42.
- Hakenberg OW, Ryall RL, Langlois SL, et al. The estimation of bladder volume by sonocytography. J Urol. 1983;130(2):249-51.
- Hvarness, H, Skjoldbye B, Jakobsen H. Urinary bladder volume measurements: comparison of three ultrasound calculation methods. Scand J Urol Nephrol. 2002;36(3):177-81.
- Teng CH, Huang YH, Kuo BJ, Bih LI. Application of portable ultrasound scanners in the measurement of post-void residual urine. J Nurs Res. 2005;13:216–224.
- Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare Infection Control Practices Advisory Committee (HICPAC). Guidelines for prevention of catheter-associated urinary tract infections 2009. 2019 [accessed 2019 Jan 25]. Available from: https://www.cdc.gov/infectioncontrol/pdf/guidelines/cauti-guidelines-H.pdf. infections 2009: mortality and costs. Infect Control Hosp Epidemiol 2011;32:101–114.
- Palese A, Buchini S, Deroma L, Barbone F. The effectiveness of the ultrasound bladder scanner in reducing urinary tract infections: a meta-analysis. J Clin Nurs. 2010 Nov;19(21-22):2970-9. doi: 10.1111/j.1365-2702.2010.03281.x. Epub 2010 Sep 8. PMID: 21040003.
- O'Brian RA, Firan A, Sheridan MJ, Kou M, Place RC, Chung CH. Bladder Point-of-Care Ultrasound: A Time Saver in the Pediatric Emergency Department. J Emerg Med. 2021 Sep;61(3):e32-e39. doi: 10.1016/j.jemermed.2021.04.010. Epub 2021 Jun 25. PMID: 34176689.
- ACEP 2012. Coding and Reimbursement Update
- CMS.gov: Hospital-Acquired Condition Reduction Program