
Tips and Tricks: Time is Testicle - Mastering the Testicular Ultrasound Exam
Acute scrotal pain makes up approximately 0.5% of all emergency department complaints.1 History and physical examination can be relatively non-specific, resulting in a broad differential diagnosis of potential etiologies. Among these, testicular torsion is the most important and time-sensitive diagnosis to make. Delay in seeking medical care or delay in diagnosis for these patients can result in significant morbidity, including infertility.2
The use of point-of-care ultrasound (POCUS) for the evaluation of patients with acute scrotal pain can be a very valuable clinical tool to facilitate more rapid diagnosis, particularly in a setting where ultrasound technologists are not available 24 hours per day. The diagnostic accuracy of POCUS for testicular torsion when performed by emergency physician is 95% sensitive and 94% specific.3 So having the skills to perform a testicular POCUS examination is extremely valuable to expedite the diagnosis and management.
Technique:
1. Prepare your patient:
Explain to the patient what to expect and be sensitive with draping during the procedure. The patient should be in a supine position with his legs separated or externally rotated at the hip (ie, frog-leg position). Use warm gel, if possible, to avoid an unintentional cremasteric reflex.4
2. Drape a towel under scrotum for support. Place the penis against the abdominal wall and cover it with a towel.
3. A high frequency linear probe (7.5-10 MHz) is the probe of choice.
4. Always start with the unaffected side to decrease discomfort and establish a baseline.
5. Scan through each scrotum and evaluate the testis, epididymis, and soft tissue in two planes (ie, sagittal and transverse).
6. Then move to the “buddy view,” which is a transverse view of both testicles in the same image. Compare both testicles echogenicity, blood flow, and size. In a testicular torsion, you should see a decrease in echogenicity on the affected side (Figure 1), while in epididymitis you will generally see normal echogenicity and enlargement of the epididymis (Figure 2). Of note, echogenicity may be normal in intermittent or early torsion cases.
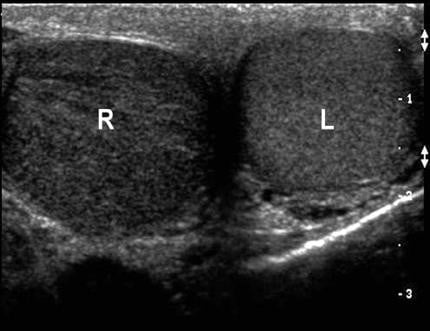
Figure 1. Left testicle normal with right testicular torsion and hypoechogenicity. Courtesy of Michael Blaivas, MD
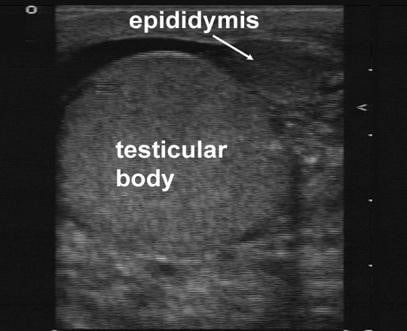
Figure 2. Enlarged Epididymis. Courtesy of Michael Blaivas, MD
7. Finally, add power Doppler to compare the pattern of flow in both testicles. Decreased flow in the affected size is suggestive of testicular torsion, while an increase in blood flow is more common in inflammatory condition as epididymitis or orchitis (Figure 3).

Figure 3. Testicular ultrasound with absence of blood flow. Courtesy of Michael Blaivas, MD
Take Home Points:
- Time is testicle. Perform a testicular POCUS examination early in the patient’s course.
- POCUS has a high sensitivity and specificity or testicular pathology.
- Ensure proper position and comfort of the patient to facilitate testicular scanning.
- Compare both testicles echogenicity and blood flow.
References:
- Blaivas M, Brannam L. Testicular Ultrasound. Emerg Med Clin North Am. 2004;22(3):723-748.
- Blaivas M, Batts M, Lambert M. Ultrasonographic diagnosis of testicular torsion by emergency physicians. Am J Emerg Med. 2000;18(2):198-200.
- Blaivas M, Sierzenski P, Lambert M. Emergency evaluation of patients presenting with acute scrotum using bedside ultrasonography. Acad Emerg Med. 2001;8(1):90-93.
- Introduction to Bedside Ultrasound. Volume 1, Chapter 10; section 2,3.
Nehal Al-Sadhan, MD
Rhode Island Hospital/Hasbro Children's Hospital



