Tips & Tricks: Supracondylar Fractures and POCUS
Elbow injuries are a common presenting complaint to the pediatric emergency department. Radiographic imaging is often obtained for evaluation of suspected fractures. Elbow fractures account for up to 15% of fractures in children with supracondylar fractures being the most common.1 Occult supracondylar fractures, those with initial normal radiographs that are later diagnosed in follow up, make up 2-18% of all the fractures seen.2 Assessment of elbow radiographs may be challenging due to the non-ossified epiphysis in children. Furthermore, in young children, clinical assessment can often be difficult and radiographs tend to be generously ordered to avoid missing potential fractures. There is a large discrepancy between the number of taken radiographs and the number of detected fractures.3
When x-ray findings are nonspecific but the clinical index of suspicion for fracture remains high, point-of-care ultrasound (POCUS) may aid in your clinical diagnosis.4 Alternatively, after minor injuries, if clinical assessment for an elbow fracture is low and POCUS examination is negative for fracture, additional radiographs may not be needed.
What to look for on ultrasound
In obvious cases, you will see direct fracture signs (ie, disruption of the cortex). However, for more subtle fractures, use POCUS to look for an elevated dorsal fat pad, caused by a joint effusion that may be an indirect sign of a fracture.5 By identifying a positive dorsal fat pad sign and/or cortical lesions of the distal humerus, Supracondylar fractures can be detected very sensitively by POCUS. One study found that for ultrasound, fracture diagnosis in comparison to radiographs had a sensitivity of 100%, a specificity of 93.5%, an NPV of 100% and PPV of 95.2%.6
How to perform the study
Probe selection: Linear probe, high frequency
Position: With the elbow bent at 90 degrees, scan along the posterior edge of the distal humerus in longitudinal and transverse axes
Key landmarks to identify: Distal humerus without cortical irregularity, olecranon, posterior fat pad
With the elbow bent at 90 degrees (Figure 1), use the linear probe in longitudinal (Figure 2) and transverse axes (Figure 3) to identify (a) distal humerus (b) olecranon (c) posterior fat pad

Figure 1: With the elbow bent at 90 degrees, use the linear probe in a longitudinal plane to identify normal ultrasound landmarks for the elbow
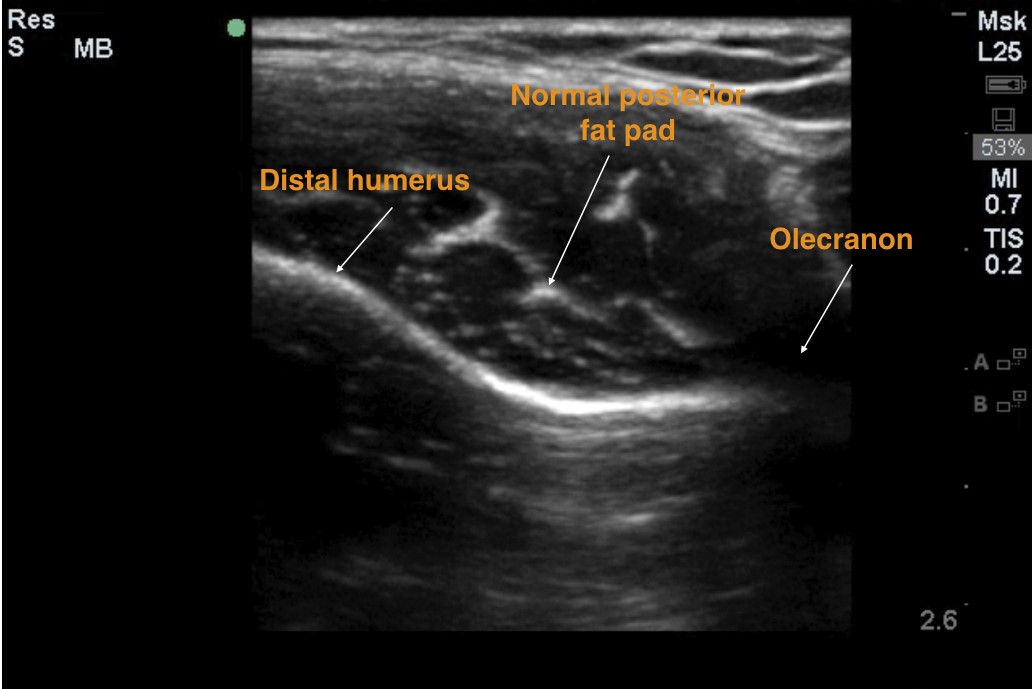
Figure 2: Longitudinal view of the distal humerus showing a normal posterior fat pad and the olecranon
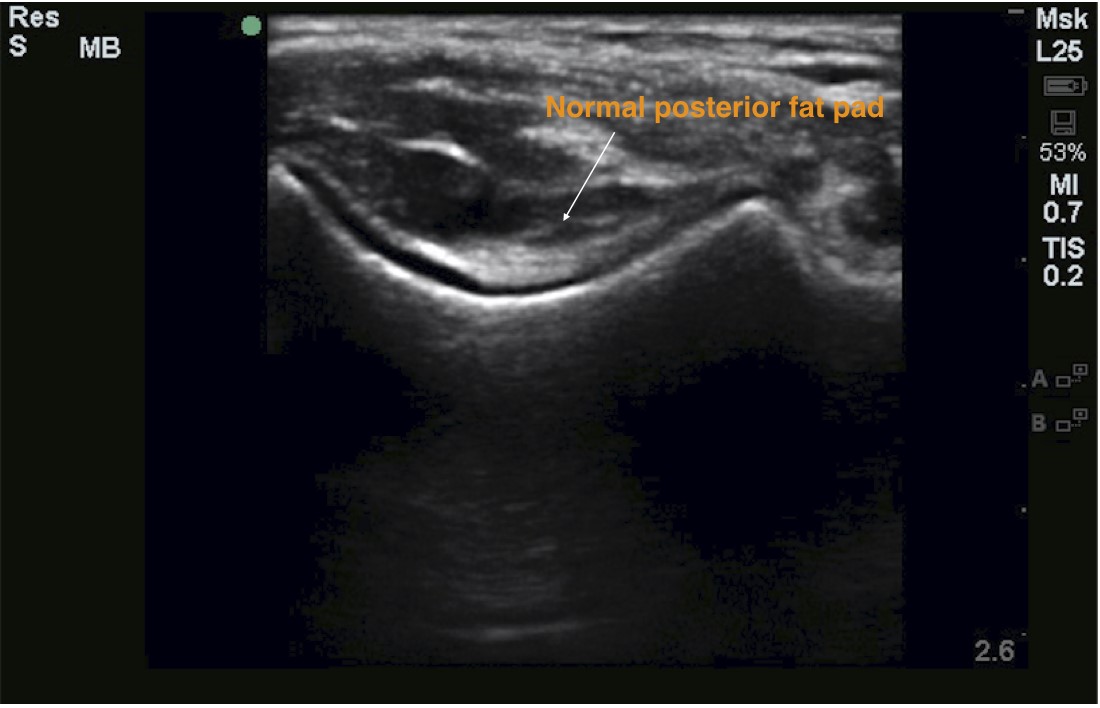
Figure 3: Transverse view of the olecranon fossa with normal posterior fat pad
Ultrasound findings of occult fracture
Bulging posterior fat pad: rise of the fat pad (Sail sign) above the extension of the distal humeral line on longitudinal view (Figure 4) or above a line connecting both lips of the olecranon fossa on transverse view (Figure 5).
