Journal Club: Jugular Venous Compliance to Assess Decompensated Heart Failure
Journal Article
Simon MA, Schnatz RG, Romeo JD, et al. Bedside ultrasound assessment of jugular venous compliance as a potential point-of-care method to predict acute decompensated heart failure 30-day readmission. J Am Heart Assoc. 2018 Aug 7;7(15):e008184.
Acute decompensated heart failure (ADHF) is one of the most common reasons for admission to the hospital and is increasing in prevalence. Patients presenting with ADHF who cannot be discharged are either admitted to inpatient or to an observational unit. The appropriate unit is determined by the ED physician based on clinical gestalt, consisting of history and physical exam, as well as laboratory values and radiological studies such as BNP and chest x-ray. However, none of these parameters has been shown to be predictive of length of stay, which is one of the primary concerns that the ED physician has to anticipate when deciding on disposition. Unnecessary admissions to the hospital increase cost over an observation admission, and an observation admission for a patient who will need a prolonged length of stay can delay definitive care and use up a resource that can be better suited for patients requiring a less than 24 hour stay.
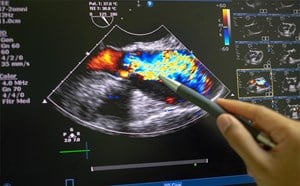
The study authors employ a novel POCUS technique to predict a patient length of stay on a patient admitted for ADHF. The authors measured the RIJV (Right internal jugular vein) in short axis at end expiration and determined the cross-sectional areas (CSA). They then had the patient perform a valsalva maneuver, where the patient expired forcefully into a manometer to generate a pressure of at least 40 mmhg and remeasured the CSA. The authors postulated that in patients with higher right atrial pressures (RAP) there would be less change with valsalva as compared to patients with lower RAP. This was based on previous work by the authors where these measurements were done in patients getting right heart catheterization and objective measurements of RAP. The authors hypothesized that patients with higher RAP would have a longer LOS than patients without and would be more likely to be readmitted within 30 days. The authors performed a RIJV POCUS on day 1 of admission and a “discharge” RIJV POCUS when the patient transitioned from intravenous to oral diuretics. Additionally, if any right heart catheterization was planned, the authors performed a RIJV POCUS prior to catheterization. The authors defined a positive study as one with less than 66% change in RIJV CSA. After exclusions, such as patients on inotropes, they analyzed 157 patients. They found overall that this cutoff had a sensitivity of 75% and specificity of 77% at predicting elevated RAP. Results were similar for both reduced ejection fraction and preserved ejection fraction group. Most importantly, they found that patients with a normal RIJV POCUS had a 91% predictive value of avoiding 30 day readmissions and those with positive RIJV POCUS were more than twice as likely to be readmitted within 30 days (Hazard ratio 5.2).
Admissions for ADHF has been increasingly scrutinized by both payors, both private and governmental. There are severe financial repercussions for all involved, with penalties being placed on hospitals for patients readmitted for ADHF, including non-payment. This study demonstrates a simple and reproducible technique to predict readiness for discharge. While other POCUS techniques such as tissue doppler, spectral doppler, tricuspid annular plane systolic excursion (TAPSE) and measures of diastolic dysfunction are used for similar purposes, this technique is simple and easy to perform by even the most novice POCUS users. While it only performs moderately well at predicting RAP, in the patient and hospital-oriented predictor of readiness for discharge, it performs extremely well. It could conceivably be performed when the patient is being considered for discharge from the observation unit or the ED. With a <66% change in CSA with Valsalva, the physician may re-evaluate plans for discharge. While not addressed in this study, future studies could have patients receiving a RIJV POCUS in the ED to determine which patients to admit to the hospital and which patients to place in observation. When in the observation unit, daily measurements could be performed to determine readiness for discharge.
Joshua Guttman, MD
Emory University School of Medicine