Lipohemarthrosis: heterogeneous echodensity with hypoechoic areas of the posterior fat pad
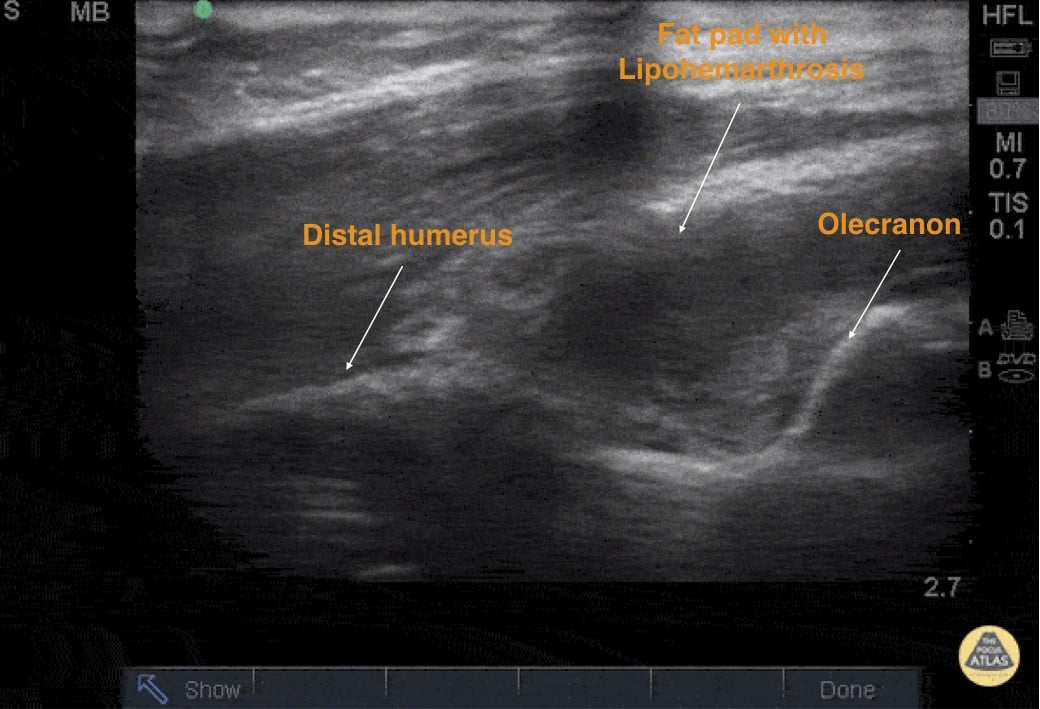
Figure 4: Longitudinal axis of the elbow depicting an area of elevated fat pad with Lipohemarthrosis (hypoechoic, with fluid) that is concerning for a supracondylar fracture. Image credit: Pocus Atlas
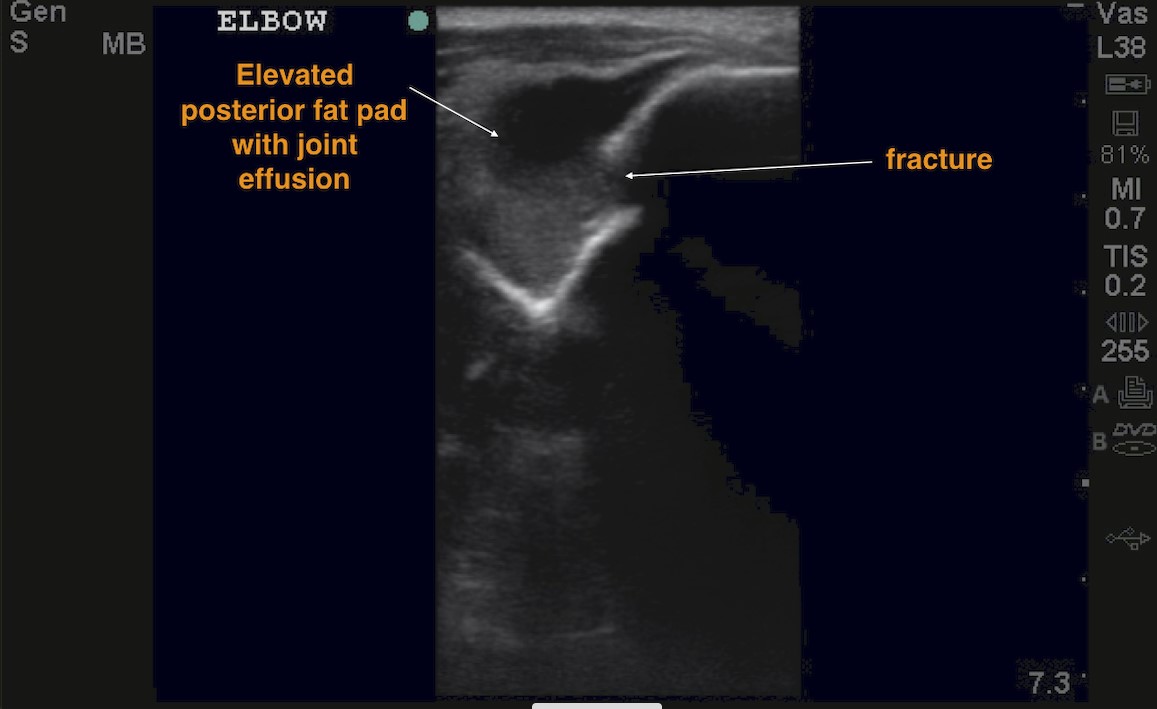
Figure 5: Transverse axis of the elbow depicting the olecranon fossa and a large joint effusion with a disruption of the cortex.
References
- Delgado J, Jaramillo D, Chauvin N. Imaging the injured pediatric athlete: upper extremity. Radiographics. 2016;36(6):1672.
- Burnier M, Buisson G, Ricard A, et al. Diagnostic value of ultrasonography in elbow trauma in children: Prospective study of 34 cases. Orthop Traumatol Surg Res. 2016;102(7):839-43.
- Alzen G, Duque-Reina D, Urhan R, et al. Radiological examinations after trauma in children: clinical and medico-legal considerations about their indications. Dtsch Med Wschr.1992;117:363-7.
- Chan W, Green-Hopkins I. Ultrasound for diagnosis of occult supracondylar fractures. Pediatrics, PEM Pearls. 2019.
- Donnelly LF, Klostermeier TT, Klosterman LA. Traumatic elbow effusions in pediatric patients: are occult fractures the rule? AJR. 1998;171:243-5.
- Eckert K, Janssen N, Ackermann O, et al. Ultrasound diagnosis of supracondylar fractures in children. Eur J Trauma Emerg Surg. 2014 Apr;40(2):159-68.
Zahra Ghazi-Askar, MD and Viveta Lobo, MD
Stanford University